ABSTRACT
To evaluate the therapeutic effects of moisture exposed burn ointment (MEBO) on phlebitis, seven electronic databases where checked until September, 2016 for randomized controlled trials (RCTs) of MEBO on phlebitis. Risk of bias was assessed using Cochrane handbook guidelines. Thirty eight randomized controlled trials met the inclusion criteria in which the aggregated results indicated that comparison revealed significant differences in total effectiveness rate of MEBO versus conventional therapy (RR=1.27, 95% confidence interval [CI]=1.06, 1.52, and P=0.009), and there were some beneficial evidence regarding the effects on reducing incidence of phlebitis MEBO versus conventional therapy in preventing phlebitis (RR=2.73, 95% confidence interval [CI]=1.94, 3.85, and P<0.00001). The evidence that MEBO is an effective treatment for phlebitis is encouraging, but not conclusive due to the low methodological quality of the RCTs. Therefore, more high-quality RCTs with larger sample sizes are required.
Key words: External application of moisture exposed burn ointment, prevention and (or) treatment, phlebitis.
Intravenous therapy may be used to correct electrolyte imbalances, deliver medications for blood transfusion, or as fluid replacement, but studies have shown that 20 to 70% of patients receiving peripheral intravenous therapy develop phlebitis (Ray-Barruel et al., 2014; Evangelos and Abdulazeez, 2014). Phlebitis is an inflammatory response to intravenously injected drugs and leads to various types of vein damage including pain, erythema, swelling, warmth, hardening and thickening of injection area and finally, fever (Zhang et al., 2012). The most common phlebitis include venous indwelling needle-induced phlebitis, PICC-induced mechanical phlebitis (Myrianthefs et al., 2005a; Malach et al., 2006), amiodarone, nimodipine, 20% mannitol, alprostadil Injection, levofloxacin, and sodium chloride injection, Iatraliptic, β-aescine sodium, fusidate sodium and chemotherapy induced phlebitis such as 5-fluorouracil, vinorelbine (Thürlimann and Bachmann,1992);Wang et al., 2014). The highest incidence of infusion phlebitis is seen in patients receiving intravenous antibiotics and antineoplastic drugs (Leal et al., 2014);(Kohno et al.,2008). It can induce the pain, increase the risk of thrombophlebitis, lead to incomplete follow-up, and thereby affect the patient’s health status (Kohno et al., 2008).
There is no consensus on the optimal management of phlebitis in clinical practice, patients receive the following treatment regimens such as heparin, heparinoid or diclofenac gels, defibrotide, notoginseny creams by rubbing or flushing the site with 75% alcohol or 0.9% saline solution, wet compresses with 50 to 75% magnesium sulphate, hydrocolloid dressing,antagonist plus block therapy (2 ml 0.5% procaine and 5 mg dexamethasone in 7 ml normal saline), and topical application of anti-inflammatory drugs etc, these methods mainly focus on relieving the pain and improving the acute inflammatory state (Wang et al.,2014;(Kim et al.,2015). However, it is unclear whether such treatment is sufficient to prevent complications such as suppurate superficial thrombophlebitis or catheter-related bloodstream infections (Tagalakis et al., 2002); (Myrianthefs et al., 2005b). Heparin is associated with the risk of bleeding at the operation site and thrombocytopenia, and corticosteroids are followed by increased risk of infection through impaired defense system (Thürlimann and Bachmann, 1992). The effects of routine treatments are unsatisfactory.
Therefore, there is an urgent need to develop a simpler, more economical, and available method to prevent and alleviate phlebitis (Kim et al., 2015). Traditional Chinese Medicine (TCM) has been used for phlebitis in the past few decades. Moist exposed burn ointment (MEBO), a Chinese burn ointment with a USA patented formulation since 1995, which was developed at the China National Science and Technology Centre in Beijing in 1989, is one of such methods. MEBO contains sesame oil, β-sitosterol, berberine, and other small quantities of plant ingredients from Chinese herbal remedies including Coptis chinensis Franch, Scutellaria baicalensis Georgi, Phellodendron Chinese Schneid, Pheretima aspergillum and Papaver somniferum L. MEBO has been suggested to exert analgesic activity, anti-inflammatory activity, and antibacterial property, which was used in plastic surgery for patients with burns, sunburn, pressure sore, diabetic ulcers, skin graft donor site, and all types of surgical and traumatic wounds and has achieved beneficial efficacy (Al-Numairy, 2000); (Atiyeh et al., 2002).
As an important complementary therapy, although a substantial amount of research has investigated the chemical constituents of MEBO, which showed that the use of MEBO alone or combined with conventional therapy could offer an effective treatment method for phlebitis (Jewo et al., 2009; Ang et al., 2002). Presently, no previously published meta-analysis has investigated the benefits of MEBO as adjuvant treatment for patients with phlebitis. In addition, many studies could potentially be missed if literature searches are restricted to English-only sources (Ezzo et al., 1998). Therefore, meta-analysis was conducted to quantitatively summarize the therapeutic effect of MEBO in patients with phlebitis based on the available randomized controlled trials (RCTs).
Data sources and searches
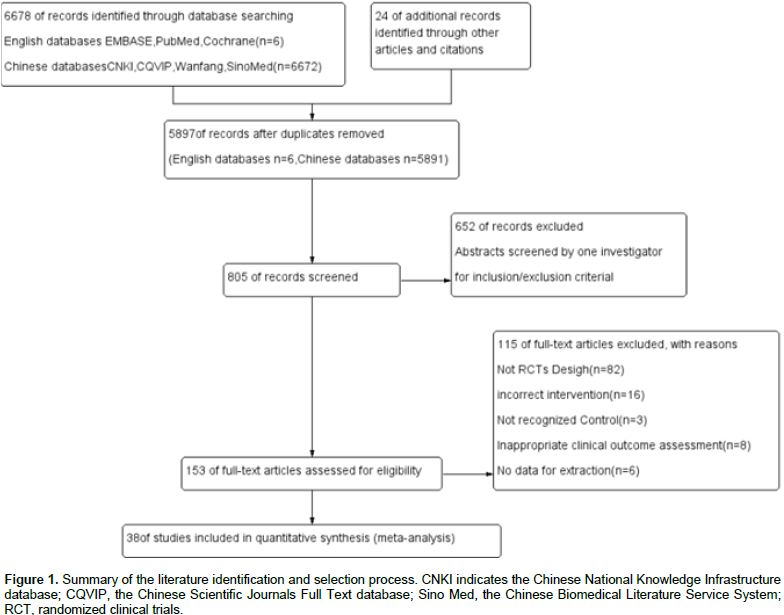
Two reviewers (Lian Liu and Song Wei Su) systematically searched the medical literature analysis and retrieval system online (MEDLINE), Excerpta medica database (EMBASE), Cochrane central register, Chinese scientific journals full text database (CQVIP), China National Knowledge Infrastructure database (CNKI), the Chinese Biomedical Literature Service System (SinoMed), and Wanfang data knowledge service platform. The search terms were “MEBO,” “moisture exposed burn ointment,” “phlebitis,” “prevention and (or) treatment,” and “randomized controlled trial,” “RCTs.” In this study, papers dating from the earliest citation in the databases until September, 2016 were included. Manual search in the references from original studies were performed to identify additional trials though there was no limit to publication languages and types, including abstract-only articles, conference proceedings and graduation dissertation, if criteria inclusion was met (Figure 1).
