Epidural abscess is a rare condition, with increasing incidence, but still underdiagnosed. Clinical set is often confused with common diseases, which delays the diagnosis and may progress to irreversible neurological sequelae or death, if no early intervention is taken. We have reported a case of a patient immunosuppressed by diabetes who developed an epidural abscess due to a complicated pyelonephritis.
Epidural abscess is a rare cause of low back pain (Bremer and Darouiche, 2004; Sendi et al., 2008). Nowadays, because of higher life expectancy, greater prevalence of spine invasive procedures and significant improvement in the sensitivity of imaging methods, the diagnosis is about 0.2 to 1.2 cases per 10,000 hospital admissions per year (Darouiche et al., 1992; Grewal et al., 2006). Due to an unspecific symptomatology, and many times with no specific neurologic signs, it turns into a challenging diagnosis (Sendi et al., 2008). We reported the case of a diabetic patient with persistent low back pain and fever despite prolonged treatment for complicated pyelonephritis, which turned to be an epidural abscess. All data was collected from direct consultation of patient chart and the patient has given his informed consent for the case report to be published.
A 64-year-old black male, resident of Rio de Janeiro, presented to the emergency department with a three day history of left lower back pain with no previous trauma, associated with a body temperature of 102°F and chills. He was already on treatment with ciprofloxacin and clindamycin 500 mg both twice a day (BID) for one day, prescribed as empirical remedy for urinary tract infection. He had a past medical history of poorly controlled arterial hypertension with atenolol and losartan potassium 25 mg both BID and type 2 diabetes mellitus with metformin 850 mg BID demonstrated by the macrovascular complications (he has had a left hallux amputation) as a result of low adherence to treatment. His social history was positive for alcohol consumption (9 units of ethanol per week), but with no use of illicit drugs.
At examination, he was febrile with 100°F, pulse was 94/min, and blood pressure was 180/80 mmHg. His capillary glucose was 515 mg/dl. He was pale 2+ and malaise. There were no breath sounds on both pulmonary bases. Cardiovascular system showed a fourth heart sound. Giordano and psoas signs were present on left side. Otherwise, he was normal, with no findings suggestive of neurologic deficits. Laboratory results on admission (06/16/14) and on the following months are presented in Table 1.
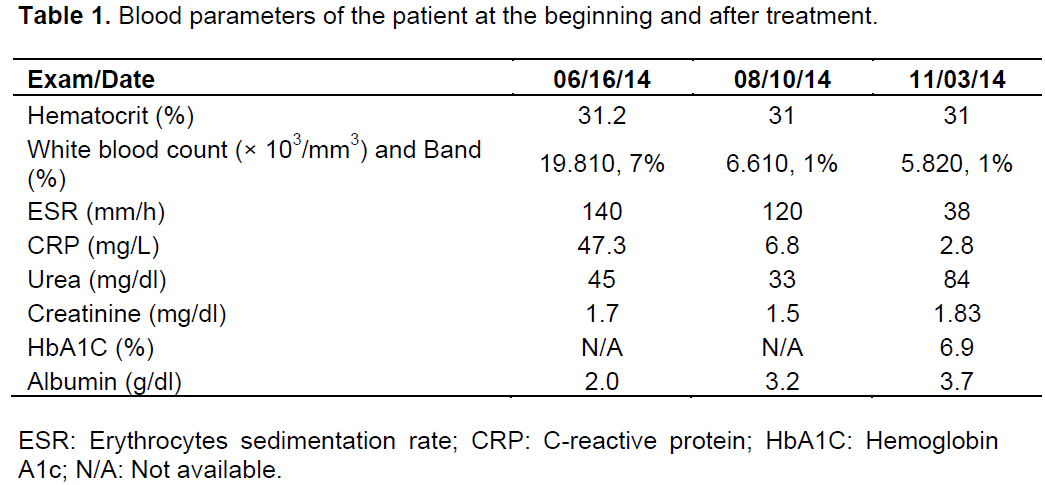
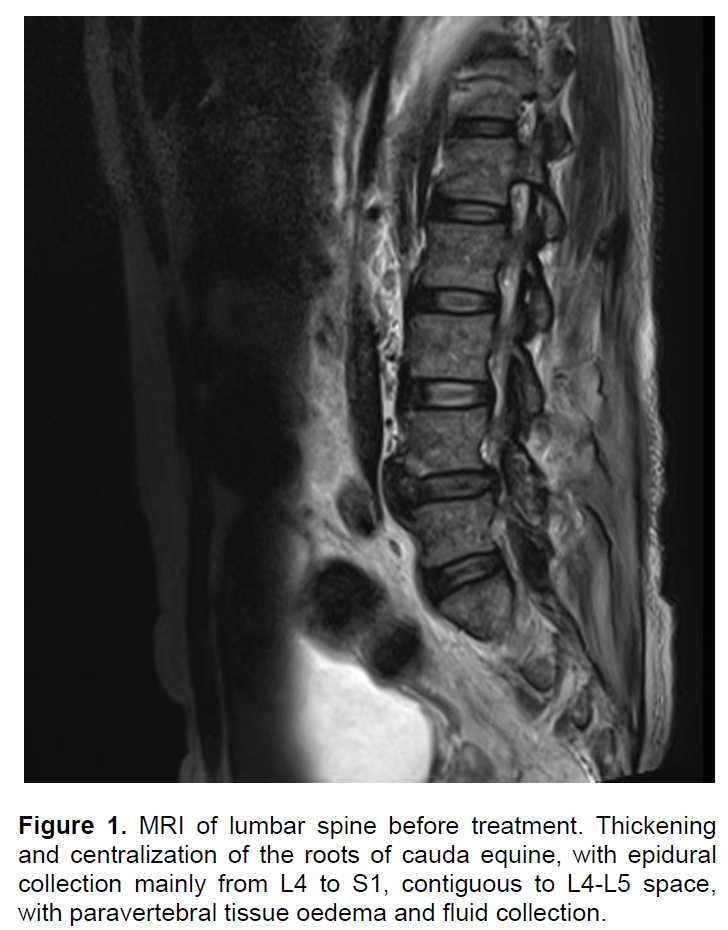
