ABSTRACT
The government of Ethiopia has been working in creating and increasing the number of open defecation free kebeles as a strategy of improving sanitation coverage in the country. However, apart from increasing sanitation coverage, data on utilization of the constructed latrines was not well investigated. Therefore, the study objective was to assess the latrine utilization coverage of the kebeles who have already declared open defecation free. Community-based cross-sectional study design with multistage sampling technique was employed. Data were checked, coded and entered into EpiInfo version 7 and analyzed using SPSS version 20. Bivariable and multivariable logistic regression model were fitted to identify factors associated with latrine utilization. Odds ratio with its 95% confidence interval was used as a measure of association. Eighty-three percent of the dwellers utilized their latrine. The odds of latrine utilization was higher among households which had latrine constructed after 2 years [AOR: 2.27; 95% CI: 1.23, 4.19], maintained latrine [AOR: 2.71; 95% CI: 1.61, 4.55], and had under-five children [AOR: 2.02; 95% CI: 1.24, 3.26]. However, households which had latrine constructed from wood and plastic [AOR: 0.44; 95% CI: 0.24, 0.81] and who constructed their latrine looking at their friends [AOR: 0.35; 95% CI: 0.18, 0.68] were less likely to use their latrine. The extent of latrine utilization is high in the community. Further strengthening of implementation modalities giving due consideration for the aforementioned factors is highly recommended.
Key words: Latrine utilization, open defecation free, cross sectional, Ethiopia.
Open defecation free (ODF) is a term used to describe either community that has eliminated the practice of open defecation or households which no longer defecate in the open. It can be used to describe the actual state of having no open defecation or the point at which a community or household are declared to have reached this state (Water-Aid, 2009). Proper use of improved sanitation facilities can help to prevent the multiplicity of diseases that are transmitted through human faeces, including intestinal worms and other neglected tropical diseases (Taiji, 2012). Poor sanitation and water supplies are the engines that drive cycles of disease like bacteria, viruses and parasites, which are major causes of diarrhea and other diseases (Water-Aid, 2009). Inadequate access to sanitation facilities resulting in the practice of widespread open defecation has a negative impact on the health of the community (Kamal, 2005). Poor waste disposal practices are responsible for a significant proportion of the world's infectious disease burden (WHO, 2003).
Globally, in 2010, an estimated 2.5 billion people were still living without improved sanitation and 15% of the population still practice open defecation, which represents 1.1 billion people (WHO, UNICEF, 2013). Open defecation is largely a rural phenomenon, most widely practiced in Southern Asian and sub-Saharan Africa (WHO, UNICEF, 2010). In sub-Saharan Africa, in 2010, 45% of the population uses either shared or unimproved facilities, and an estimated 25% practice open defecation (WHO, UNICEF, 2012). The region made the least progress, ‘having lowered the proportion of its population engaged in unsanitary practices by roughly 15% (Taiji, 2012). Unless the speed of movement of change in the sanitation sector is accelerated, the Millennium Development Goal (MDG) sanitation target may not be achieved until 2026 (WHO, UNICEF, 2013). In the WHO African Regions, 40% of Nigeria, Niger, and Cameroon people had no access to any kind of improved sanitation facilities (WHO, UNICEF, 2010).
Building improved sanitation facilities is a crucial health intervention to realize proper use and maintenance of the facilities and good personal and domestic hygiene. Sanitation facilities interrupt the transmission of fecal-oral disease at its most important source by preventing human faecal contamination of water and soil (WHO, 2003). Diarrheal disease is a major cause of death in sub-Saharan Africa due to lack of improved sanitation practice and those who practice open defecation are the riskiest group for sanitation related disease (Savadogo, 2013).
According to Ethiopian Mini-Demographic Health Survey (EMDHS) 2014 report the majority of households, 89% use non-improved latrine facilities (CSA, 2014), and 38% of households have no toilet facility. Most commonly used non-improved toilet facility is an open pit latrine or pit latrine without slabs was used by 57% of households in rural areas and 43% of households in urban areas and about 7% of households use shared toilet facilities (CSA, 2011).
