ABSTRACT
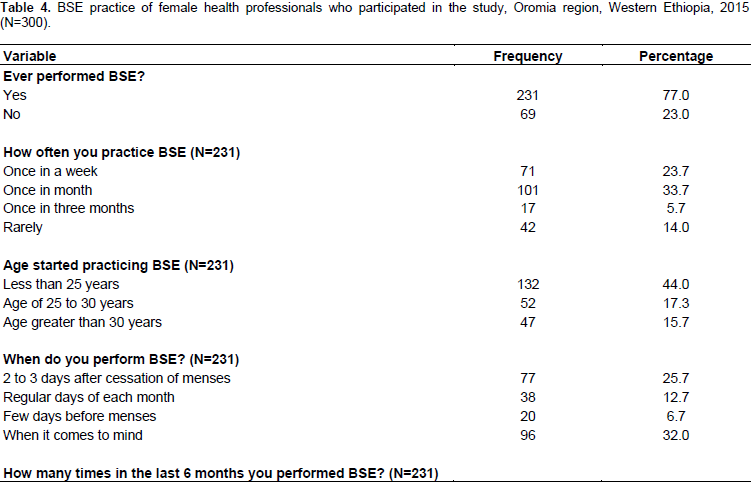
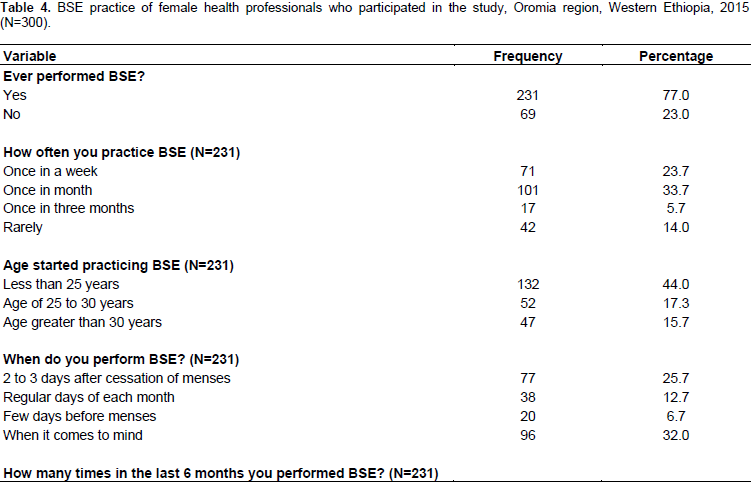
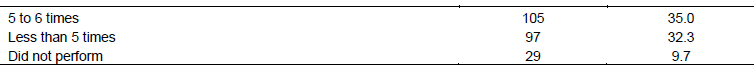
Breast cancer is the leading cause of cancer mortality worldwide. Breast cancer incidence is increasing both in developed and developing regions. Regular breast self-examination (BSE) is one of the most cost effective methods for early detection of breast cancer in asymptomatic women. The aim of this study is to assess the magnitude of BSE practice and its associated factors among female health professionals working in public health facilities in Western Ethiopia. The study applied is health facility based cross-sectional study design. Simple random sampling technique was used to recruit a total of 390 female health professionals. The study was conducted from January to March, 2015. Bivariate and multivariable logistic regression model was used, odds ratios with 95% confidence intervals were computed and significance of all tests was decided at p-value of 0.05. From the total respondents, 77% had ever practiced BSE and only one third (33.7%) of them practiced regularly. Not experiencing breast problem (12.7%) was the main reason for not practicing regular BSE. After adjusting for possible confounders; personal history of breast cancer (AOR=4.7, 95%CI: 1.32-17.07), having knowledge of BSE (AOR=4.1, 95%CI: 1.36-5.65), positive attitude (AOR, 3.8, 95%CI: 2.10-9.17) and ever taught BSE to a client (AOR=5.2, 95%CI: 2.35-8.14) were found to be statistically significant predictors of BSE. Even though the life time BSE practice in this study was high, the regular BSE practice was low. Thus, trainings on BSE practice will be important to improve the practice level of health professionals and their counseling skill for the clients.