Study selection
Studies
RCTs were included. Quasi-RCTs, non-RCTs, or randomized trials with false randomization methods, incorrect intervention, inappropriate clinical outcome assessment, and no data for extraction, were excluded.
Participants
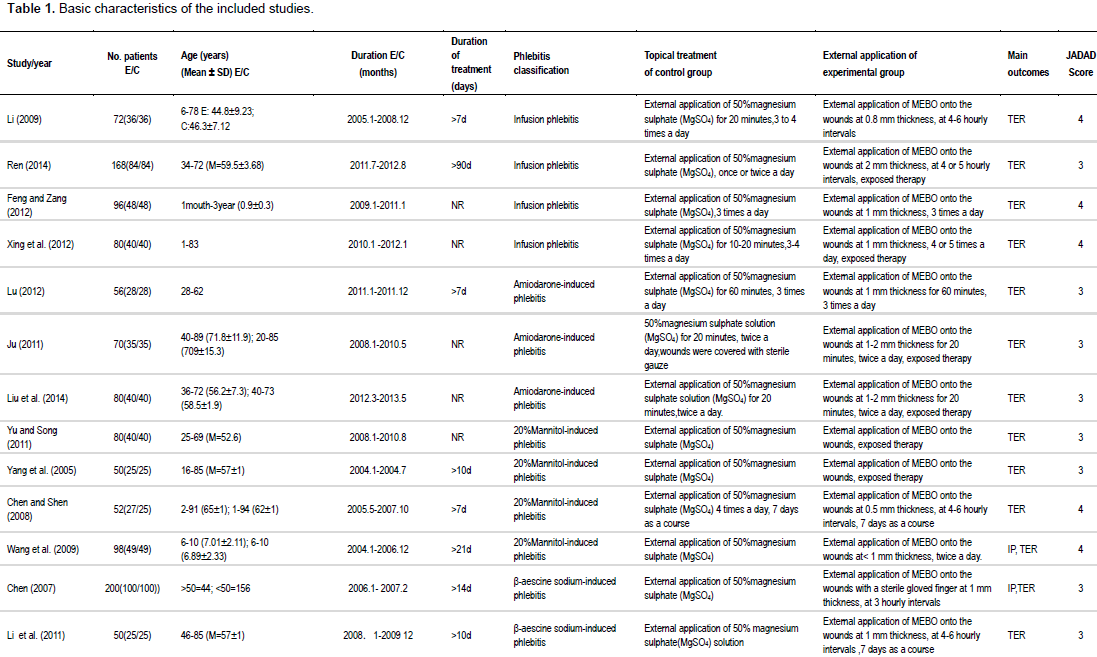
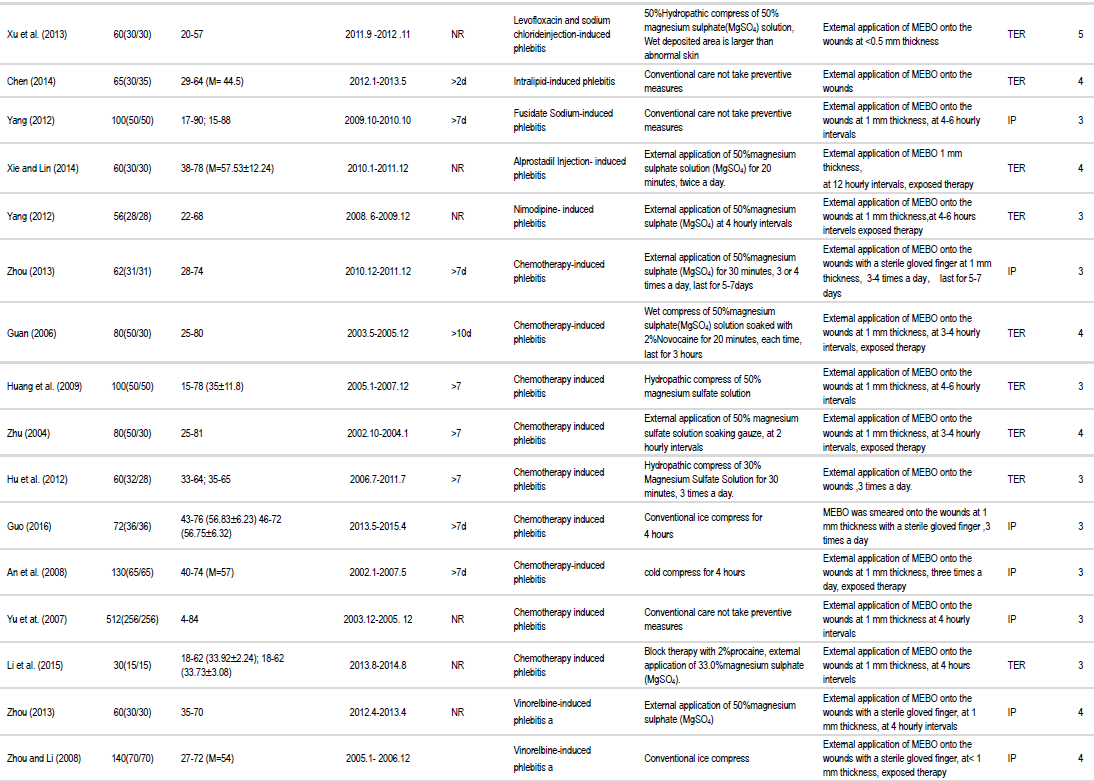
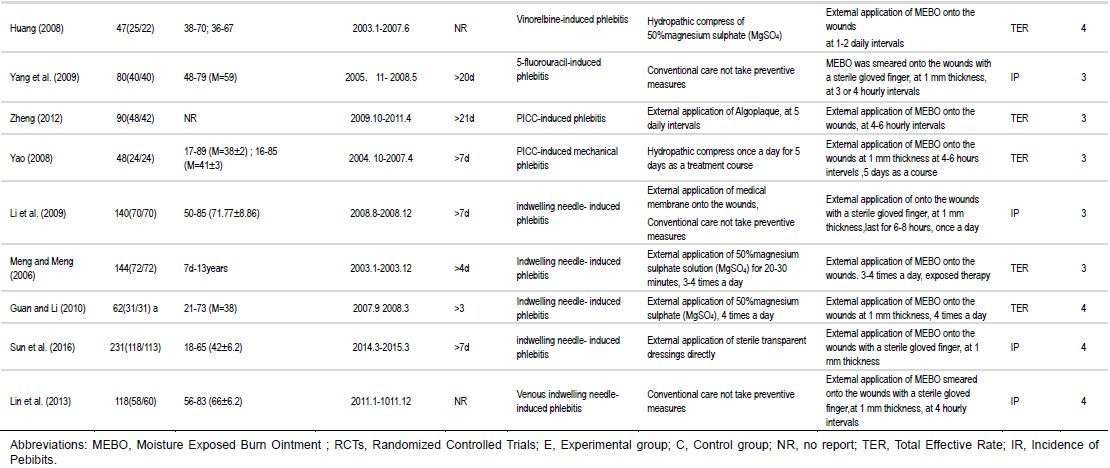
Patients diagnosed with phlebitis based on any set of explicit criteria were included; other severe infection or full-thickness dehiscence were excluded. There were no restrictive limitations on participant age, gender, nationality, or surgical procedures. Retrieval results in this study included infusion phlebitis (Xu et al., 2013); (Yang, 2012), such as amiodarone-induced phlebitis (Lu, 2012); (Ju, 2011), 20% mannitol induced phlebitis (Yu and Song, 2011); (Chen and Shen,2008), β-aescine sodium-induced phlebitis (Chen, 2007); (Li et al., 2011), levofloxacin and sodium chloride injection-induced phlebitis (Xu et al., 2013), intralipid-induced phlebitis (Chen, 2014), fusidate sodium-induced phlebitis (Yang, 2012), alprostadil injection-induced phlebitis (Xie and Lin, 2014), nimodipine-induced phlebitis (Yang, 2012), chemotherapy induced phlebitis (Zhou, 2013); (Yang et al.,2009), such as vinorelbine-induced phlebitis (Yan and Qiong, 2008); (Huang et al., 2008), 5-fluorouracil-induced phlebitis (Yang et al., 2009), PICC- induced mechanical phlebitis (Zheng, 2012; Yao, 2008), and in dwelling needle-induced phlebitis (Li et al.,2009); (Lin et al., 2013). (Table 1). Phlebitis was assessed based on infusion nursing standards of practice set by the American Infusion Nurses Society in 2006.
