ABSTRACT
This research aims to study the findings from diagnostic laparoscopy among infertile women managed in a secondary healthcare center in Nigeria. This is a prospective study of eighty infertile women who had diagnostic laparoscopy in a secondary healthcare facility in Nigeria. The age range of the women was 24 to 45 years with most of them belonging to the parity group of 0 to 1 (90.0%; n=0.72). Primary infertility accounted for 43(53.8%) of cases, whereas the mean duration of infertility was 4.3+/- 2.4 years. Fifty-seven (71.3%) of the women had abnormal findings at laparoscopy. This comprised mainly of tubal pathologies (63.8%, n=51), pelvic adhesions (33.8%, n=27) and uterine fibroids (31.3%, n=25). Tubal occlusion was found in 39(48.8%) of the women, compromised bilateral tubal occlusion in 12(15.0%) and unilateral tubal occlusion in 27(33.8%) of cases. Distal tubal occlusion accounted for 24(30.0%) while proximal tubal occlusion was seen in 15(18.8%) of cases. While there were 21(26.3%) cases of polycystic ovaries, there was no significant difference in prevalence of abnormal laparoscopy (p=0.8), tubal pathology (p=0.5) and tubal occlusion (p=0.18) with respect to the type of infertility. There was a high rate of abnormal laparoscopy findings among the studied women which were mainly tubal occlusion and pelvic adhesions. These findings indicate the need to incorporate laparoscopy in the initial evaluation of all infertility cases in our environment.
Key words: Abnormal laparoscopy findings, Nigerian infertile women, Nnewi secondary health care centre.
Infertility, which refers to the inability of a couple to conceive after one year of regular unprotected sexual intercourse, is the commonest indication for outpatient gynaecological consultation in Nigeria (Adeyemi et al., 2009; Obuna et al., 2012; Orhue and Aziken, 2008; Ikechebelu, 2005; Karshima et al., 2014). The aetiological factors include tuboperitoneal diseases, anovulation, uterine lesions and semen fluid abnormalities (Adeyemi et al., 2009; Obuna et al., 2012; Orhue and Aziken, 2008).
The structural and functional integrity of the fallopian tubes are crucial to successful fertilization and subsequent implantation of the embryo. The tubes serve
to nourish, and also aids subsequent interaction of the sperm cells and the released egg. They provide the immediate environment for fertilization and subsequent travel of the conceptus to the uterus for implantation.
Tubal factor infertility, likely congenital or acquired, results from either unilateral or bilateral tubal obstruction. Congenital causes include tubal stenosis, absent tube and other mullerian duct anomalies. The acquired causes could be endoluminal, such as those caused by pelvic inflammatory diseases/sexually transmitted diseases, post abortion sepsis or puerperal sepsis. It can also be exoluminal, commonly caused by pelvic peritoneal adhesion bands and endometriosis.
The prevalence of tubal infertility varies across the regions depending on the prevalence of the risk factors. It may also depend on which modality of evaluation is utilized in the diagnosis. Both hysterosalpingogram (HSG) and laparoscopy and dye test can be utilized in the evaluation of tubal factor infertility. However, laparoscopy remains the gold standard for detection of tuboperitoneal pathologies as it has a better diagnostic yield than HSG (Tvarijonaviciene and Nadisauskiene, 2008). Diagnostic laparoscopy enables inspection of the peritoneal cavity, evaluation of tubal patency as well as examination of the adnexal structures.
Additionally, it also enables the surgical treatment of the identified lesions in order to improve reproductive outcome. These lesions include proximal tubal occlusions, polycystic ovaries, peritoneal adhesions and uterine fibroids. The setback in the use of laparoscopy especially in the resource constrained areas of the world necessitates the need for skill and facilities.
In Nigeria, the main modality of tubal factor evaluation in Nigeria remains HSG with varying rates of tubal abnormalities (Imo and Sunday-Adeoye, 2008; Adesiyun et al., 2008; Ibekwe et al., 2010; Bukar et al., 2011; Bello 2006).
In a review of the pattern of HSG findings among 320 infertile women in Nnewi, Southeast Nigeria, Okafor et al. (2010) reported a prevalence rate of 43.5% among the women. They found bilateral tubal occlusion in 18.7% of the women. Similarly, Imo and Sunday-Adeoye (2008) reported a prevalence of 54.6% among infertile women who had HSG in a tertiary healthcare center in Abakiliki, Southeast Nigeria.