Key words: Breast self-examination, health professionals, practice, females.
Cancer is a group of disease that causes cells in the body to change and grow out of control. An estimated 12.7 million new cancer cases and 7.6 million cancer deaths occurred in 2008. Higher burden of cancer was observed in less developed regions of the world which accounts for 56% of new cancer cases and 63% of cancer deaths worldwide (Ferlay et al., 2010). Breast cancer has increasingly become an issue of public health importance in both developed and developing nations because of its high incidence-prevalence, the over-burdened health system and direct medical expenditure. It is the second leading cause of death among women worldwide with an estimated 1.38 million new cases diagnosed annually which accounts for 10.9% of all cancer cases next to lung cancer. It is the fifth cause of overall cancer mortality with an estimated 458,000 deaths (Bray et al., 2013).
Breast cancer incidence is increasing both in developed and developing regions. In 2008, an estimated 636,000 incident cases were diagnosed in high resource countries, while 514,000 cases were diagnosed in low and middle resource countries. It is the most frequent cause of death among women both in developing (269,000 deaths (12.7%) of total) and developed region with an estimated 189,000 deaths. It is estimated that 70% of all breast cancer cases worldwide will be in low and middle resource countries by 2020 (IARC, 2008). Breast cancer is the most commonly diagnosed cancer in women with age-adjusted incidence rate of 28 per 100,000 and the second leading cause of death in women in Africa. The incidence varies across the continent ranges from 19.3 per 100,000 per year in Eastern Africa to 38.1 per 100,000 in Southern Africa (Ibrahim and Odusanya, 2009).
Breast self-examination (BSE) is one of screening methods, which involves the woman herself looking at and feeling each breast for possible lumps, distortions or swelling. BSE is a simple exercise which can potentially save the life of a woman. It is recommended for every woman above the age of 20 years to be done for 20 minutes every month (Ginseng et al., 2012). However, women in developing countries do not perform BSE for various reasons (Fung, 1998).A woman who performs regular BSE may be more motivated to seek medical attention, including Clinical Breast Examination (CBE) and mammography (Balogun and Owoaje, 2005). A study conducted in Ethiopia among women with breast cancer shows that more than half of the patients were age 50 and younger. Around 69.6% of patients ignored their symptoms initially for an average of more than one and half year (Dye et al., 2012).
BSE is still recommended as a general approach to increasing breast health awareness and thus potentially allow for early detection of any anomalies, because it is free, painless and easy to practice (Ginseng et al., 2012). The American Cancer Society also recommends that
women, starting from the age of 20 years should be educated on the pros and cons of performing a monthly BSE (The American Cancer Society, 2014)Most healthcare facilities in Ethiopia do not have advanced laboratory investigations for diagnosing breast cancer. Women present for health care at late stages of breast cancer, at which treatment is most ineffective. The early detection and diagnosis methods are not accessible to all women especially women leaving outside major cities. Therefore, many women miss early detection and treatment opportunities due to lack of information, knowledge and awareness of breast cancer, as well as to cancer screening practices. In resource scarce countries like Ethiopia, BSE should be promoted for early detection of breast cancer to prevent related morbidities and mortalities (Azage et al., 2013).
The finding of this study will provide information to the concerned bodies to plan potential important interventions. Furthermore, better documentation of female health professional practice of BSE would be useful to design interventions aimed at reducing breast cancer mortality through increasing community awareness and improving early diagnosis and treatment of the disease. Therefore, the aim of this study was to assess the magnitude of BSE practice and its associated factors among female health professionals working in public health facilities located in Western Ethiopia.
Settings, study design and area
The study applied health facility based cross-sectional study design. The study was conducted from January to March, 2015. The study was carried out in four zones of Western Ethiopia (East, West, and Kellem and Horro Guduru Wollega zones) health facilities (hospitals and health centers). In these selected zones for the study, there are 9 hospitals and 100 health centers. The total numbers of female health professionals working in the four selected zones’ hospitals and health centers are about 2000. Simple random sampling technique was used to recruit a total of 390 female health professionals.