In Ethiopia, about 60% of the current disease burden is the result of poor sanitation, and diarrhea among under-five children accounts for 15% of the total deaths (FDRE, MOH, 2005). Even though the government has placed two interventional programs, the introduction of health extension program since 2004 and community-led total sanitation and hygiene (CLTSH) programs, the changes that have been recorded so far have not brought change in latrine utilization as required (WHO, UNICEF, 2014; CDC, 2008; Barnard et al., 2013; Kema et al., 2012; Paul et al., 2013). Therefore, it is believed that the gap in utilization required further study.
The objective of this study, therefore, was to determine the magnitude and to identify potential factors associated with latrine utilization in Wondo Genet district.
A community-based cross-sectional study was conducted in Wondo Genet district, Southern Ethiopia from March 2015 to April 2015. This study was conducted in Wondo Genet district which is located in Southern Ethiopia. Wondo Genet district has an estimated population of 154,510 and 30,215 households (Wendo Genete District, 2015). The capital town of Wondo genet district is Chuko, which is located at 24 km far from the regional state capital city (Hawasa). The district is divided into 14 rural kebeles (the lowest administrative unite in Ethiopia), and 2 rural towns. There are 13 health posts, 13 clinics and 3 health centers making health coverage of the district 63%. Because of governmental and non-governmental efforts made so far, the kebeles declared open defecation free.
The study population were all households in the district. The necessary sample size (n) was computed by single population proportion formula:
by assuming 95% confidence level of za/2= 1.96, margin of error 5%, design effect 2, proportion (p) of latrine utilization 61.2% according to the previous similar study conducted, and non-response rate 5%. The calculated sample was 759. Multi-stage sampling technique was employed to select the study participants. Five kebeles (the lowest administrative structure) were selected randomly. The total determined sample size was proportionally allocated for each kebele’s and systematic random sampling (K=15) was used to select the final household.
A structured questionnaire supported with observational checklist was used to collect the required data. A face to face interview and observation of latrine usage was conducted to collect the data. The data collection instrument was first prepared in English language and then translated into Amharic and finally, it was retranslated into English by language experts to check its consistency. Data collectors with diploma and B.Sc. rank and three supervisors which had B.Sc. in Environmental health were selected and trained. A pre-test was done before engaging in full implementation of data collection by taking 5% of the sample size in kebeles adjacent to the study kebeles for assuring data quality.
Data were entered to Epidemiological Information (EPI-INFO) software version 3.5.1 and analyzed by Statistical Package for Social Sciences (SPSS) software version 20. A backward binary logistic regression model was used to identify factors associated with latrine utilization. Both Crude Odds Ratio (COR) and Adjusted Odds Ratio (AOR) were used to show an association between hypertension and selected variables at 95% confidence interval (CI). Variables having a p-value≤0.05 in the final model were assumed to be significant determinants. Model fitness test was checked by the Hosmer and Lemeshow goodness of fit test.
Socio-demographic characteristics
The households included in the study were from five kebeles of Wondo Genet district. A total of 744 households were included with a response rate of 98.03%. Of the total respondents, 81.9% were females. The mean age of the respondents was 40.79 (±SD) of 11.36 years. Most, 64% of households had a family size of greater or equal to 5 persons. Under-five children were found in 202 (27.2%) of households (Table 1).
Sanitation/Latrine facilities
Almost all 727 (98.9%) types of available latrines were simple pit latrines followed by ventilated improved pit latrine 8 (1.1%). Half, 381 (51.8) of the latrine were constructed before two years. Almost, 692 (94.1%) of latrine were functional, among this, 413 (56.2%) latrines need maintenance. Twenty-eight (3.8%) of latrines had no superstructure and 1.5% of the latrines need maintenance. The majority, 92.7% of the latrine had pit slabs, among this, 65.6% of the latrine slab was made of wood with mud (Table 2).