Also, among the earlier report was that of Adesiyun et al. (2008) in 2008 who reported a bilateral tubal occlusion rate of 67.2% of the women which were mainly distal tubal occlusion.
Elsewhere in Addis Ababa, Ethiopia, Kitilla (2010) reported a 31.0% prevalence rate of bilateral tubal occlusion among 8582 women, 60% of whom experienced distal tubal occlusion. In Nigeria, the findings of tubal pathologies follow similar pattern.
One of the few reports on laparoscopy findings among infertile women is that of Ikechebelu and Mbamalu (2010). They reviewed 253 cases of laparoscopy and dye test done among infertile women in a private specialist hospital and reported 60.4% prevalence rate of tubal pathologies comprising mainly of bilateral tubal occlusion in 38.3% and unilateral tubal occlusion in 22.1% of cases. Pelvic adhesions were found in 42.7% of the women.
Much earlier in Ibadan, Otolorin et al. (1987) had reviewed 218 laparoscopies done for infertility and reported a rate of 35.3% of bilateral tubal occlusion and 9.6% of unilateral tubal occlusion. They noted pelvic adhesions in 55.1% of the women. Uterine fibroids were present in 26.6% of the cases. Their account was similar to that of Odusoga et al. (2002) who reviewed the findings at laparoscopy among 215 women being managed in a tertiary healthcare institution in Sagamu, Southwest Nigeria. They reported tubal occlusion in 31.6% of the women and pelvic adhesions in 74.9% of cases. They advocated for the incorporation of laparoscopy as a first line investigative tool in management of infertility in the region.
In Nigeria, mission hospitals play a significant role in reproductive health service delivery system because they are often located closer to the people and are normally better managed because most of them are privately owned. Patients who visit these centers report that the staffs are friendlier than those at the government owned institutions (Nwosu et al., 2012).
However, endoscopy in a secondary healthcare centre can be challenging on the basis of need for personnel and equipment especially in a resource poor setting. These include anaesthetic and nursing support services. This study reported on the laparoscopy findings among the infertile women managed in a missionary secondary healthcare center in Nigeria.
Aim and objectives
This research examines the abnormal laparoscopy findings among infertile women managed at Holy Trinity Specialist Hospital, Onitsha, Nigeria in relation to the type of infertility based on the following objectives
1. To study the sociodemographic and clinical characteristics of the women.
2. To determine the rate and pattern of abnormal laparoscopy findings among the women.
3. To determine the association of abnormal laparoscopy findings with the type of infertility.
4. To make recommendations on the use of laparoscopy in the evaluation of female infertility in Nigeria.
Hypothesis
There is a high rate of tubal abnormalities which has no relationship with the type of infertility common among infertile women attending a missionary hospital in Onitsha.
Outcome measures
1. The rate and types of abnormal laparoscopy findings among the women.
2. The relationship of abnormal hysteroscopies to the type of infertility among the women.
Study setting
Holy Trinity Specialist Hospital and Maternity is a big missionary hospital located in the commercial city of Onitsha. It is a secondary health care center that also offers specialist services. The hospital employed the services of three gynecologists who run the obstetric and gynaecological services of the hospital. The gynaecological endoscopy unit of the hospital is managed by a trained gynaecological endoscopist. Hysteroscopy and laparoscopy services are offered to the patients as indicated.
Study design
This is a prospective study of the first eighty infertile women who had diagnostic laparoscopy at the Gynaecological Endoscopy Unit, Holy Rosary Specialist Hospital, Onitsha, Anambra State, between 1st November, 2015 and 30th April, 2017.
Study population
Consecutive infertile women who presented at the Fertility and Gynaecology Endoscopy Unit, Holy Rosary Specialist Hospital, Onitsha, Anambra State, Nigeria for management within the study period and gave consent to the study were recruited. Those who withheld consent were excluded from the study.
At presentation, a proforma was used to collect data on all the infertile women who presented for management. The information obtained includes the biosocial data, the presenting complaint, menstrual pattern and reproductive performance.
Following clinical evaluation including transvaginal scan and in some cases, hysterosalpingogram, the patients were scheduled for diagnostic laparoscopy. General anaesthesia with endotracheal intubation and positive pressure ventilation was used in all cases. The procedures were done in the immediate post menstrual phase because diagnostic hysteroscopy was performed at the same setting.