Sample size determination
The sample size for the quantitative survey was computed using a formula for calculating single population proportions, with 95% confidence level and 5% level of accuracy. Sample size was calculated considering the prevalence of practice of BSE which was conducted among female health care professionals in Addis Ababa, which was 35.5% (Teferi et al., 2012). After adjustment, the calculated total sample size was 314 female health care professionals.
Sampling techniques
Health centers were selected by simple random sampling technique. The sample size in each health center was proportional to population size. Sampling frame of female health professionals working in each health facilities have been prepared and study subjects were selected from the frame by using simple random sampling method.
Data collection and processing
A quantitative data was collected using self-administered questionnaire. The questionnaire was prepared originally in English and then translated to Afan Oromo and Amharic languages and back retranslated to English to check its consistency. Data collectors and supervisors’ training was given by the investigators to make them familiar with the data collection tool. Pre testing was conducted on 5% of the sample size and based on the result necessary amendment were made. The investigators and supervisors were assisting and coordinating the data collectors as well as the health professionals during data collection. The questionnaire contains five parts; these are socio demographic, history of breast cancer, knowledge, attitude about BSE, and practice of BSE. The collected data were reviewed and checked for completeness before data entry. Five percent of the data were double-entered in order to compare and assure the quality of the data.
Ethical consideration
Ethical clearance was obtained from Research Ethics Review Committee of Wollega University and the research was done in conformity with the ethical guidelines approved by the Institutional Review Board (IRB) of Wollega University. Supporting letter was written by Wollega University to zonal and woreda health offices to get institutional consent after communicating with formal letters and to other relevant concerned bodies to get official permission. Respondents were informed about the objective and purpose of the study. Participation in the study was completely voluntary and refusal to respond to some of the questions or interruption from the study was possible at any time the respondent need. Written consent was attached to each questionnaire and was read out by the interviewer at the time of data collection. All participants signed on the written consents form provided after completing the questionnaire. Prior to interview of each study participant, both verbal and written consent procedures were approved by IRBs of Wollega University.
Socio-demographic profile of the participants
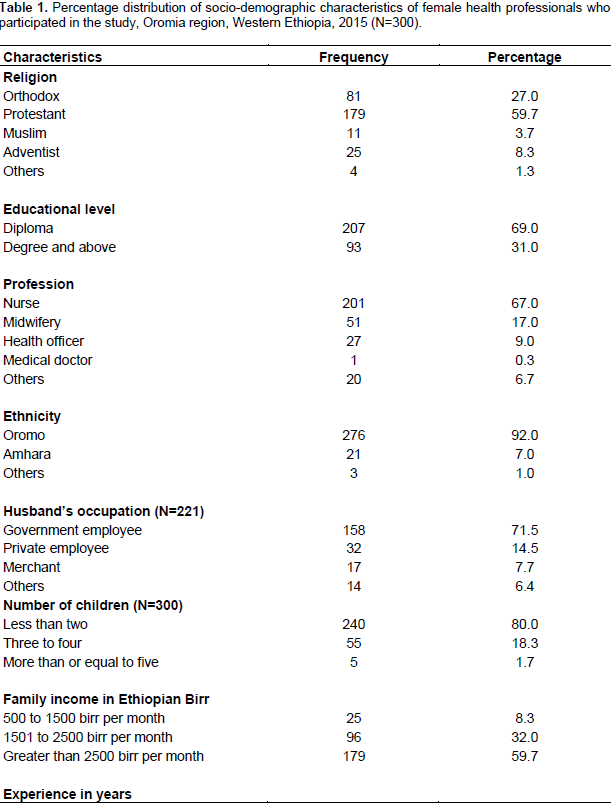
A total of 300 female health professionals were recruited, making (95.5%) response rate. Table 1 shows the socio-demographic profile of the respondents. The mean age of the respondents was 28.0±4.6 (ranging from 18-50 years). Almost three fourth (73.7%) of the study participants were married, 59.7% were protestant Christians and 92.0% were Oromo ethnic group.