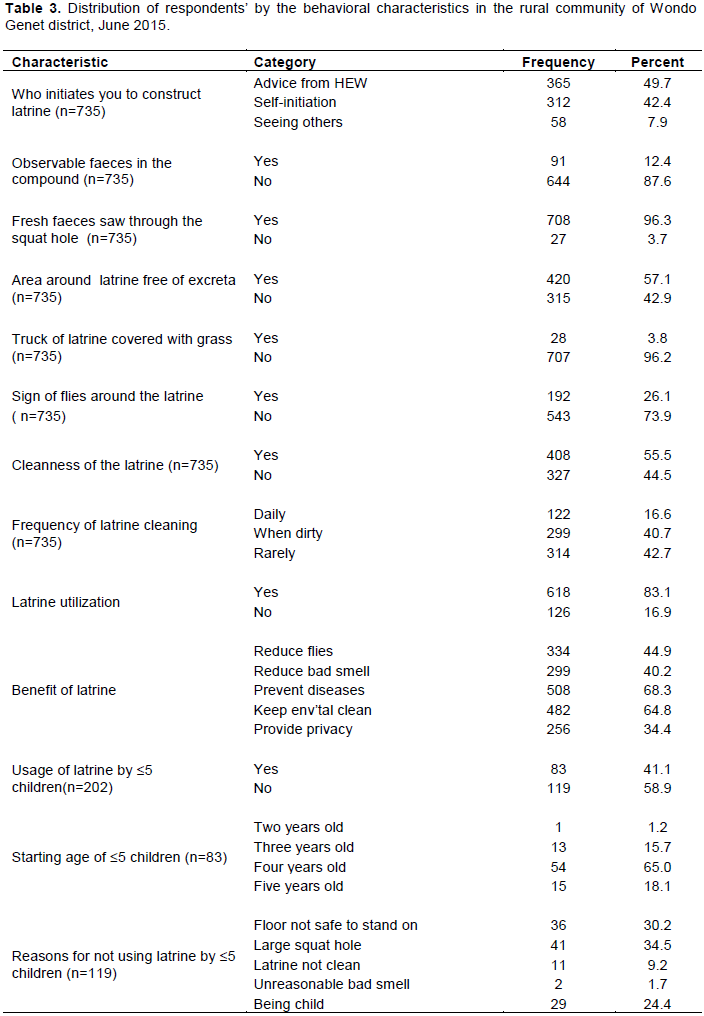
Behavioral factors
About half 365 (49.7%) of the households who had latrine were advised by health extension workers to construct their latrines, while few 15 (2%) of the households had imposed by other bodies like local administrative officials. Almost all, 725 (98.6%) of households explained that all family members were using the latrine (Table 3).
Latrine utilization and associated factors
Latrine usage was observed among 618 (83.1%) of the households. Only 91 (12.4%) of households had observable feaces in the compound. Majority 708 (96.3%) of the household latrine had observable fresh feaces in the squat hole of the latrine.
Selected variables that were significantly associated at the bi-variable analysis were further examined in the multiple logistic regressions to see their relative effects on the extent of latrine utilization. The factors that were found to have association during multivariable logistic regression with latrine utilization were the duration of latrine construction, the condition of latrine super-structure, reasons of initiation for latrine construction, the status of the latrine, presence of ≤5 children and age of the head of the household.
The extent of latrine utilization was 56% [AOR: 0.43, 95%CI: 0.24, 0.76] less among those households who use latrine constructed within the last two or lesser years as compared to latrine constructed before two years. Those households who had latrine superstructure made up of wood and plastic were 56% [AOR: 0.44; 95%CI: 0.25, 0.81] lesser to utilize their latrine as compared to households with latrine facility superstructure made up of wood and locally available material like “enset kitel”.
Households who construct their latrine following seeing others were 65% [AOR: 0.35; 95%CI: 0.18, 0.68] less likely to utilize their latrine than those of households constructed their latrine followed advice by Health Extension Workers (HEW). The odd of latrine utilization was 2.71 [AOR: 2.71; 95%CI: 1.61, 4.55] times higher among households with maintained latrine compared to households whose latrine needs maintenance.
Similarly, the odd of latrine utilization among households who had ≤5 children was 2.02 times higher as compared to households who had not ≤ 5 children [(AOR: 2.02 (1.25, 3.27)] (Table 4).
This study found that the rate of latrine utilization among open defecation free kebeles in the rural community of Wondo Genet district is about 83.1% (95% CI: 80, 86), which is higher than a study conducted in the community of Hulet Ejju Enessie district, East Gojam Zone 60.7% and Denbia district, Northwest Ethiopia 61.2% (Yimam et al., 2014; Andualem and Abera, 2010). On the other hand, the coverage was lower than the study conducted in Alaba and Mirab Abaya district SNNPR 91.1% (Tefera, 2008). This variation might be explained by the fact that the study community would have differences in socio-cultural background, time of studies conducted and difference in intervention modalities among these study areas.