Due to the suspicion of urinary tract infection, after 5 days of quinolone, the antibiotic was changed to a broader spectral antimicrobial for gram negative germs - piperacilin/tazobactam for 14 days. Blood and urine cultures were all negative before and after treatment, his erythrocyte sedimentation rate was high (Table 1) and the symptoms persisted with daily fever, back pain, and loss of apetite. Protein immunoeletrophoresis test revealed a polyclonal pattern not confirming multiple myeloma. Transthoracic echocardiogram showed no evidence of infectious endocarditis. Polymerase chain reaction urinary, repeated sputum studies and blood cultures were all negative for mycobacteria. X-ray computed tomography (CT scan) of abdomen and vertebral column on admission suggested inflammatory process bilaterally around kidneys and degenerative disease of the vertebral bodies, with no evidence of bone or soft tissue infection. A magnetic resonance imaging (MRI) of the back with intravenous gadolinium was then performed, and showed loss of normal disc space, with oedema and fluid collection on paravertebral muscles and cauda equina. After thirty days of hospitalization, he was submitted to surgical drainage and then empirically started an eight-week therapy with full-dose of vancomicin and meropenem. Drained material from the paravertebral fluid collection was sterile and had a non-purulent aspect. After eight weeks of treatment, he gained weight, had no more fever and no restrictions to walk. He was finally discharged after 110 days with no complains at all. On outpatient follow-up, a repeated MRI showed residual alterations and significant reduction of the fluid collection (Figure 1).
Epidural abscess may have different clinical symptoms, and can be misdiagnosed as other causes of back pain, either infectious (osteomyelitis, discitis, meningitis), or non-infectious (herniated disc, neoplasias, demyelinating disease, transverse myelitis), especially if the patient does not have neurologic signs (Nussbaum et al., 1992; Grewal et al., 2006; Pereira and Lynch, 2005). It is more common in men in their fifth decade of life, with a prevalence of 2 to 25 cases per 100,000 admissions (Darouiche et al., 1992). Main risk factors are diabetes mellitus, alcoholism, HIV, back trauma, tattoo, acupuncture, skin and soft tissue infections, bacteremia and use of intravenous drugs (Bremer and Darouiche, 2004; Reihsaus et al., 2000). In the present case, there was correspondence to the presence of diabetes and an infectious trigger (pyelonephritis). Poorly controlled diabetic patients are more susceptible to staphylococcal infections due to the disabled lymphocytic and phagocytic activity (Nussbaum et al., 1992).
