ABSTRACT
The reason for a long stay in the Intensive Care Unit (ICU) is unknown in most cases, but there are some risk factors that can prolong the patients’ stay in the ICU. However, the threshold of prolonged length of stay is useful in analyzing the quality of health care and hospital costs. The main objective of this study was to assess the factors affecting prolonged intensive care unit stay in Nigist Eleni Mohammed Memorial Hospital from January, 2015 to January, 2016. Institutional based cross sectional study design was conducted. Census was used to include all study participants admitted to intensive care. Regular supervision and follow up was made. Data was entered into Epi info version 7 by investigators and was transported to statistical package for social sciences (SPSS) version 20 for analysis. Bivariate and multivariate analysis was used to identify factors associated with patient’s outcome. A total of 280 patients were included in the study by census. The mean length of stay in the intensive care unit was 5.49 ± 4.36. Majority of patients (61.4%) had poor nutrition status. In addition to their underlying diseases, majority of the patients in the intensive care units had one or more comorbidities. Poor nutritional status, male sex, presence of comorbidity and unplanned extubation was significantly associated with length of stays in intensive care unit at p-value less than 0.05. In this study, it was found that unconscious patients had about two times more likelihood to have prolonged length of stays in intensive care unit than conscious patients (AOR 1.724; 95% CI: 809 to 3.676). Higher proportions of patients stayed in the intensive care unit for more than three days. Therefore, the implication of this study was to recommend the decrease in length of intensive care unit stays in medically appropriate ways.
Key words: Intensive care unit, Ethiopia, length of stay, patient management.
Abbreviation:
ICU, Intensive care unit; LOS, length of stays; NEMMH, Nigst Eleni Mohammed Memorial Hospital.
Length of stay (LOS) in the intensive care unit (ICU) is one of the most important factors that influence health management (Keenan et al., 1998; Halpern and Pastores, 2010). Prolonged stays in the intensive care unit are associated with high costs and burdens on patients, patients’ families and in turn affect society at large. It
is associated with a complicated clinical course of the diseases with higher incidence of respiratory and renal insufficiency (Joskowiak et al., 2013). Therefore, it can decrease the chance of survival and reduce the quality of life (Lagercrantz et al., 2010), which may result in increased costs and reduced hospital beds available in the ICU (Arabi et al., 2002; Doering et al., 2000; Azarfarin et al., 2014).
A primary goal in intensive care is to decrease length of stay in a medically appropriate way which helps to improve the quality of medical care, reduce hospital cost and avoid excess use of resources (Jaber et al., 2006). The precise prediction of the length of ICU stay enables the physicians to obtain reliable information to provide a better care for patients, allocating funds to the health care systems and changing their routines (Azarfarin et al., 2014; Austin et al., 2002; De Cocker et al., 2011). Therefore, this study was conducted to identify potential factors of prolonged ICU stays that enable health care providers and managers to devise different strategies which in turn help to reduce length of stay (LOS) on one hand and improve quality of care for critically ill patients and reduce hospital cost on the other hand.
Study setting
A cross-sectional study design was conducted from January, 2015 to January, 2016 at Nigst Eleni Mohammed Memorial Hospital (NEMMH) in Hosanna town. Hosanna town is an administrative city of Hadiya zone which is located at a distance of 230 km to the south of Addis Ababa, capital city of Ethiopia. The hospital has nine wards. There are adult and neonatal intensive care units in the hospital. All adult critical ill patients from different departments have been admitted to adult intensive care unit. This study excluded neonates as they were admitted to neonatal intensive care unit. The hospital has a total of 220 beds including eight and seven beds in neonatal and adult ICU, respectively.
Source population
This includes all charts of patients admitted to adult intensive care unit of Nigst Eleni Mohammed Memorial Hospital.
Study population
This includes selected charts of patients admitted to adult intensive care unit of Nigist Eleni Mohammed Memorial Hospital from January, 2015 to January, 2016.
Sample size determination and sampling technique
Census was used to include all eligible 280 patients admitted to adult intensive care unit of Nigist Eleni Mohammed Memorial Hospital from January, 2015 to January, 2016.
Data collection tools and procedure
Data was collected using structured questionnaires by two B. Sc. anesthetists and supervised by one M. Sc. holder anesthetist. Patient’s charts were reviewed. At the end of data collection, patient’s charts were replaced into its original place properly.
Data quality assurance and data analyzing
The structured questionnaire prepared in English was used as a data collection tool. Data collectors and supervisors were trained on each items included in the study tools, objective, relevance of study, and right of respondents. During data collection, regular supervision and follow up were made. The data was entered into epi info version 7 and was exported to SPSS version 20 computer program for analysis. Bivariate and multivariate analyses were used to detect the effect of independent variable over length of ICU stays. A p-value of less than 0.05 was used as a cut of point for presence of association. Strength of association was measured by 95% confidence interval and/Odd ratio.