History of breast and other body parts cancer
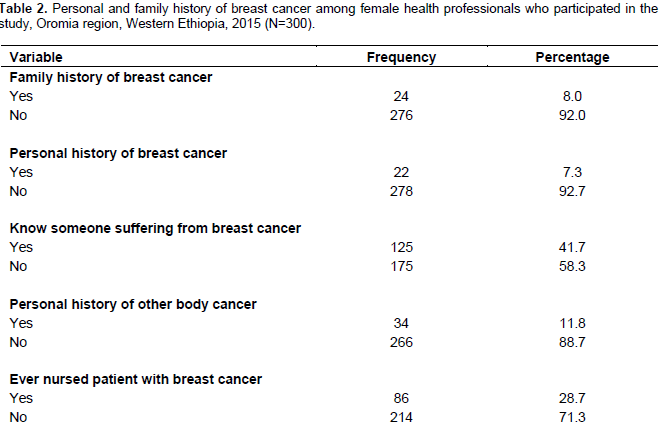
Table 2 shows personal and family history of breast cancer of the respondents. Among the total respondents, 8.0% reported that they had family history of breast cancer (that is, have a family member diseased or died of breast cancer) and 7.3% of them have personal history of breast cancer. On other hand, 41.7% of the respondents knew someone or patients suffering from breast cancer. reported they had and 28.7% of the participants have ever nursed patients with breast cancer.
Knowledge of health professionals on BSE
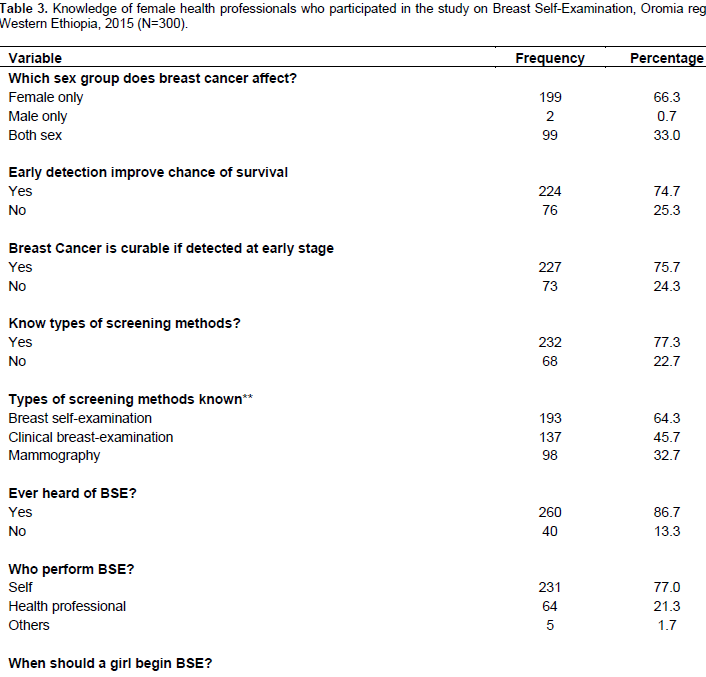
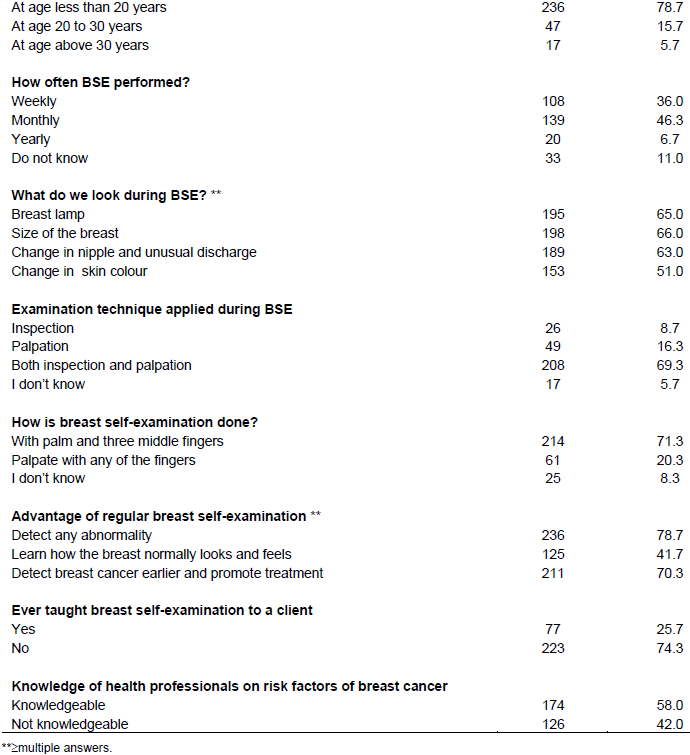
Table 3 shows the knowledge of the respondents on BSE. Among female health professionals that participated in this study, 66.3% of them reported that breast cancer affects only the female gender. Almost three fourth of the study participants (74.7%) knew early detection of breast cancer increases chance of survival and 76% reported that breast cancer is treatable if it is detected and diagnosed at an early stage. Among study participants, 77.3% of the respondents knew the types of screening methods. The methods of screening for breast cancer reported by health professionals were: BSE (64.3%), clinical breast examination (45.7%), and mammogram (32.7%). Almost one forth, 13.3% of the respondents have never heard about BSE. Only 15.7% of the respondents knew the age at which BSE should start and 46.3% of them indicated that BSE should be performed monthly. Almost all respondents (90.5%) wanted more information on BSE and breast cancer. They were more interested to receive more training and education about BSE. The knowledge of the respondents was assessed by using 15 questions. More than half (58.0%) scored the median (seven) and above value and regarded as knowledgeable and the remaining (42.0%) scored below the median and were not knowledgeable. From the total study participants, only 25.7% have ever counseled clients on BSE.
Attitudes of respondent toward BSE