Generally, this disease is followed by constitutional symptoms such as fever and asthenia. Only in few patients, the classic triad of persistent fever, back pain and neurological deficits may be found (Bremer and Darouiche, 2004). As a result, the delay in diagnosis may lead to gradual progression of symptoms; lower back pain, radicular pain, weakness of the lower limbs and sensory deficits, up to complete paralysis, that may be irreversible if not promptly treated (Reihsaus et al., 2000). Fever is considered as a warning, since it is not found in common conditions, such as osteoarthritis (Reihsaus et al., 2000; Sendi et al., 2008). Spinal epidural abscess or vertebral osteomyelitis could be diagnosed when compatible radiological images are available, or if there is no clinical improvement after usual treatment. The patient in this case did not have any clinical improvement after intravenous broad-spectrum antibiotics, with persistence of low back pain, physical restriction and daily fever.
The spread of epidural abscess may be haematogenic, by contiguity from nearby infected tissues (vertebral body or psoas muscle) or by direct inoculation (compression, thrombosis and thrombophlebitis, ischemia or inflam-mation of the spinal cord). The most prevalent pathogens are Staphylococcus aureus (57 to 93%), Streptococcos sp. (18%) and Gram-negative bacilli (13%) (Darouiche et al., 1992; Davis et al., 2004). About 30% of patients did not have identifiable source of infection, 22% enters through soft and skin parts, 22% after invasive procedures and 10% by hematogenous spread due to intravenous drugs (Darouiche et al., 1992). Although 62% of blood cultures gives a positive result, 90% of abscesses material and 19% of the liquor can result in a specific germ (Angtuaco et al., 1987; Reihsaus et al., 2000; Sendi et al., 2008). The most common site of infection is the thoracolumbar region, due to the greater presence of fatty tissue, vascularization and lower adherence of the dura mater to the cord, as observed in this case (L4 to S1) (Grewal et al., 2006; Mampalam et al., 1989; Simpson et al., 1999).
Analyses of laboratories usually show leukocytosis and positive inflammatory markers (high erythrocyte sedimentation rate and c-reactive protein) in most cases (Bremer and Darouiche, 2004; Nussbaum et al., 1992; Tang et al., 2002). If available, cerebrospinal fluid shows hyperproteinemia and pleocytosis (Nussbaum et al., 1992). The patient in this case had elevated values for inflammatory parameters, although blood cultures and urine cultures were negative.
Epidural abscesses may contain purulent material in acute cases. At the time of surgical drainage, it is common to detect granulation tissue, a finding that may suggest a process longer than two weeks (Darouiche et al., 1992; Reihsaus et al., 2000). The material from surgical drainage in the present case showed only granulation tissue and therefore the culture was also negative probably due to previous antibiotic therapy. Magnetic resonance image (MRI) of the spine with gadolinium offers sensitivity close to 90%, with better definition of the inflammatory process as the location and extent, including the early stages of infection. In the present case, the first available exam was a CT scan, which showed densification and anterior and posterior fluid collection around the kidneys, in addition to the thickening of the surrounding soft tissue.
Treatment choices rely on the clinical condition of the patient, but general rule is that decompression laminec- tomy with drainage is the best alternative in cases of neurological paralysis (Nussbaum et al., 1992). If the paralysis persists for more than 36 to 48 h, nonsurgical approach is recommended (Mampalam et al., 1989). In cases without acute neurological involvement, diagnostic aspiration followed by antibiotic therapy for 4 to 8 weeks may be a reasonable choice (Angtuaco et al., 1987; Bremer and Darouiche, 2004). Prolonged courses (around 6 weeks) are preferred due the presence of associated vertebral osteomyelitis. In this case, because of the insidious course without acute neurological complaints, the choice was drainage and then treatment with antibiotics.
Empirical antibiotic therapy should cover staphylococci (usually vancomycin in a dose of 30 to 60 mg/kg/day intravenously), and due to the potentially serious implications, or in the presence of urinary infection, combination with a third or fourth generation cephalosporin to cover gram-negatives is recommended. When the causative agent is identified by the cultures, the schemes should be simplified and targeted. The patient in this case received vancomycin and meropenem for eight weeks, since he had already tried other schemes including broad spectrum antibiotics and had a prolonged hospitalization.
Most common complications of epidural abscess are neurological (60% may persist with some motor weakness), and in a percentage of 4 to 22% may persist leading to irreversible neurological damage (especially if the diagnosis is delayed) (Davis et al., 2004; Grewal et al., 2006). Others include pressure ulcers, urinary tract infection, deep venous thrombosis and pneumonia, and up to 5% of patients may die (Reihsaus et al., 2000). In the present case, at the end of his treatment, the patient developed severe sarcopenia and kept motor weakness in the lower limbs due to prolonged hospitalization.
This report reinforces the importance of considering epidural abscess, an underdiagnosed disease, as a differential diagnosis in the approach of patients with low back pain.