Definitions
Operational definitions
Prolonged ICU stays: Patients who stayed in the intensive care unit for more than three days.
Unplanned extubations: Premature removal of an endotracheal tube by a patient receiving mechanical ventilation support or unintentional removal of an endotracheal tube by staff during nursing and medical procedures.
Ethical consideration
Ethical clearance and approval was obtained from the Ethical Review Committee, Anesthesia Department, Wolaita Soddo University. Permission to conduct the work was obtained from the hospital. The obtained data was only used for the study purpose. Confidentiality and anonymity were ensured.
Socio-demographics and personal information
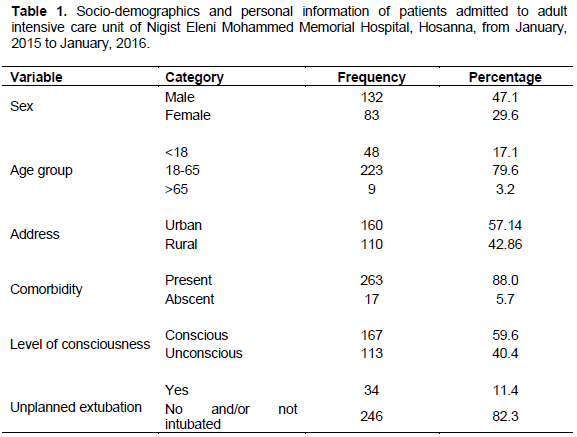
A total of 280 patients were enrolled in the study of which majority of them were male. Almost four fifth of the patients were found between age groups of 18 to 65 years. About 78.3% of the sampled respondents were married. The percentages of patients below 18 years and above 65 years were about 17.1 and 3.2%, respectively. Majority of them were from urban area. Patients in the intensive care unit can have single or multiple comorbidities. But, in this research, comorbidity diagnosis was divided into two categories, namely the presence and the absence of comorbidity. In addition to their underlying diseases, majority of the patients in the intensive care units developed comorbidities (Table 1).
Length of ICU stays
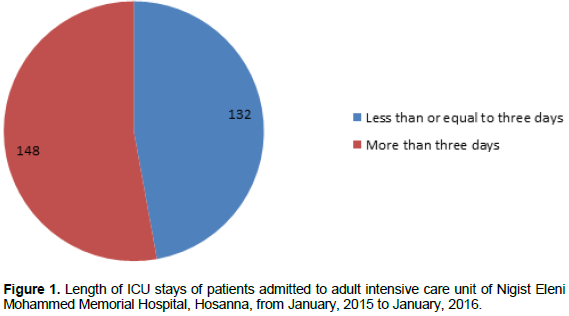
Mean length of stays in the intensive care unit was 5.49 ± 4.36 (minimum 1 and maximum 15) which included both survivors and non-survivors. About 47.1% of the patients stayed in the intensive care unit for less than three days (Figure 1).
Nutrition status, age and gender among different categories of hospital stay
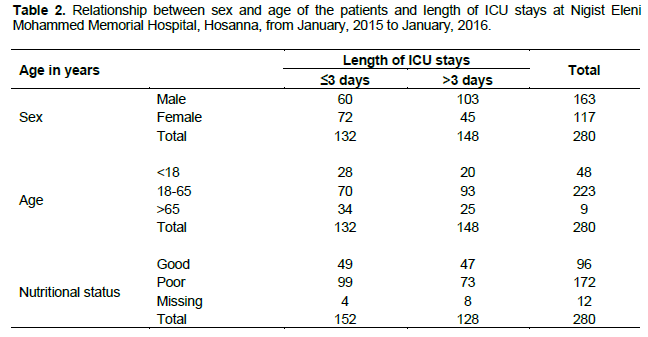
The height and weight of the patients used to calculate the body mass index (BMI), which is important to determine the nutritional status of the patients could not be obtained. Therefore, instead of using BMI to determine whether the patient is malnourished or not, the status of albumin level as indicators of nutritional status was used. Below the normal level of albumin (N<3.5 to 5.0 g/dl) was considered as poor nutrition status, while normal level was good nutrition status (N: 3.5 to 5.0 g/dl). According to the results of this study, majorities of patients (61.4%) had below normal albumin level which means that most of the patients in the intensive care units had poor nutrition status. Majority of the male patients stayed for more than three days and the reverse was true for female (Table 2).