Interventions
The focused experimental groups received external application of MEBO, the wound sites were cleansed with normal saline gauze if they were soiled. The wounds were then dabbed dry with sterile gauze. MEBO was smeared onto the wounds at 1 to 3 mm thickness for exposed therapy alone or dressed with MEBO on Tulle gras several times daily (Table 1). Limitations were not set on dosages and routes of administration of MEBO.
Control group treatments
Control groups were defined as patients who received any type of conventional therapy without MEBO treatments, which included conventional dressing change (including iodophor, normal saline
solution, 75% alcohol, external application of 50% magnesium sulphate (MgSO4), ice compress, infrared radiation of wound surface, microwave radiating treatment etc., or just conventional attendance without taking preventive measures while measurements and documentation was performed (Table 1).
Outcome measurements
To provide more accurate effectiveness of the MEBO treatments, outcomes as total effectiveness rate of MEBO versus conventional therapy groups and incidence of phlebitis in preventing phlebitis applied with MEBO was evaluated. Trials were excluded if any of the following factors were identified:
1. Insufficient information concerning evaluation rates;
2. Lack of MEBO treatment and;
3. Mixed interventions in the experimental group (for example, MEBO combined with internal TCM and animal trials).
Data extraction
Two reviewers (Lian Liu and Song Wei Su) extracted data independently using predetermined inclusion criteria. Disagreements were resolved by consensus or arbitrated by the third investigator (Hong Yan Sun). The data extracted included the first author, title, year of publication, study characteristics, participant characteristics (that is, mean age, sample size, types of phlebitis, and topical therapy of experimental group/control group) and main outcomes. For studies with insufficient information, the reviewers contacted the primary authors to acquire and verify the data when possible. The use of modified JADAD scale evaluation mainly includes four aspects:
1. The generation of random sequence;
2. Random hidden;
3. Whether the use of blind method and;
4. Loss of access and withdrawal from the report.
The highest score is 7 points and the lowest is divided into 0 points. At present, 1 to 3 was considered as a low quality, and 4 to 7 considered as a high quality (Table 1).
Risk of bias assessment
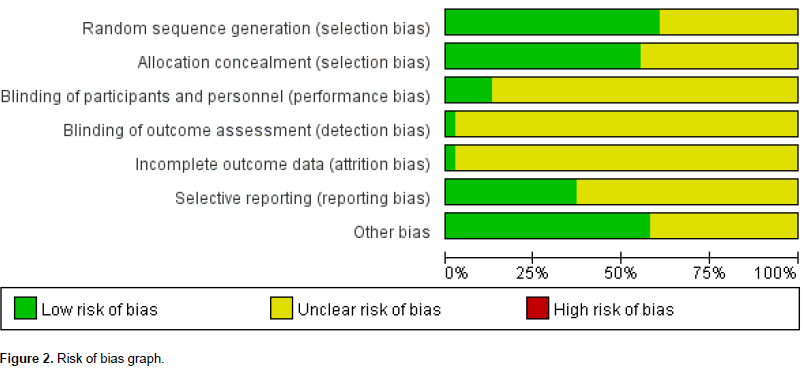
The risk of bias in each study was assessed by two independent authors (Ping Zhou and Ru Song) using the Cochrane risk of bias tool (Higgins et al., 2011); disagreements were resolved either by consensus or by a third reviewer (Hong Yan Sun). Risk of bias in included trials and methodological quality of the included studies is described in Figure 2.
Data synthesis and analyses
For this meta-analysis, the total effectiveness rates of dichotomous data were pooled using risk ratios (RRs). All statistical analyses were performed using Review Manager 5.3.1 software (Cochrane Community, London, United Kingdom). Cochrane’s χ2 and I2 tests were used to assess the degree of heterogeneity between studies. There was considerable heterogeneity for P-values less than 0.10, or I2 value above 50%, in the χ2 and I2 tests, respectively (Higgins et al., 2011), in this case, a random-effects model was used to compute the global RR. Otherwise, with 𑃠values greater than 0.10 or ð¼2 less than 50%, between-study heterogeneity was not substantial, and the fixed-effect models were suitable. Clinical heterogeneity was assessed by reviewing the differences in the distribution of participants’ characteristics among trials (that is, age, gender, and different types of phlebitis and conventional topical treatment).
Study selection
From a total of 6,702 titles, the full text of 805 potentially relevant studies was reviewed to confirm their eligibility. Among these 153 studies, 115 were excluded including 82 non-RCT studies, 16 with incorrect interventions, 3 did not recognized control, 8 showed inappropriate clinical outcome assessment, and 6 no data for extraction. Finally, 38 trials met the inclusion criteria (Figure 1). All the 38 RCTs were conducted in China and published in Chinese with randomization procedure and single center.
Study characteristics
A total of 3,779 participants were included in these trials, with 1,898 and 1,881 in the experimental and control groups, respectively. The sample sizes of these trials ranged from 30 to 512 (Table 1). There were no statistically significant differences between two groups in patient characteristics, in terms of gender, age, severity of phlebitis, underlying comorbidity, and etiological factor. The doses and routes of the MEBO used in each trial varied and the most common form of conventional therapy used in 24 trials was 50% magnesium sulphate, other forms of conventional care used in clinical trials are listed in Table 1.
Risk of bias assessment
The methodological quality of all included trials was poor (Figure 2). Although all these trials reported random sequence generation, only two adequately described the randomization method (Xu et al., 2013);(Guan, 2010). Moreover, none of the studies reported information such as allocation concealment, blinding of participants and personnel, and blinding of outcome assessment. All the relevant trials adequately addressed incomplete outcome data, selective reporting could not be judged in all the studies because of the insufï¬cient information provided. No other biases were found in these trials; however, considering their poor methodological quality, it was determined that an unclear risk of bias should be given to all the included trials.