As presented in Table 4, a set of 12 statements (attitude indicators/items) pertaining to attitude of respondents toward BSE was included in the questionnaire. Six positive and 6 negative items were included to maintain the balance of responses. The 12 items were answered as strongly agree, agree slightly, neither agree nor disagree, slightly disagree, and strongly disagree (on a five-point likert scale). For positively worded statements, those who selected strongly agree were regarded as having favorable (positive) attitude and those who choose ‘strongly disagree’ were considered as having unfavorable (negative) attitude. Similarly, for negatively worded statements, those who selected ‘agreed’ were clustered as having negative outlook whereas those who Concerning cancer of other body parts, 11.3% of them said ‘disagree’ were categorized as having positive attitude. The responses on each attitudinal items were scored, tallied, and then the total of each respondent score was made to range between 0 and 12 (0-100%). A score of 50% and above was considered as ‘favorable attitude’ whereas those that scored below 50% of the total were thought of as having ‘unfavorable attitude’. The summarized attitudinal index indicates that 59.7% of the total respondents had favorable attitude towards BSE.
Factors affecting BSE practice
In this study, factors associated with BSE were assessed. Predictor variables that showed association in bivariate analysis at p-value less than 0.05 were selected and included in the final logistic regression (multivariate analysis) model to control confounders. These factors include socio-demographic characteristics, history of breast cancer, knowledge and attitude of health professionals on BSE (Table 5) After adjusting for the other variables, personal history of breast cancer retains its association in multivariate regression. Professionals who had personal history of breast cancer were 5 times (AOR=4.7, 95%CI: 1.32, 17.07) more likely to perform BSE.
Those professionals knowledgeable on BSE were 4 times (AOR=4.2, 95%CI: 1.36, 5.65) more likely to examine their breast than those who were not knowledgeable, those study participants reporting teaching BSE to a client were 5 times more likely (AOR=5.2, 95%CI: 2.33, 8.14) to practice BSE than those who do not counsel clients on BSE. Those who had positive attitude toward BSE were four times more likely to perform BSE than who had negative attitude (AOR=3.8, 95%CI: 2.11, 9.17).