Following general anaesthesia, diagnostic hysteroscopy and introduction of the dye injector into the uterus was done. Laparoscopy was started with veress needle insufflation and primary port insertion at the supraumbilical region. The peritoneal cavity was then surveyed systematically to include the pelvis, paracolic gutters, liver, undersurface of the diaphragm as well as the spleen and stomach. The head of the patient was then tilted downwards to allow the guts fall away from the pelvis so as to obtain a clear vision of the pelvic cavity and the organs at maximal uterine anteversion by the vaginal assistant.
The pelvis was then examined closely starting from the uterus, the right adnexum, left adnexum, the pouch of Douglas and the anterior pouch. Any identified lesions were documented and described. Some lesions such as polycystic ovaries and pelvic adhesions were also addressed at the same time. If visualization is impaired by adhesions, a secondary port was inserted for further manipulation. Dye injection was achieved with 50-ml syringe while both ostia were observed for spillage of dye. Irrigation and suctioning were done at the end of the procedure, when indicated.
At the end of the procedure, desufflation was achieved by opening the port valves in which secondary ports were then removed under vision followed by the removal of the primary port. The port sites were sutured with Vicryl 2.0 (subcuticular). Postoperatively, the patients were given antibiotics and discharged home the same day with follow-up at the clinic in a week’s time. The designed proforma were then completed with the findings at laparoscopy and the operative details including duration of the procedure, challenges and complications encountered were also documented.
Data analysis
Data was analyzed with Stata version 12.1. The mean, median and modes were calculated for the continuous variables while percentages were calculated for the composite variables. Pearson’s Chi square was used to determine the relationship between abnormal laparoscopy findings and the type of infertility. A p-value of less than 0.05 at a confidence interval of 95% was taken as significant. The data is presented in tables.
Ethical clearance
Ethical clearance was obtained from the Institutions’ ethical board and the ethical principles of non-maleficence, beneficence, confidentiality and respect of persons were applied throughout the duration of the study. The patients were well counseled on the purpose of the study and they all gave consent. Those who withheld consent were excluded from the study.
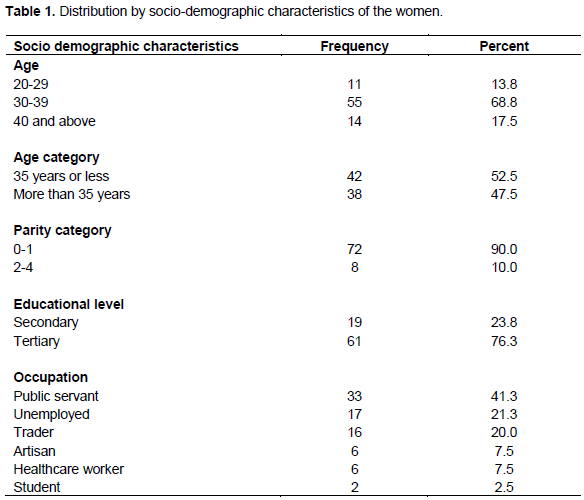
Table 1 shows the socio-demographic characteristics of the eighty women that were studied. The age of the women ranged from 24 to 45 years with a mean of 34.9 +/- 5.9 years. The modal age group was 30 to 39 (68.8%, n=55) with most of the women belonging to the parity group of 0 to 1 (90.0%; n=0.72). Majority of the women were public servants (413%; n=33) and those that had acquired tertiary education (76.3%; n=61).
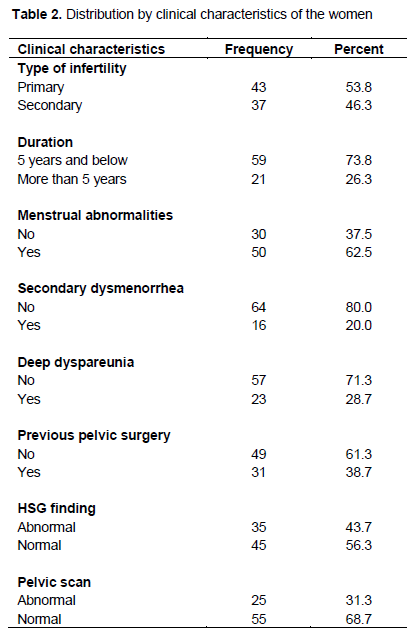
The mean age of menarche was 13.4+/- 1.7 years. Primary infertility accounted for 43(53.8%) of cases. The duration of infertility ranged from 1 to 10 years with a mean of 4.3+/- 2.4 years. Fifty (62.5%) of the women presented with menstrual abnormality while 16(20.0%) had a history of secondary dysmenorrhea. Thirty-one (38.8%) of the women had undergone a pelvic surgery in the past (Table 2).