Outcomes
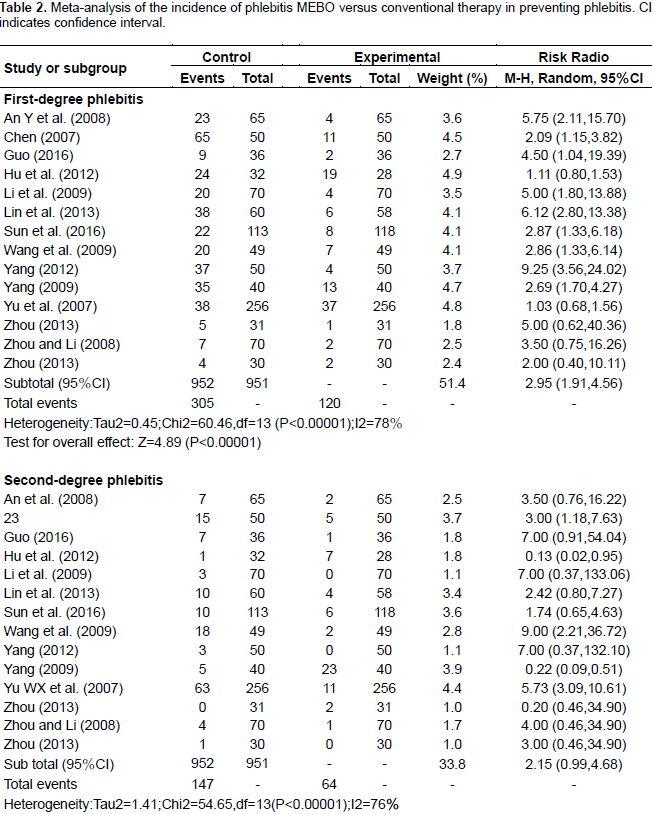
Incidence of phlebitis external application of MEBO versus conventional therapy in preventing phlebitis
Fourteen RCTs containing 1,903 patients studied the incidence of phlebitis while the experimental and control groups received MEBO and conventional therapy, respectively. Pooling of the results from these trials showed a significant difference (RR = 2.73, 95% confidence interval [CI] = 1.94, 3.85, and P < 0.00001) using the random-effects model, and there were also significant differences in each subgroup (First-degree phlebitis RR = 2.95, 95% CI = 1.91, 4.56, P < 0.00001; second-degree phlebitis RR = 2.15, 95% CI = 0.99, 4.69, P < 0.00001; third-degree phlebitis RR=3.21 95% CI = 1.47, 7.04, P = 0.004) (Table 2).
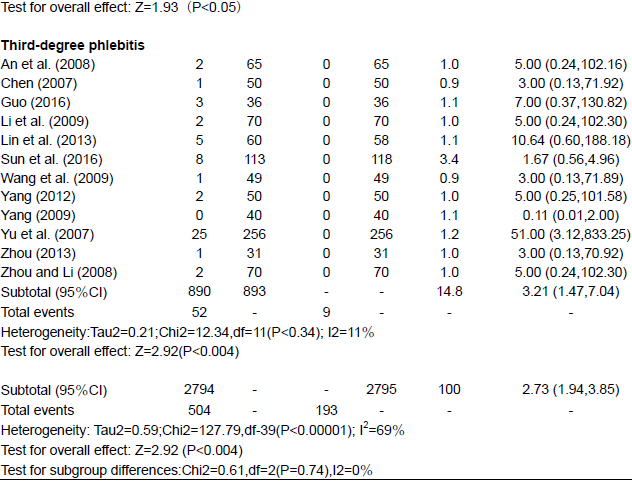
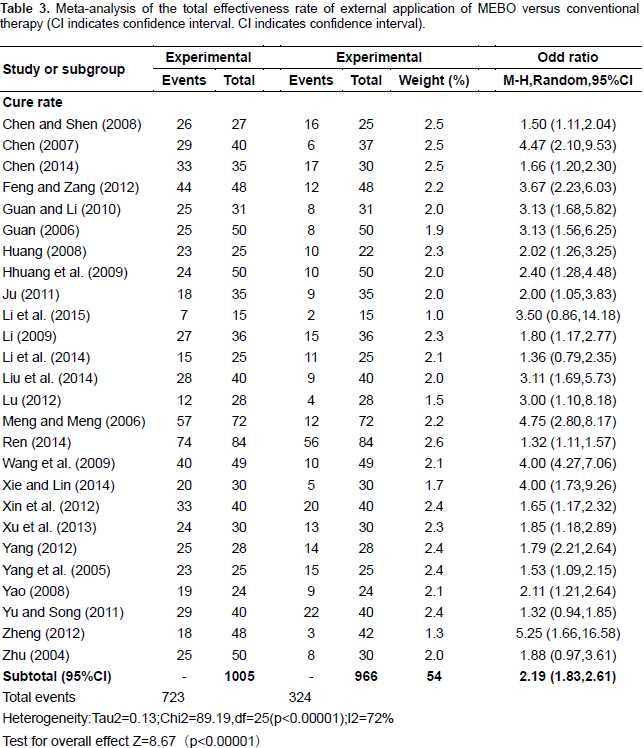
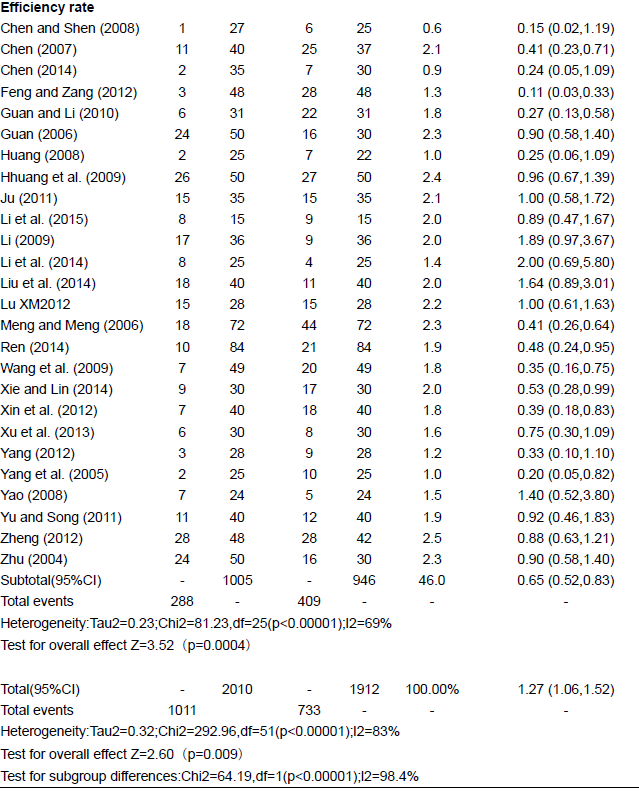
Total effectiveness rate of external application of MEBO versus conventional therapy in management of phlebitis
Twenty six RCTs containing 1,971 patients illustrated the total effectiveness rate, the experimental and control groups received topical application of MEBO and conventional preventive measures, respectively. Results of meta-analysis using the random-effects model indicated significantly higher total effectiveness rate for MEBO compared to that of the control groups (RR = 1.27,95% confidence interval [CI] = 1.06, 1.52, and P = 0.009), and significant differences were found between subgroups of cure rate (RR = 2.19, 95% CI = 1.83, 2.61, P < 0.00001); and efficiency rate (RR = 0.65, 95% CI = 0.52, 0.83, P < 0.00001) (Table 3).