This study was conducted in order to assess the magnitude of BSE practice and its associated factors among female health professionals working in public health facilities in Western Ethiopia. In this study, 77% of respondents had ever performed BSE. This is almost similar with the results of a previous study done in Addis Ababa (75.1%) (Teferi et al., 2012). But, it is inconsistent with the findings of a study from Nigeria (89%) and United Arab Emirates (84.4%) (Odusanya et al., 2001; Sreedharan et al., 2010) and higher than a study conducted on Egyptian nurses (56.4%) (Karima and Ashraf, 2010). The difference observed could be due to the difference in socio-economic and demographic characteristics among the study population and difference in time interval between the studies. The finding implies that improving awareness among health workers on importance of BSE is very crucial to reach the community at large.
From those study participants who ever practiced BSE, only (33.7%) performed the practice on regular bases (monthly). The finding was consistent with studies done in Addis Ababa, Ethiopia (35.5%), in Turkey (28%) of the nurses and 32% of physicians did not practice BSE (Teferi et al., 2012; Demirkan et al., 2007). Likewise, in a cross-sectional study conducted in Iran, it was revealed that most of the female health care workers (63% to 72%) did not practice BSE (Haji-Mohammed et al., 2002). The finding of the study done in Nigeria and Sao Paulo was much higher than this study area (82 and 90.3%) respectively (Odusanya et al., 2001; Carelli et al., 2008). This could be due to the difference of educational level among the study participants.
In the present study, more than one fifth of respondents mentioned that they did not have breast problem, did not feel comfortable in doing BSE, are scared of being diagnosed with breast problem or cancer, they did not believe BSE is beneficial and they did not know how to perform BSE. The findings were similar to studies conducted among Norwegian female physicians and Jordanian nurses in Egypt who stated similar reason for not performing BSE (Alkhasawneh et al., 2009). In this study, 58.0% of the study participants were knowledgeable about BSE. This result is lower than studies done in Addis Ababa, Ethiopia (85%), Egypt (73%), and Nigeria (63%) (Teferi et al., 2012; Odusanya et al., 2001; Akhigbe and Omuemu, 2009). The difference may be due to difference in educational status, study area and accessibility to information, composition of the study population, accessibility to mass media and different reading materials.
In many findings, practice of BSE was determined by the knowledge of women or having information on diagnostic methods of breast cancer (Teferi et al., 2012; Karima and Ashraf, 2010; Sadler et al., 2001; Demirkan et al., 2007; Canbulat and Uzun, 2008). Similarly in the current study, participants who were knowledgeable on BSE were more likely to perform BSE. Having positive attitude toward BSE was also a significant predictor of BSE practice in this study which is consistent with other studies (Teferi et al., 2012; Seah and Tan, 2007). In a study done in Turkey, significant association was observed between breast cancer knowledge and practice of BSE (Cavdar et al., 2007).
In this study, the professionals who have personal history of breast cancer were five times more likely to examine their breast than others. In addition, women with a positive family history of breast cancer had a better knowledge as well as higher frequency of BSE than those with a negative family history (Kosgeroglu et al., 2011; Karayurt and ZorukoÅŸ, 2008). This could be due to their exposure to different health professionals and advise on BSE in noticing any change at early stage.
In the present study, female health professionals who ever taught BSE to a client were more likely to be engaged in practicing BSE. This could be due to different training they have had, self-commitments and exposure to different reading material to be equipped with knowledge for teaching others. The importance of education in the adoption of BSE practice has been reported repeatedly (Ravichandran et al., 2011; Rasu et al., 2011; Ceber et al., 2010). Simultaneously, the positive impact of educational interventions on BSE and breast cancer awareness have also been emphasized (Yavari and Pourhoseingholi, 2007; Venkatramana et al., 2011).
Strengths and limitations of the study
The response rate for the study was high. The behavioral study outcomes are based on self-reported information. Therefore, some information may not be reported honestly and possibility of underestimation cannot be ruled out. Some sort of desirability and recall bias may not be eliminated. The information collected quantitatively was not triangulated with qualitative method. Being cross sectional study design which does not show the cause effect relationship is the other limitation of the study. The lack of standardized questionnaire used to assess BSE practice may limit the comparability of the findings of this study with other studies.