The current study also identified factors for latrine utilization in the studied community: duration of latrine construction (year of latrine service), the condition of latrine superstructure, reasons of initiation for latrine construction (how the households told about the latrine during construction), the status of the latrine, the presence of ≤5 children in the household and age of the head remain significant predictors of latrine utilization.
The study has revealed the reason for initiation of latrine construction has a vital role for utilization of toilet facilities. Households which constructed their latrine following others were 65% less likely to utilize their latrine as compared to households which got HEW’s advice. This finding is supported by a similar study conducted at Awabel district, Northwest Ethiopia (Awoke and Muche, 2013) which revealed the importance of HEWs in disseminating sanitation and hygiene related messages.
Similarly, the current study revealed that latrine utilization practice was 56.7% less among the household that had a latrine which was constructed within the last two years. This finding is in line with a study conducted in Hulet Ejju Enessie and Gulomekada districts (Yimam et al., 2014; Gedefaw et al., 2015). The newer latrine might be constructed after the household's knowledge about latrine utilization was improved. On top of that, the newer latrine might keep user’s privacy and the quality of the latrine might also motivate the household to use their latrine efficiently. The extent of latrine utilization was also 2.02 times higher among households who did not have under-five children. This may be due to the fact that under-five children are unable to use the available latrine design and they mostly defecate their faeces near to the latrine area. However, this finding is the reverse of the findings of a study conducted in Denbia district in which the odds of latrine utilization is higher among households having under five children (Yimam et al., 2014).



Sanitation facilities must be properly maintained to function properly and the use of inappropriate materials for latrine construction leads to the collapse of the latrine due to various reasons (such as loose soil condition, flooding, etc.) necessitating frequent maintenance (Debesay et al., 2013; FDRE, MoH, 2004). In this study, the odd of latrine utilization was 2.71 times higher among a household who had a maintained latrine. The finding of this result was consistent with a study conducted in Awabel district (Awoke and Much, 2013). In this study, 56.2% of the latrine facilities need complete maintenance and repair of their superstructure. This figure was similar to study conducted in Bahir Dar Zuria district (56.9%) (Tefera, 2008) and lower than the finding by Hawzien district Tigray (69%) (FDRE, MoH, 2010).
According to the data observed in this study, utilization of latrine was affected by the condition of latrine superstructure; those households whose latrine superstructure was made from wood and plastic were 55.6% less likely to utilize their latrine. The cost of using locally available materials would help the households to construct their latrine easily and to use them as well. This finding is in line with a study conducted in Awabel district (Awoke and Muche, 2013). Since the study is on utilization of latrine, recall bias and social desirability bias might have overestimated some of the findings.
This study found that the rate of latrine utilization in the rural community of Wondo Genet district is found to be high. Duration of latrine construction, the condition of latrine superstructure, reasons of initiation for latrine construction, the status of the latrine, and the presence of children less than five years in the household are factors associated with latrine utilization. Attention should be given to the identified factors in order to sustain and improve latrine utilization in the community.
The authors have not declared any conflict of interests.
The University Gondar College of Medicine and Health Science and Southern Nations Nationalities and People Regional Health Bureau are acknowledged for the financial support. The field supervisors, data collectors, the study participants and health department of the administration are appreciated for the support during project implementation.
REFERENCES
|
Andualem A, Abera K (2010). Assessment of the impact of latrine utilization on diarrhoeal diseases in the rural community of Hulet Ejju Enessie Woreda, East Gojjam Zone, Amhara Region Ethiopia; Journal of Health Development 24(2):110-8.
|
|
|
|
Ashebira Y, Sharmab HR, Alemu K, Kebede G (2015). Latrine use among rural households in northern Ethiopia: a case study in Hawzien district, Tigray. Available at:
View
|
|
|
|
|
Awoke W, Muche S (2013). A cross-sectional study: latrine coverage and associated factors among rural communities in the District of Bahir Dar Zuria, Ethiopia. BMC Public Health 13:99.