Adverse events
No study reported adverse events in the experimental groups or control groups with MEBO.
Sensitivity analysis
Sensitivity analysis using the leave-one-out approach indicated the finding was reliable and was not dependent on any single study. The direction of the combined estimates did not vary markedly with the removal of each study in turn, indicating that the meta-analysis was robust and the data was not overly influenced by any single study.
Assessment of publication bias
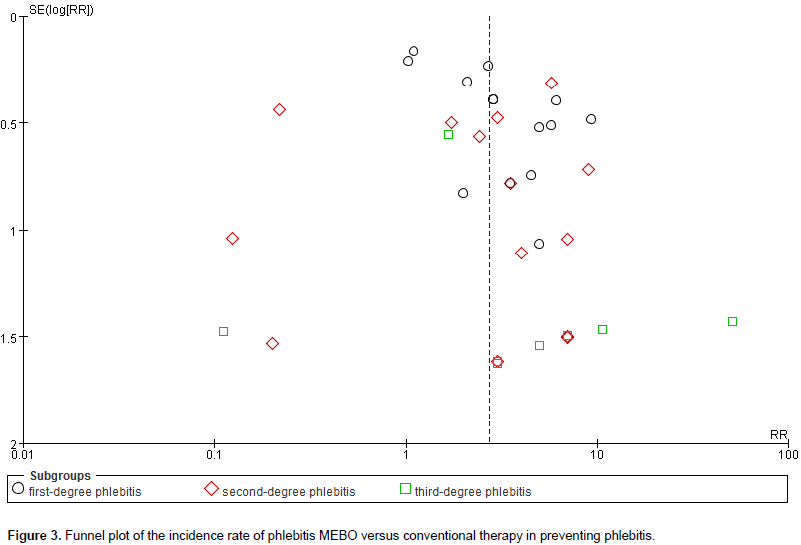
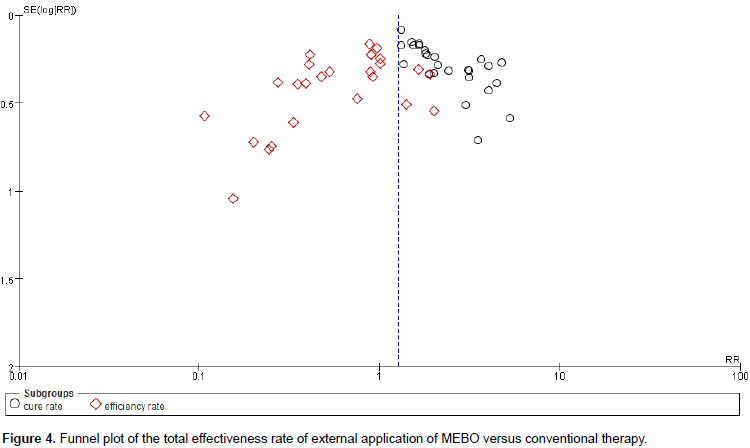
In this review, the funnel plots for incidence rate of phlebitis and total effectiveness rate of MEBO was combined with conventional therapy 14 RCTs, 26 RCTs, respectively (Figures 3 and 4). Regarding these studies of MEBO for phlebitis, the publication bias was small because the spots were substantially symmetric, and none of the studies lies outside the limits of the 95% CI. However, the probability of publication bias may also exist in this study because of all included trials published in Chinese.
Summary of evidence
MEBO has been used in clinical practice for many years as an adjunctive treatment method to phlebitis; however, this paper was the ï¬rst systematic review and meta-analysis to assess the effects of MEBO in comparison with conventional measures. A total of 38 RCTs were identified, a detailed subgroup analysis based on different comparisons revealed the clinical outcome of phlebitis. Even though most of the trials had small sample sizes and poor methodological quality, analysis of the pooled data showed a consistently superior effect of MEBO in aminophylline, terms of increasing total effectiveness rate and reducing the incidence of phlebitis. MEBO could even lead to a shorter postoperative recovery time by decreasing healing time of phlebitis, when compared to the control groups. But it was not assessed, as well as final pain measurements, the mean hospitalization time and the recurrence rates during follow-up in this meta-analysis for incomplete data, inappropriate clinical outcome assessment or no effective data for extraction. There were no patients who dropped out of their trials due to adverse effects, suggesting that MEBO was safe for clinical use.
Possible mechanism of MEBO for phlebitis
Phlebitis is an inflammation of the veins in which the vascular intima proliferates, leading to narrowing of the vascular cavity and slowing of the blood flow. Congestive erythema accompanied by edema sometimes appears in the peripheral skin but fades over time and is replaced by pigmentation. After the occurrence of phlebitis, a minority of patients present with general phlebitis symptoms (including a decrease in skin temperature, fever and raised white blood cell counts), and complain of pain and swelling. Most common related risk factors include: Female sex, low pH and high-osmolality intravenous solutions, many cancer chemotherapeutic agents, intravenous antibiotics such as vancomycin, amphotericin B, “poor-quality” peripheral veins, insertion in the lower extremity, and underlying medical disease (cancer, immunodeficiency, hypercoagulability) (Myrianthefs et al., 2005a);(Malach et al., 2006); (Aljitawi et al., 2005); (Leal et al., 2014); (Milutinović et al.,2015). Especially calcium glubionate, vancomycin and benzylpenicillin antibiotics, aminophylline, amiodarone hydrochloride and potassium chloride 7.4% were identified to potentially cause phlebitis (Spiering, 2014).
During drug-induced phlebitis, endothelial cells are activated with subsequent induction and up-regulation of E-selectin expression, and they become amenable to adherence by inflammatory cells in blood such as neutrophils, which ultimately leads to a cascade of events including loss of endothelial cells, increased vascular permeability, infiltration of inflammatory cells, onset of tissue edema, and even thrombosis (Kohno et al., 2008); (Di Nisio et al.,2015); (Myrianthefs et al., 2005b). Research has shown that conventional application of magnesium sulfate could improve the vascular permeability and reduce the small artery spasm, thereby quickly eliminating the inflammatory edema of local tissue, but the moisture evaporates quickly on the sterile gauze; pharmacological efficacy could not reach sufficient concentration at local vascular vessel, thus reducing the wet compress duration in management of phlebitis. Moreover, magnesium sulfate is easy to form crystals on the skin, thus producing stimulation to the skin (Galgon et al., 2015; Yamamoto et al., 2016).
Compared to magnesium sulfate, external use of MEBO alone or combined with conventional therapy could offer a more effective treatment method for phlebitis. According to traditional Chinese medicine (TCM), all phlebitis share common characteristics, the primary pathogenesis of phlebitis is due to “Re (heat) evil,” “Yu (qi-stagnancy, blood-stasis),” “Xu (qi blood and yin yang deficiency)” and stagnated blood obstructing meridians and collaterals. The basic treating principle is to invigorate blood circulation and remove blood stasis, warming Yang and relieving spasm, clearing away heat and cooling blood, invigorating Qi and nourishing blood, and finally providing supplements for deficiencies (Zhang et al., 2001); this is just how MEBO act in the prevention and treatment of phlebitis according to TCM theory. In modern pharmacology research, while the exact mechanism of action of MEBO has not been fully elucidated, studies indicated that MEBO has a unique mechanism of wound debridement by which the necrotic tissues become fragmented and liquefied chemically by esterification and saponification processes, then surrounded by oil globules and removed physically through oil frame base of the ointment (Johnson et al., 2003; liu et al., 2012; Yang et al., 2005).