Even though the life time BSE practice in this study was high, the regular BSE practice was low. Knowledge on BSE, positive attitude, engagement in teaching clients on importance of BSE and personal history of breast cancer were the factors found associated with BSE practice. Thus, trainings on BSE practice will be important to improve the practice level of health professionals and their counseling skill for the clients. In addition to this, more efforts are required in creating breast cancer awareness campaigns and screening programs at the grassroots in order to encourage early detection and diagnosis and enhance prevention strategies that would lessen the burden of breast cancer in Ethiopia.
The authors are grateful to Wollega University for the financial support of this study and research directorate office for the all-round support. They would like to acknowledge the East, West, Horro Guduru and Kellem Wollega Zone Health Bureaus and Health Facilities. Their appreciation also goes to the supervisors, data collectors and respondents (female health professionals) who generously and willingly participated in the study; without them this study would not have been achieved.
The authors have not declared any conflict of interests.
REFERENCES
|
Akhigbe AO, Omuemu VO (2009). Knowledge, attitudes and practice of breast cancer screening among female health workers in a Nigerian urban city. BMC Cancer 9(1):203.
Crossref
|
|
|
|
Azage M, Abeje G, Mekonnen A (2013). Assessment of factors associated with breast self-examination among health extension workers in West Gojjam Zone, Northwest Ethiopia. Int. J. Breast Cancer 2013:814395. Available at:
Crossref
|
|
|
|
|
Balogun MO, Owoaje ET (2005). Knowledge and practice of BSE among female Trader in Ibadan, Nigeria. Ann. Ibadan Postgraduate Med. 3(2):52-56
|
|
|
|
|
Bray F, Ren JS, Masuyer E, Ferlay J (2013). Global cancer prevalence for 27 sites in the adult population in 2008. Int. J. Cancer 132(5):1333-1145.
Crossref
|
|
|
|
|
Canbulat N, Uzun U (2008). Health beliefs and breast cancer screening behaviors among female health workers in Turkey. Eur. J. Oncol. Nurs. 12(2):148-156.
Crossref
|
|
|
|
|
Carelli I, Pompei LM, Mattos CS, Ferreira HG, Pescuma R, Fernandes CE, Peixoto S (2008). Knowledge, attitude and practice of breast self-examination in a female population of metropolitan São Paulo. Breast 17(3):270-274.
Crossref
|
|
|
|
|
Cavdar I, Akyoclu N, Ozbas A, Oztekin D, Ayoglu T, Akyuz N (2007). Determining female physicians' and nurses' practices and attitudes toward breast self-examination in Istanbul, Turkey. Oncol. Nurs. Forum 34(6):1218.
Crossref
|
|
|
|
|
Ceber E, Turk M, Ciceklioglu M (2010). The effects of an educational program on knowledge of breast cancer, early detection practices and health beliefs of nurses and midwives. J. Clin. Nurs. 19(15-16):2363-2371.
Crossref
|
|
|
|
|
Demirkan B, Alacacioglu A, Yilmaz U (2007). Relation of body mass index (BMI) to disease frees (DFS) and distant disease free survivals (DDFS) among Turkish women with operable breast carcinoma. Japanese J. Clin. Oncol. 37(4):256-265.
Crossref
|
|
|
|
|
Dye TD, Bogale S, Hobden C, Tilahun Y, Deressa T, Reeler A (2012). Experience of Initial Symptoms of Breast Cancer and Triggers for Action in Ethiopia. Int. J. Breast Cancer. Volume 2012 (2012), Article ID 908547. 5 p. Available at:
Crossref
|
|
|
|
|
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010). Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer 127(12):2893-2917.
Crossref
|
|
|
|
|
Fung S (1998) Factors associated with breast self-examination behaviour among Chinese women in Hong Kong. Patient Educ. Counseling 33(3):233-243.
Crossref
|
|
|
|
|
Ginseng GM, Lauer JA, Zelle S, Baeten S, Baltussen R (2012). Cost effectiveness of strategies to combat breast, cervical, and colorectal cancer in Sub-Saharan Africa and South East Asia: Mathematical modelling study. BMJ 344:e614.