Factors affecting length of stay in intensive care units
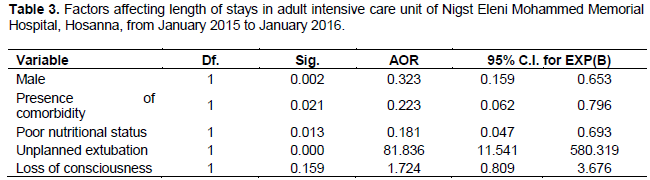
The result of multivariate analysis showed that sex, infection, nutritional, unplanned extubation had strong association with prolonged ICU stay at p-value of less than 0.05. Unconscious patients had about two times more likely to have prolonged length of stays in intensive care unit than conscious patients (AOR 1.724; 95% CI: 0.809 to 3.676) (Table 3).
The reduction of length of stays in intensive care unit should be a major aim of medical staff as longer ICU stays increase the risk for infections and associated with a higher risk of hospital death (Vincent et al., 2009; Cavallazzi et al., 2012)and have immense costs (Wunsch et al., 2012). Some study revealed that social, psychological, and institutional factors have an impact on ICU length of stay. Lack of effective communication and the occurrence of conflicts between the physician and the patient’s family can also lead to prolonged ICU stays (Higgins et al., 2003; Dimick et al., 2001). However, these cannot be identified in our study as psychological and social factors could not be recorded on patient’s chart and it was considered as limitation of our study. Therefore, the study was conducted on other important risk factors available on patient’s charts like age, sex, category of disease, nutritional status, presence of comorbidity, unplanned extubation and level of consciousness.
In these studies, the reason for a long stay in the ICU is unknown in most cases, but there are some risk factors that can prolong the patients’ stay in the ICU. However, due to the differences among the populations and the countries, and the definition of prolonged ICU stay in different centers, the predictive models of a hospital may not be applicable in another hospital (Azarfarin et al., 2014; Curtis et al., 2002; Gardner et al., 2001).
In the present research, it was found that majority of the patients had prolonged ICU stays which is consistent with other similar study (Sugiarto and Darmawan, 2014). According to the result of present study poor nutritional status and presence of comorbidities had a significant relationship with length of stay which was consistent with other similar study. However, in this studies age did not show significant relationship with LOS. Another study also found that comorbidities influence not only the outcome of patients but also it affects length of ICU stays (Ingeman et al., 2011; Luker et al., 2011). The study conducted on recent trends in the treatment of spontaneous intracerebral hemorrhage revealed that individual comorbidities could influence the outcome of patients and length of ICU stays (Ingeman et al., 2011). For example, some studies used hypertension or diabetes mellitus as outcome indicators, and other researchers found that respiratory failure or pneumonia influence the LOS and mortality rate of patients (Andaluz and Zuccarello, 2009; Szepesi et al., 2015). These patients utilize more hospital resources than those with a single comorbidity or no comorbidities, no matter whether the comorbidities arise from previous disease history or complications. Although the previous disease history of patients cannot be changed, decreasing complications using quality control methods will lead to a better outcome and a shorter LOS (Ingeman et al., 2011).
The likely causes of prolonged ICU stays among patients who developed comorbidities were acute deterioration in vital sign of critically ill patients and the involvement of other vital organ in the disease process.
Limitations of this study were due to lack of availability of adequate risk factors on the patient’s chart which might be important to thoroughly discuss risk factors of length of ICU stays and inadequate sample size.
The aim of intensive care medicine is to provide quality of care for patients while reducing length of stays in intensive care unit. In this study, poor nutritional status, male sex, presence of comorbidity and unplanned extubation had significant relation with LOS. There may also be social and psychological factors that influence patients’ length of stays. Majorities of patients stayed in intensive care unit for a prolonged period. Therefore, it was recommended to reduce length of stay by preventing modifiable risk factors and improving the type and quality of communication. Further prospective studies on risk factors of length of stay should be conducted to come up with all potential risk factors of length of ICU stays.
The authors have not declared any conflict of interest.
We would like to thank all the staff in the ICU and record keeper for their support during data collection.
REFERENCES
|
Andaluz N, Zuccarello M (2009). Recent trends in the treatment of spontaneous intracerebral hemorrhage: analysis of a nationwide inpatient database: Clinical article. J. Neurosurg. 110:403-410.
Crossref
|
|
|
|
Arabi Y, Venkatesh S, Haddad S, Alshimemeri A, Al malik S (2002). A prospective study of prolonged stay in the intensive care unit: predictors and impact on resource utilization. Int. J. Qual Health Care 14:403-410.
Crossref
|
|
|
|
|
Austin PC, Rothwell DM, TU JV (2002). A comparison of statistical modeling strategies for analyzing length of stay after CABG surgery. Health Serv. Outcomes Res. Methodol. 3:107-133.