The moving up globules creates negative suction of air, providing the necessary oxygen. It provides physiological moisture necessary to optimize wound healing and re-epithelialization (Vincy, 2004); (Allam et al., 2007). In addition, it has pharmacological effects as it reduces water evaporation from the burn surface thus improving microcirculation, as well as anti-inflammatory, anti-bacterial, and analgesic effects. It also promotes debridement, epithelial repair and improves scar formation. A moist environment enhances wound healing by preventing tissue dehydration and cell death, but particularly by promoting angiogenesis (through the presence of growth factors and proteinases in the fluidexudate), keratinocyte migration (epidermal cells migrate easier over a moist wound surface than below the eschar), wound drainage and breakdown of necrotic tissue. Therefore, MEBO significantly promote the formation of granulation tissue in cutaneous wounds like phlebitis, shortened the time of wound healing, and increased neovascularization and the number of fibroblasts (Hindy, 2009); (Tsati et al.,2004)..
It could be the case that apart from tumor necrosis factor (TNF) and interleukin-1, vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) also exhibit key roles in inflammatory reflex and wound healing. VEGF promotes angiogenesis/vasculogenesis and vascular permeability, it enhances endothelial cell proliferation and migration, as well as the adhesion of leukocytes. Further research revealed that VEGF stimulates hydrogen sulfide synthesis and release from endothelial cells, thus leading to subsequent endothelial cell growth, migration and permeability, micro-vessel formation, collagen deposition and wound healing. Recent data indicated that bFGF-mediated angiogenesis refers to endothelial cell proliferation, migration, and tube formation by activating c-Jun N-terminal kinase/stress activated protein kinase signaling. Also, research has shown that local administration of MEBO for eight days markedly increased the levels of VEGF and bFGF by 77.5 and 90.8%, respectively (all P<0.01), when compared with the model group.
Furthermore, quantitative polymerase chain reaction (qPCR) analysis indicated that MEBO treatment for eight days led to increase in the mRNA expression of VEGF and bFGF by 40.9 and 97.1%, respectively, when compared with the recombinant bovine basic fibroblast growth factor (rbbFGF) group (all P<0.05) (Tang et al.,2014). The results indicate that MEBO increases the protein expression levels of VEGF and bFGF to promote wound healing, implicating the potential mechanism of MEBO for delayed cutaneous wound healing. Moreover, CK19 is considered as a bio-marker specifically expressed in epidermal stem cells. A study had investigated the effect of MEBO topical application on activation and proliferation of epidermal stem cells through the immune histo-chemically localization of cytokeratin 19 (CK19). More researches have shown that the analgesic effect of MEBO is attributable to the presence of the layer of oily ointment that shields the burn wound from external environment. During the first 2 weeks post-randomization, the cumulative MRSA infection rates at 14 days for Control group and MEBO group were 38.5 and 37.4%, respectively (See et al., 2001); (Tang et al., 2014).
This systematic review demonstrated positive evidence regarding the effects of MEBO on phlebitis, but it is not conclusive due to the low methodological quality of the RCTs. Given the small sample size and heterogeneity of the included trials, multicenter and larger scale RCTs are needed to verify our conclusion.
LIMITATIONS AND IMPLICATIONS FOR RESEARCH
Nevertheless, some limitations of this meta-analysis should be discussed. Firstly, the number of RCTs and the number of patients included in retrieved studies were limited. In the assessment of publication bias, the power of this meta-analysis was modest due to the limited number of trials and patients. Secondly, although all trials had a randomization design, very few studies reported the randomization procedure at length thus the blinding of participants and allocation concealment or outcome assessment were not available, resulting in high risk of selection or detection bias. Third, while Cochrane’s ðœ’2 and ð¼2 tests revealed no statistical heterogeneity in the total effectiveness rate among these studies, an unpredictable clinical heterogeneity was present nonetheless.
It is believed that differences in MEBO dose, treatment duration, basic intervention strategies and conventional therapies, wound-cleaning methods, time interval of drug application and evaluation criterion were the major sources of the heterogeneity and the follow-up durations of most studies were not longer than one month thus the use meta-analysis to assess the long-term effect of MEBO for phlebitis patients was not performed. Fourthly, all the RCTs included in the present meta-analysis were conducted in China and published in Chinese, causing high risk of selection bias. Therefore, more trials with high methodological quality are needed to further identify the effectiveness and safety of MEBO treatments. Randomized controlled trials should be strictly required in study design and reported, based on the consolidated standards of reporting trials (CONSORT).
Rigorous methods of design, measurement, and evaluation (DME) following the Cochrane Handbook should be applied to enhance the representativeness of the sample (Higgins et al., 2011). Clinical trial registries should be encouraged to provide details of the protocols, speciï¬cally, placebo-controlled clinical trials are essential. Furthermore, careful consideration of the interventions for responding to different levels of phlebitis severity is required to ï¬nd optimal subgroups that provide greater beneï¬ts than harm. Outcome measures should include the evaluation of sub-items in the internationally recognized scales. Quality of life and long term effect should be assessed as well.
The authors have not declared any conflict of interests.
This study was supported by grant from the Department of Science and Technology of Sichuan Province--Luzhou Municipal People's Government-- joint special foundation of Luzhou Medical College (Grant No.14JC0070); Department of Science and Technology of Sichuan Province--Luzhou Municipal People's Government-- (Grant No.2013LZLY-J35).
REFERENCES
|
Aljitawi O, Shabaneh B, Whitaker J (2005). Bilateral Upper Extremity Thrombophlebitis Related to Intravenous Amiodarone: A Case Report. Southern Med. J. 98(8):813-816.
Crossref
|
|
|
|
Allam AM, Mostafa W, Zayed E, El-Gamaly J (2007). Management of the acute partial-thickness burned hand; moist exposed burn ointment or silver sulphadiazine cream both combined with a polyethylene bag. Ann. Burn Fire Disaster 20(3):144.
|
|
|
|
|
Al-Meshaan M, Abdul HM, Quider T, Al-Sairafi A, Dham R (2008). Role of Mebo (Moist Exposed Burn Ointment) in the Treatment of Fournier'S Gangrene. Ann. burns fire Disaster 21(1):20.
|
|
|
|
|
Al-Numairy A (2000). Clinical Use of MEBO in Wounds Management in UAE. Int. J. Cosmet. Surg. Aesthet. Dermatol. 2(1):27-33.
Crossref
|
|
|
|
|
An Y, Wu MH, Li Y, Peng H, Yang XH (2008). Application of MEBO in Preventing Chemotherapy Phlebitis in 65 Cases. Available at:
View
|
|
|
|
|
Ang E, Lee ST, Gan CS, Chan YH, Cheung YB, Machin D (2003). Pain control in a randomized, controlled, clinical trial comparing moist exposed burn ointment and conventional methods in patients with partial-thickness burns. J. Burn. Care Rehabil.24:289-296.