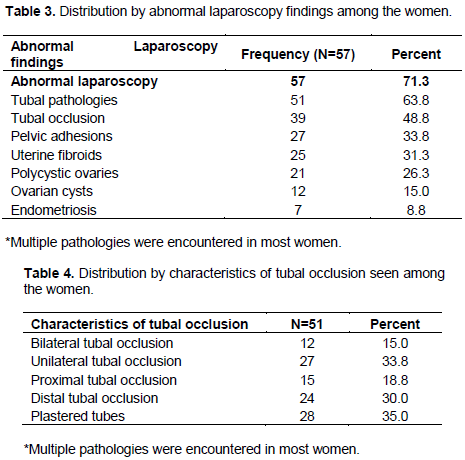
Table 3 shows the prevalence and pattern of abnormal laparoscopy findings among the women. Fifty-seven (71.3%) of the women had abnormal findings at hysteroscopy. This comprised mainly of tubal pathologies (63.8%, n=51), tubal occlusion 39(48.8%), pelvic adhesions (33.8%, n=27) uterine fibroids (31.3%, n=25) and polycystic ovaries (26.3%, n= 21). Endometriosis was seen in 7(8.8%) of the women.
Table 4 showed tubal occlusion, compromised bilateral tubal occlusion in 12(15.0%) and unilateral tubal occlusion in 27(33.8%) of cases. Distal tubal occlusion accounted for 24(30.0%) of all cases of tubal occlusion while proximal tubal occlusion was seen in 15(18.8%) of cases.
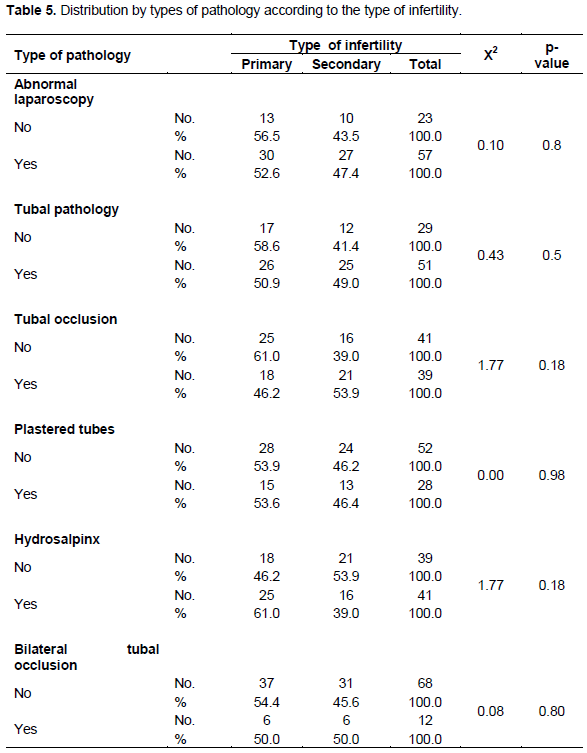
As shown in Table 5, there was no significant difference in prevalence of abnormal laparoscopy (p=0.8), tubal pathology (p=0.5) and tubal occlusion (p=0.18) between primary and secondary infertility.
Laparoscopy is an invaluable tool in the current evaluation and management of infertility, worldwide. In addition to detection of tuboperitoneal pathologies, it also enables their treatments with positive impact on fertility.
The prevalence rate of 71.3% of abnormal laparoscopy was found in this work and comprised mainly of tubal pathologies (63.8%) and peritoneal/pelvic adhesions (33.8%). This high prevalence of tuboperitoneal diseases among the studied women underlines the significant contribution of tubal pathologies to the aetiology of infertility in our region. The 63.8% rate of tubal pathologies found is very similar to 60.4% reported by Ikechebelu and Mbamalu (2010) in the same town six years ago among infertile women that presented in a specialist private hospital for management. They advocated the incorporation of laparoscopy in the initial evaluation of infertile women in the region.
This study found an overall rate of 48.8% for tubal occlusion comprising 33.8% of unilateral tubal occlusion and 15% of bilateral tubal occlusion. These findings are similar to the reports of Okafor et al. (2010) in Nnewi, Southeast Nigeria, who found a rate of 43.5% of tubal occlusions among infertile women managed in a tertiary health care facility. Their reported prevalence rate of 18.7% for bilateral tubal occlusion among the women was also similar to our rate of 15.0%.