Crossref
|
|
|
|
|
Azarfarin R, Ashouri N, Totonchi Z, Bakhshandeh H, Yaghoubi A (2014). Factors influencing prolonged ICU stay after open heart surgery. Res. Cardiovasc. Med. 3(4).
Crossref
|
|
|
|
|
Cavallazzi R, Saad M, Marik PE (2012). Delirium in the ICU: An overview. Ann. Intensive Care 2:49.
Crossref
|
|
|
|
|
Curtis JJ, Mckenneyâ€Knox, CA, Wagnerâ€mann CC (2002). Postcardiotomy centrifugal assist: a single surgeon's experience. Artif Organs 26:994-997.
Crossref
|
|
|
|
|
De cocker J, Messaoudi N, Stockman BA, Bossaert LL, Rodrigus IE (2011). Preoperative prediction of intensive care unit stays following cardiac surgery. Eur. J. Cardio-Thoracic Surg. 39:60-67.
|
|
|
|
|
Dimick JB, Pronovost PJ, Heitmiller RF, Lipsett PA (2001). Intensive care unit physician staffing is associated with decreased length of stay, hospital cost, and complications after esophageal resection. Crit. Care Med. 29:753-758.
Crossref
|
|
|
|
|
Doering LV, Esmailian F, Laks H (2000). Perioperative predictors of ICU and hospital costs in coronary artery bypass graft surgery. Chest J. 118:736-743.
Crossref
|
|
|
|
|
Gardner SC, Grunwald GK, Rumsfeld JS, Mackenzie T, Gao D, Perlin JB, Mcdonald G, Shroyer ALW (2001). Risk factors for intermediate-term survival after coronary artery bypass grafting. Ann. thoracic Surg. 72:2033-2037.
Crossref
|
|
|
|
|
Halpern NA, Pastores SM (2010). Critical care medicine in the United States 2000–2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit. Care Med. 38:65-71.
Crossref
|
|
|
|
|
Higgins TL, Mcgee WT, Steingrub JS, Rapoport J, Lemeshow S, Teres D (2003). Early indicators of prolonged intensive care unit stay: Impact of illness severity, physician staffing, and pre–intensive care unit length of stay. Crit. Care Med. 31:45-51.
Crossref
|
|
|
|
|
Ingeman A, Andersen G, Hundborg HH, Svendsen ML, Johnsen SP (2011). In-hospital medical complications, length of stay, and mortality among stroke unit patients. Stroke Strokeaha 110:610881.
Crossref
|
|
|
|
|
Jaber S, Amraoui J, Lefrant JY, Arich C, Cohendy R, Landreau L, Calvet Y, Capdevila X, Mahamat A, Eledjam JJ (2006). Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit. Care Med. 34:2355-2361.
Crossref
|
|
|
|
|
Joskowiak D, Kappert U, Matschke K, Tugtekin S (2013). Prolonged intensive care unit stay of patients after cardiac surgery: initial clinical results and follow-up. Thoracic Cardiovasc. Surg. 61:701-707.
Crossref
|
|
|
|
|
Keenan SP, Massel D, Inman KJ, Sibbald WJ (1998). A systematic review of the cost-effectiveness of noncardiac transitional care units. Chest 113:172-177.
Crossref
|
|
|
|
|
Lagercrantz E, Lindblom D, Sartipy U (2010). Survival and quality of life in cardiac surgery patients with prolonged intensive care. Ann. Thoracic Surg. 89:490-495.
Crossref
|
|
|
|
|
Luker JA, Bernhardt J, Grimmer-somers KA (2011). Demographic and stroke-related factors as predictors of quality of acute stroke care provided by allied health professionals. J. Multidiscipl. Healthcare 4:247-259.
Crossref
|
|
|
|
|
Sugiarto N, Darmawan ES (2014). The Factors Affecting the Length of Stay in the Intensive Care Units of Pertamina Central Hospital in Indonesia Related to Healthcare Associated Infections. J. US-China Med. Sci. 11: 195-204.
Crossref
|
|
|
|
|
Szepesi R, Széll IK, Hortobágyi T, Kardos L, Nagy K, Lánczi LI, Berényi E, Bereczki D, Csiba L (2015). New prognostic score for the prediction of 30-day outcome in spontaneous supratentorial cerebral haemorrhage. BioMed Res. Int. 2015:961085
Crossref
|
|
|
|
|
Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y (2009). International study of the prevalence and outcomes of infection in intensive care units. Jama 302(21):2323-2329.
Crossref
|
|
|
|
|
Wunsch H, Gershengorn H, Scales DC (2012). Economics of ICU organization and management. Crit. Care Clin. 28(1):25.
Crossref
|
|