Crossref
|
|
|
|
|
Ang ES, Lee ST, Gan CS(2002).The role of alternative therapy in the management of partial thickness burns of the face--experience with the use of moist exposed burn ointment (MEBO) compared with silver sulphadiazine. J. Ann. Acad. Med. Singapore. 29(1):7-10.
|
|
|
|
|
Atiyeh BS, Dham R, Kadry M, Abdallah AF, Al-Oteify M, Fathi O, Samir A (2002). Benefit–cost analysis of moist exposed burn ointment. Burns 28(7):659-663.
Crossref
|
|
|
|
|
Boyce BA, Yee BH (2012). Incidence and Severity of Phlebitis in Patients Receiving Peripherally Infused Amiodarone. Crit. Care Nurs. 32(4):27-34.
Crossref
|
|
|
|
|
Chen PF, Shen YS (2008). Application of MEBO MEBO in the Phlebitis Induced by Mannitol. Available at:
View
|
|
|
|
|
Chen F (2007). Effect of MEBO on preventing and treating phlebitis induced by sodium aescinate. Available at:
View
|
|
|
|
|
|
|
Chen Y (2014). MEBO moisturizing burn cream applied to the clinical evaluation of fat emulsion exudative phlebitis. Available at:
View
|
|
|
|
|
Di Nisio M, Peinemann F, Porreca E, Anne WR (2015).Treatment for superficial infusion thrombophlebitis of the upper extremity. Cochrane Database Systematic. Reviews. Available at:
View
Crossref
|
|
|
|
|
El-Hadidy MR, El-Hadidy AR, Bhaa A, Asker SA, Mazroa SA (2014). Role of epidermal stem cells in repair of partial-thickness burn injury after using Moist Exposed Burn Ointment (MEBO ®) histological and immunohistochemical study. Tissue Cell 46:144-151.
Crossref
|
|
|
|
|
Evangelos T,Abdulazeez S (2014). Improving the frequency of visual infusion phlebitis (VIP) scoring on an oncology ward. BMJ Qual. Improv. Rep. 3(1):u2054-w2364.
|
|
|
|
|
Ezzo J, Berman BM, Vickers AJ, Linde K(1998). Complementary medicine and the Cochrane Collaboration. Jama, 280(18):1628-1630.
Crossref
|
|
|
|
|
Feng X, Zang H (2012). Efficacy of topical application of MEBO in the treatment of phlebitis induced by infusion.
|
|
|
|
|
Galgon RE, Strube P, Heier J, Groth J, Wang SJ, Schroeder KM (2015).Magnesium Sulfate with Lidocaine for Preventing Propofol Injection Pain: A Randomized, Double-Blind, Placebo Controlled Trial. J. Anesthesiol. 29(2):206-211.
|
|
|
|
|
Guan C (2010). Effect of MEBO in treating phlebitis induced by peripheral venous catheterization.Available at:
View
|
|
|
|
|
Guan WJ (2006). Treatment of 50 Cases of Chemotherapy Phlebitis with MEBO. Available at:
View
|
|
|
|
|
Guo G (2016). Preventive effect of MEBO treated with MEBO. Available at:
View
|
|
|
|
|
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JA (2011). The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928.
Crossref
|
|
|
|
|
Hindy AMGAD (2009). Comparative study between sodium carboxymethyl-cellulose silver, moist exposed burn ointment, and saline-soaked dressing for treatment of facial burns. Ann. burn Fire Disaster 22(3):131.
|
|
|
|
|
Hu Y, He XB, Huang H (2012). Efficacy of MEBO in the treatment of drug extravasation after chemotherapy. Available at:
View
|
|
|
|
|
Huang A, Kao L, Zeng Y (2008). External application of MEBO in treatment of vinorelbine-induced phlebitis (leakage injury).Available at:
View
|
|
|
|
|
Huang YP, Huang LL, Chen HP (2009). Efficacy of MEBO in treating 50 cases of chemotherapy phlebitis. Available at:
View
|
|
|
|
|
|
|
Jewo PI, Fadeyibi IO ,Babalola OS, Saalu LC, Benebo AS, Izegbu MC, Ashiru OA(2009).A Comparative study of the wound healing
|
|
|
|
|
Johnson JL, He Y, Yalkowsky SH (2003). Prediction of Precipitation-Induced Phlebitis: A Statistical Validation of an In Vitro Model. J. Pharm. Sci. 92(8):1574-1581.
Crossref
|
|
|
|
|
Ju HR (2011) Efficacy of MEBO in treating phlebitis induced by amiodarone injection.
|
|
|
|
|
Kim MH, Young A, Han SH, Kim JH, Hwang JW, Jeon YT (2015). The effect of magnesium sulphate on intubating condition for rapid-sequence intubation: A randomized controlled trial. J. Clin. Anesth. 27:595-601.
Crossref
|
|
|
|
|
Kohno E, Murase S, Nishikata M (2008). Research Paper Methods of preventing vinorelbine-induced phlebitis: an experimental study in rabbits. Int. J. Med. Sci. 5(4)218-223.
Crossref
|
|
|
|
|
Leal AD, Kadakia KC, Looker S, Hilger C, Sorgatz K, Anderson K, Jacobson A, Grendahl D, Seisler D, Hobday T, Loprinzi CL (2014). Fosaprepitant-induced phlebitis: a focus on patients receiving doxorubicin/cyclophosphamide therapy. Support Care Cancer 22(5):1313-1317.
Crossref
|
|
|
|
|
Li B, Jiang JX, Li CX (2015). Efficacy of MEBO MEBO in treating chemotherapy - induced skin lesions and phlebitis. Available at:
View
|
|
|
|
|
Li SD, Zhang XL, Cai XS (2009). Observation of the effect of topical application of MEBO in preventing phlebitis by intravenous. at:
View
|
|
|
|
|
Li XZ (2009). Efficacy of External Application of MEBO in Treating Phlebitis. Available at:
View
|
|
|
|
|
Li YF, Wang J, Sun JL (2011). Therapeutic effect of MEBO MEBO in treating phlebitis induced by β-aescinate sodium. Available at:
View
|
|
|
|
|
Lin YZ, Ye L, Ye LL, Chen LL (2013). Therapeutic effect of MEBO MEBO in preventing phlebitis caused by indwelling needle
|
|
|
|
|
Liu C ,Yang FL, Zhao XH (2014). Effect of MEBO in treating amiodarone phlebitis. Available at:
View
|
|
|
|
|
Liu F, Chen D, Liao Y (2012). Apparatus on Phlebitis in a Neurological Intensive Care Unit: A Case-control Study. J. Intern. Med. Res. 40(6)2321-2326.
Crossref
|
|
|
|
|
Lu XM (2012). Effect of MEBO in treating phlebitis induced by amiodarone. Available at:
View
|
|
|
|
|
Malach T, Jerassy Z, Rudensky B, Schlesinger Y (2006). Prospective surveillance of phlebitis associated with peripheral intravenous catheters. Am. J. Infect. Control 34(5):308-312.
Crossref
|
|
|
|
|
Meng GP, Meng GL (2006). Clinical Application of MEBO in Treating Intravenous Needle Combined with Phlebitis.Available at:
View
|
|
|
|
|
Milutinović D, Simin D, Zec D (2015). Risk factor for phlebitis: A questionnaire study of nurses' perception. Rev. Lat. Am. Enfermagem. 23(4):677-684.