Our tubal occlusion rate was however lower than 67.2% reported by Adesiyun et al. (2008) and 54.6% reported by Imo and Sunday-Adeoye (2008) in Abakiliki, Nigeria but higher than the previous reports from Otolorin et al. (1987) (35.4%) in Ibadan and Odusoga et al. (2002) (31.6%) in Sagamu.
The persisting high rates of tubal pathologies among infertile women in Nigeria poses a management challenge as assisted reproductive techniques are not commonly affordable in Nigeria and are also not covered by insurance. The aetiology of tubal occlusion in our study can be traced to pelvic adhesions arising from postoperative adhesions and pelvic infections. This seems plausible as the study also found a significant number of women with peritoneal adhesions (33.8%), past history of pelvic surgeries (38.7%), and in most cases the occlusions are located at distal part of the tube.
The other possible cause of the tubal occlusion was pelvic inflammatory disease as we observed Fitz Hutz Curtis syndrome in 11(13.8%) of cases. The finding of significant cases of deep dyspareunia (28.7%) and secondary dysmenorrhea (20.0%) further lends credence to the impact of the pelvic adhesions on the reproductive organ. The rate of 33.8% of peritoneal/pelvic adhesions found in our patients compares to 42.7% reported by Ikechebelu and Mbamara (2010), but much lower than that found by Odosuga et al. (2002) in Sagamu.
Post-operative adhesive disease represents a significant cause of morbidity for patients. Most obstetric and gynaecological surgeries are conducted using significant adhesion formation. In addition to infertility, the resultant effects include intestinal obstruction, chronic pelvic pain and difficulty with additional surgical treatment. It is clear therefore, that efforts to reduce tubal abnormalities in the environment will necessarily target reduction of adhesion formation following pelvic surgeries especially myomectomy.
Measures that have been shown to reduce post-operative adhesions include strict adherence to the basic surgical principles including gentle handling of tissues to minimize trauma, meticulous hemostasis, minimizing tissue ischemia and desiccation, and prevention of infection through postoperative antibiotic prophylaxis.
Other surgical adjuncts to prevent adhesion formation include irrigation with crystalloid solutions and high-molecular-weight dextran (Wiseman et al., 1998). The use of crystalloid solutions is known as hydroflotation. In these methods, some crystalloid is left in the pelvis at the end of surgery to allow the tissues to float apart from one another thereby decreasing the risk of adhesion formation.
Other strategies that have been found effective in reducing postoperative adhesion formation include the use of adhesion barriers such as expanded polytetrafluorethylene (Gore-Tex Surgical Membrane), oxidized regenerated cellulose (Interceed) and carboxymethylcellulose (Seprafilm) (Haney et al., 1995; Diamond, 1996).
Polycystic ovaries Syndrome (PCOS) were found as a factor of infertility in 26.3% cases. It is the commonest cause of anovulatory infertility in our region and management entails ovulation induction commonly with clomiphene citrate. The clomiphene resistant patients are usually offered laparoscopic ovarian drilling which was done for some of our patients. The other implications of PCOS include recurrent miscarriages, gestational and type II diabetes, cardiovascular disease as well as metabolic syndrome. The patients therefore, require long term follow up.
This study did not find any positive correlation of abnormal hysteroscopy findings with the type of infertility which may be due to the fact that the main cause of tubal occlusions was postoperative adhesion and not abortion related morbidities.
There is also a high rate of tuboperitoneal abnormalities among the studied population as well as no significant association with type of infertility. Thus, introduction of laparoscopy in the initial evaluation of infertility in our environment is ably recommended.
The authors have not declared any conflict of interests.
The authors wish to acknowledge the contributions of the clinical staff that assisted in collecting data from the patients and also participated during the laparoscopy procedures.
REFERENCES
|
Adesiyun AG, Ameh CA, Eka A (2008). Hysterosalpingographic tubal abnormalities and HIV infection among black women with tubal infertility in sub-Saharan Africa. Gynecol. Obstet. Invest. 66(2):119-22.