Crossref
|
|
|
|
|
Hajiâ€Mahmoodi M, Montazeri A, Jarvandi S, Ebrahimi M, Haghighat S, Harirchi I (2002). Breast Selfâ€Examination: Knowledge, Attitudes, and Practices Among Female Health Care Workers in Tehran, Iran. Breast J. 8(4):222-225.
Crossref
|
|
|
|
|
Ibrahim NA, Odusanya OO (2009). Knowledge of risk factors, beliefs and practices of female healthcare professionals towards breast cancer in a tertiary institution in Lagos, Nigeria. BMC Cancer 9(1):76.
Crossref
|
|
|
|
|
International Agency for Research of Cancer (IARC) (2008). Breast Cancer Incidence, Mortality and Prevalence Worldwide.
|
|
|
|
|
Alkhasawneh IM, Akhuâ€Zaheya LM, Suleiman SM (2009). Jordanian nurses' knowledge and practice of breast self-examination. J. Adv. Nurs. 65(2):412-416.
Crossref
|
|
|
|
|
Karayurt O, ZorukoÅŸ SN (2008). Feel of women at a high risk for breast cancer and meeting, their needs for knowledge and support. J. Breast Health 4(2):56-61.
|
|
|
|
|
Karima FE, Ashraf MS (2010). Knowledge and practice of breast cancer screening among Egyptian nurses. J. Hematol. Oncol. 1(4):122-128.
|
|
|
|
|
Kosgeroglu N, Ayranci U, Ozerdogan N, Unsal A (2011). Knowledge of women on early diagnosis methods and risk factors for breast cancer in a province of Western Turkey: a descriptive study. Pak. J. Med. Sci. 27(3):646-650.
|
|
|
|
|
Odusanya O, Olufemi O, Tayo O (2001). Breast cancer knowledge, attitudes and practice among nurses in Lagos, Nigeria. J. Acta Oncologica 40(7):844-848.
Crossref
|
|
|
|
|
Rasu RS, Rianon NJ, Shahidullah SM, Faisel AJ, Selwyn BJ (2011). Effect of educational level on knowledge and use of breast cancer screening practices in Bangladeshi women. Health Care Women Int. 32(3):177-189.
Crossref
|
|
|
|
|
Ravichandran K, Al-Hamdan NA, Mohamed G (2011). Knowledge, attitude, and behavior among Saudis toward cancer preventive practice. J. Family Community Med. 18(3):135-142.
Crossref
|
|
|
|
|
Sadler GR, Dhanjal SK, Shah NB, Shah RB, Ko C, Anghel M, Harshburger R (2001). Asian-Indian women: knowledge, attitudes and behaviors toward breast cancer early detection. J. Public Health Nurs. 18(5):357-363.
Crossref
|
|
|
|
|
Seah M, Tan S (2007). Am I breast cancer smart? Assessing breast cancer knowledge among healthcare professionals. Singapore Med. J. 48(2):158-162.
|
|
|
|
|
Teferi S, Mezgebe T, Demissie M, Durgaprasada A (2012). Knowledge about breast cancer risk-factors, breast screening method and practice of breast screening among female healthcare professionals working in governmental hospitals, Addis Ababa, Ethiopia. IOSR J. Pharm. Biol. Sci. 2(1):5-12.
|
|
|
|
|
Sreedharan J, Muttappallymyalil J, Venkatramana M, Thomas M (2010). Breast self-examination: knowledge and practice among nurses in United Arab Emirates. Asian Pac. J. Cancer Prev. 11(3):651-654.
|
|
|
|
|
The American Cancer Society (AMS) (2014). Breast Cancer Prevention and Early Detection. Available at:
View
|
|
|
|
|
Venkatramana M, Sreedharan J, Muttappallymyalil J, Thomas M (2011). Opinion of nurses regarding breast cancer screening programs. Indian J. Cancer 48(4):423-427.
Crossref
|
|
|
|
|
Yavari P, Pourhoseingholi MA (2007). Socioeconomic factors association with knowledge and practice of breast self-examination among Iranian women. Asian Pac. J. Cancer Prev. 8(4):618-622.
|
|