Crossref
|
|
|
|
|
Myrianthefs P, Karatzas S, Baltopoulos G (2005a). Complications, thrombophlebitis rates, and intravenous catheter replacement strategies. Infection 33(2):96-97.
Crossref
|
|
|
|
|
Myrianthefs P, Sifaki M, Samara I, Baltopoulos G (2005b). The epidemiology of peripheral vein complications: Evaluation of the efficiency of differing methods for the maintenance of catheter patency and thrombophlebitis prevention. J. Evaluation Clin. Pract. 11(1):85-89.
Crossref
|
|
|
|
|
Ray-Barruel G, Polit DF, Murfield JE, Rickard CM (2014). Infusion phlebitis assessment measures: a systematic review. J. Evaluation Clin. Pract. 20(2):191-202.
Crossref
|
|
|
|
|
Ren L (2014). Treatment of infusion phlebitis by MEBO external application: a report of 84 cases. Available at:
View
|
|
|
|
|
See GJ, Chan YH, Lee-Hua Ng BN, Machin D (2001). Evaluating the role of alternative therapy in burn wound management: randomized trial comparing moist exposed burn ointment with conventional methods in the management of patients with second-degree burns. Medscape/General Med. 3(12):3-18.
|
|
|
|
|
Spiering M (2014).Peripheral Amiodarone-Related Phlebitis: An Institutional Nursing Guideline to Reduce Patient Harm. J. Infusion Nurs. 37(6):453-460.
Crossref
|
|
|
|
|
Sun QL, Tian M, Tian BB, Zhang QF, Ding ZG (2016). Efficacy of MEBO in preventing phlebitis induced by surgical indwelling needle. Available at:
View
|
|
|
|
|
Tagalakis V, Kahn SR, Libman M, Blostein M (2002).The Epidemiology of Peripheral Vein Infusion Thrombophlebitis: A critical review. Am. J. Med. 113(2):146-151.
Crossref
|
|
|
|
|
Tang QL, Han SS, Feng J (2014). Moist exposed burn ointment promotes cutaneous excisional wound healing in rats involving VEGF and bFGF. Mol. Med. Rep. 9(4):1277-1282.
Crossref
|
|
|
|
|
Thürlimann B, Bachmann I (1992). Effective prevention of chemotherapy-induced phlebitis by low-dose heparin: A prospective randomised trial. Ann. Oncol. 3(4):311-313.
Crossref
|
|
|
|
|
Tsati E, Panayotou P, Ioannovich J (2004). Moist exposed burn therapy: evaluation of the wound healing process. An experimental model to assess the efficacy of local agents on wound repair in partial-and full-thickness wounds. European J. Plastic Surg. 27(4):171-177.
Crossref
|
|
|
|
|
Vincy LWS (2004) Comparison of Moist Exposed Burn Ointment (MEBO) with Silver Sulfadiazine (Ag-S) for the Treatment of Deep Burn Injury .Hong Kong Baptist University School of Chinese Medicine . Bachelor of Science (Hons) in Biomedical Science April. Available at:
View
|
|
|
|
|
Wang Z, Ma LJ, Wang XB (2014).Cimetidine attenuates vinorelbine-induced phlebitis in mice by militating E-selectin expression. Cancer Chemother. Pharmacol. 74:239-247.
Crossref
|
|
|
|
|
Xie WR, Lin HY (2014). Nursing Analysis of MEBO MEBO in Treating
|
|
|
|
|
Xing YB, Zhang XQ, Chen YF (2012). Application of MEBO in the Infusion Infusion of Intravenous Infusion. Available at:
View
|
|
|
|
|
Xu J, Bai ZY, Peng X (2013). Efficacy of MEBO MEBO in treating phlebitis. Available at:
View
|
|
|
|
|
Yamamoto T, Mori K, Esaki T, Nakao J, Watanabe M (2016). Preventive effect of continuous cisternal irrigation with magnesium sulfate solution on angiographic cerebral v Y asospasms associated with aneurysmal subarachnoid hemorrhages: A randomized controlled trial . J. Neurosurg.124:18-26.
Crossref
|
|
|
|
|
Yan W, Shu-Qian W, Jing Qu (2009). Clinical Experience on Preventing Infant from Phlebitis Caused by the Application of Venous Indwelling Needle with MEBO. Available at:
View
|
Yang S (2012). The effect of MEBO on the prevention of phlebitis caused by intravenous infusion of fusidic acid. Chinese J. Burn Urol. 13(6):495-496.
|
|
|
|
Yang XH (2012). Effect of MEBO in treating phlebitis induced by nimodipine.
|
|
|
|
|
Yang XH, Huang JH, Chen JX (2005). Clinical Observation of MEBO's Scalds-plasters by Wet Compressing in the Treatment of Mannitol-induced Phlebitis. J. Hebei. Med. 11(6):562-563
|
|
|
|
|
Yang XQ, Yang JD, Zhang Q, Zhao X (2009). Effect of MEBO MEBO in Preventing 40 Cases of Phlebitis Caused by 5-Fu.
|
|
|
|
|
Yao C (2008). Comparison of the Efficacy of External Application of MEBO in Treating Mechanical Phlebitis Caused by PICC Catheterization.
|
|
|
|
|
Yu CY, Song HM (2011). Therapeutic effect of MEBO MEBO in treating phlebitis induced by mannitol.
|
|
|
|
|
Yu W, Li C, Prospect, Wu W, Zeng H (2007). Clinical Study on External Application of MEBO in Preventing Chemotherapy Phlebitis.
|
|
|
|
|
Zhang HQ, Yip TP, Hui I, Lai V, Wong A (2005). Efficacy of moist exposed burn ointment on burns. J. Burn Care Res. 26(3):247-251.
|
|
|
|
|
Zhang YJ, Chen ZX, Liu YJ, Zhang YL(2001).Treating principles and methods of traditional Chinese medicine in treatment of peripheral vascular diseases. Journal of traditional Chinese medicine= Chung i tsa chih ying wen pan/sponsored by All-China Association of Traditional Chinese Medicine. Acad. Tradit. Chinese Med. 21(2):130-133.
|
|
|
|
|
Zhang ZX, Wang P,Zhang QS, Pan X, Zhao QX,Wang XK (2012).Original article Effects of anisodamine on the expressions of vascular endothelial growth factor and intercellular adhesion molecule 1 in experimental infusion phlebitis. Chin. Med. J. 125(2):300-305.
|
|
|
|
|
Zheng SH (2012). Experimental study of two methods for treatment of phlebitis induced by peripheral central venous catheter chemotherapy.
|
|
|
|
|
Zhou D (2013). Clinical Application of MEBO in Preventing Chemotherapy Phlebitis.
|
|
|
|
|
Yan Z, Qiong L (2008). Observation on effect of moist burn cream plus ice compress to prevent patients from Vinorelbine caused phlebitis [J]. Chinese Nurs. Res. 2:047.
|
|
|
|
|
Zhou YH (2013). Effect of magnesium sulfate wet dressing combined
|
|
|
|
|
Zhu AE (2004). Efficacy Observation and Experience of MEBO in Treating Chemotherapy Phlebitis.
|
|
|