Crossref
|
|
|
|
Adeyemi AS, Adekanle DA, Afolabi AF (2009). Pattern of gynaecological consultations at Ladoke Akintola University of Technology Teaching Hospital. Niger. J. Clin. Pract.12:47-50.
|
|
|
|
|
Bello TO (2006). Tubal abnormalities on hysterosalpingography in primary and secondary infertility. West Afr. J. Med. 25(2):130-133.
|
|
|
|
|
Bukar M, Mustapha Z, Takai UI, Tahir A (2011). Hysterosalpingographic findings in infertile women: A seven year review. Niger. J. Clin. Pract. 14(2):168-170.
Crossref
|
|
|
|
|
Diamond MP (1996). Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL-F): a blinded, prospective, randomized, multicenter clinical study. Seprafilm Adhesion Study Group. Fertil. Steril. 66:904-910.
Crossref
|
|
|
|
|
Haney AF, Hesla J, Hurst BS, Kettel LM, Murphy AA, Rock JA, Rowe G, Schlaff WD (1995). Expanded polytetrafluoroethylene (Gore-Tex Surgical Membrane) is superior to oxidized regenerated cellulose (Interceed TC7+) in preventing adhesions. Fertil. Steril.63:1021-1026.
Crossref
|
|
|
|
|
Ibekwe PC, Udensi AM, Imo AO (2010). Hysterosalpingographic findings in patients with infertility in south eastern Nigeria. Niger. J. Med. 19(2):165-167.
Crossref
|
|
|
|
|
Imo AO, Sunday-Adeoye I (2008) Radiological assessment of the uterus and fallopian tubes in infertile women at Abakaliki, Nigeria. Niger. J. Clin. Pract. 11(3):211-215.
|
|
|
|
|
Ikechebelu JI, Mbamara SU (2010). Should laparoscopy and dye test be a first line evaluation for infertile women in southeast Nigeria? Niger. J. Med. 20(4):462-465.
|
|
|
|
|
Ikechebelu JI (2005). Prevalence of gynaecological diseases in Nnewi, Nigeria(2005). Niger. J. Clin. Pract. 8(2):136-137.
|
|
|
|
|
Ismajovich B, Wexler S, Golan A, Langer L, David MP(1986). The accuracy of hysterosalpingography versus laparoscopy in evaluation of infertile women. Int. J. Gynaecol. Obstet. 24(1):9-12.Available at:
Crossref
|
|
|
|
|
Karshima JA, Pam VC, Atim T, Abata PP Reich M I (2014). Indications for Gynaecological Consultation by Women at a Rural Outreach Centre in North-Central Nigeria. Int. J. Trop. Dis. Health 4(6):696-712.
Crossref
|
|
|
|
|
Kitilla T (2010). Hysterosalpingography in the evaluation of infertility: A five years review. (FGAE, 2001-5). Ethiop. Med. J. 48(4):267-275.
|
|
|
|
|
Nwosu BO, Ugboaja JO, Obi-Nwosu AL, Nnebue CC, Ifeadike CO (2012). Proximate determinants of antenatal care utilization among women in southeastern Nigeria. Niger. J. Med. 21(2):196-204.
|
|
|
|
|
Obuna JA, Ndukwe EO, Ugboma HA, Ejikeme BN, Ugboma EW (2012).
|
|
|
|
|
Odusoga OI, Oloyede OA, Adewunmi AA, Fakoya TA (2002). Experience with the laparoscope in the evaluation of infertile women in Sagamu. Niger. J. Clin. Pract. (5)2:127-129.
|
|
|
|
|
Okafor CO, Okafor CI, Okpala OC, Umeh E (2010). The pattern of hysterosalpingographic findings in women being investigated for infertility in Nnewi, Nigeria. Niger. J. Clin. Pract. 13(3):264-267.
|
|
|
|
|
Orhue A, Aziken M (2008). Experience with a comprehensive university hospitalâ€based infertility program in Nigeria. Int. J. Gynecol. Obstet. 101(1):11-15.
Crossref
|
|
|
|
|
Otolorin EO, Ojengbede O, Falase AO (1987). Laparoscopic evaluation of the tuboperitoneal factor in infertile Nigerian women. Int. J. Gynaecol. Obstet. 25(1):47-52.
Crossref
|
|
|
|
|
Tvarijonaviciene E, Nadisauskiene RJ (2008). The value of hysterosalpingography in the diagnosis of tubal pathology among infertile patients. Medicina (Kaunas). 44(6):439-448.
|
|
|
|
|
Wiseman DM, Trout JR, Diamond MP (1998). The rates of adhesion development and the effects of crystalloid solutions on adhesion development in pelvic surgery. Fertil. Steril.70:702-711.
Crossref
|
|