Crossref
|
|
|
|
|
Barnard S, Routray P, Fiona Majorin, Peletz R, Boisson S, Sinha A (2013). Impact of Indian Total Sanitation Campaign on Latrine Coverage and Use: A Cross-Sectional Study in Orissa: Three Years following Programme Implementation.
|
|
|
|
|
Communicable Disease Control (CDC) (2008). Global Water, Sanitation and Hygiene. Available at:
View
|
|
|
|
|
Central Statistics Authority (CSA) (2011). Ethiopia Demographic and Health Survey Addis Ababa, Ethiopia. ICF International Calverton, Maryland, USA. pp. 16-37.
|
|
|
|
|
Central Statistics Authority (CSA) (2014). Ethiopia Mini Demographic and Halth Survey Addis Ababa, Ethiopia. Available at:
View
|
|
|
|
|
Debesay N, Ingale L, Gebresilassie A, Assefa H, Yemane D (2013). Latrine Utilization and Associated Factors in the Rural Communities of Gulomekada District, Tigray Region, North Ethiopia: A Community-Based Cross-Sectional Study. Journal of Community Medicine & Health Education 5:338.
|
|
|
|
|
FDRE, MoH (2004). Construction Usage and Maintenance of Sanitary Latrine Extension Package.
|
|
|
|
|
FDRE, MOH (2005). National Hygiene and Sanitation Strategy to Enable 100% Adoption of Improved Hygiene and Sanitation.
|
|
|
|
|
FDRE, MoH (2010). Hygiene and Environmental Health, part-2 blended learning module for the health education program. Ethiopian Federal Ministry of Health. Available at:
View.
|
|
|
|
|
Gedefaw M, Amsalu Y, Tarekegn M, Awoke W (2015). Opportunities and Challenges of Latrine Utilization among Rural Communities of Awabel District, Northwest Ethiopia, 2014. Open Journal of Epidemiology 5(02): 98.
Crossref
|
|
|
|
|
Kamal K (2005). A practical guide for use by frontline extension staff, based on the experience of facilitating community-lead-total sanitation in at least eight different countries in South and South East Asia and in East Africa.
|
|
|
|
|
Kema K, Innocent S, Serafina M, Ignatio K, Florence T, Festus I, Martin M (2012). Factors affecting the utilisation of improved ventilated latrines among communities in Mtwara Rural District, Tanzania. The Pan African Medical Journal 13 (Supp 1):4.
|
|
|
|
|
Paul TB, Matthew B, Ross K (2013). Open Defecation Free Sustainability Study by Plan International. Available at:
View
|
|
|
|
|
Savadogo AS (2013). Monitoring sanitation in Africa Ongoing initiatives and lessons from the field. Sanitation and Hygiene in Africa: Where do We Stand?, p.165.
|
|
|
|
|
Taiji SB (2012). Global Access to Clean Drinking Water and Sanitation: U.S. and International Programs. Report R42717. Washington, DC: Congressional Research Service.
|
|
|
|
|
Tearfund, WaterAid. The Human Waste A call for urgent action to combat the millions of deaths caused by poor sanitation A. Available at:
View.
|
|
|
|
|
Tefera W (2008). Research-inspired Policy and Practice Learning in Ethiopia and the Nile region Technical issues of Sanitation and Hygiene in Mirab Abaya and Alaba A case study report from the Southern Nations Region ('SNNPR') of Ethiopia.
|
|
|
|
|
Water-Aid (2009). Sustainability and equity aspects of total sanitation programmes. A study of recent WaterAid-supported programmes in three countries.
|
|
|
|
|
Wendo Genete District (2015). Yearly report of health services (unpublished).
|
|
|
|
|
World Health Organization (WHO) (2003). People and waste: the size of the problem. Water sanitation and health. Water, Environment and Sanitation. Available at:
View
|
|
|
|
|
WHO, UNICEF (2010). The Global Water Supply and Sanitation Assessment. Available at:
View
|
|
|
|
|
WHO, UNICEF (2012). Progress on drinking water and sanitation: update: UNICEF and World Health Organization pp. 20-30.
|
|
|
|
|
WHO, UNICEF (2013). Progress on sanitation drinking water: update: UNICEF and World Health Organization. Available at:
View
|
|
|
|
|
WHO, UNICEF (2014). Progress on drinking water and sanitation: update: UNICEF and World Health Organization. Available at:
View
|
|
|
|
|
WHO, UNICEF (2014). The WHO/UNICEF Joint Monitoring Programme for Water Supply and Sanitation is charged with international reporting on progress towards the MDG drinking water and sanitation target.
|
|
|
|
|
Yimam TY, Kassahun AG, Daniel HC (2014). Latrine utilization and associated factors among people living in rural areas of Denbia district, Northwest Ethiopia: A cross-sectional study. The Pan African Medical Journal18:334.
Crossref
|
|