ABSTRACT
Mother-to-child transmission (MTCT) of human immune virus/acquired immune deficiency syndrome (HIV/AIDS) is the largest mode of HIV transmission among children. This study assesses the prevention of mother to child transmission (PMTCT) of HIV/AIDS service utilization and associated factors among mothers attending antenatal care (ANC) in selected public health facilities of Horo Guduru Wollega Zone, Oromia Region, Ethiopia. Facility-based cross sectional study was conducted among mothers attending ANC in five public health facilities of Horo Guduru Wollega Zone from February to March, 2016. Randomly selected four health centers and one public hospital were included in the study. The study participants from each health facility were recruited by using systematic sampling technique. Exit interviews were conducted among mothers attending ANC services. Bivariate and multiple logistic regression analyses were performed to identify factors associated with PMTCT service utilization of mothers. A total of 378 pregnant mothers having antenatal visit during the study period participated in the study. All of the study participants were offered HIV counseling and testing at that particular antenatal visit. Among these, 317 (83.8 %) were counseled and tested for HIV as part of PMTCT service. Age, residence, mother’s educational status, male partner involvement during antenatal HIV testing, and service providers’ perceived handling of clients were associated with PMTCT service utilization of mothers. The utilization of HIV testing as PMTCT service in this study was lower when compared to the national recommendation set forth in the national PMTCT guideline, which recommends that every pregnant woman coming for ANC visit to health facilities should get HIV counseling and testing.
Key words: Prevention of mother to child transmission (PMTCT), HIV/AIDS, Horo Guduru Wollega Zone, Ethiopia.
Abbreviation:
AIDS, Acquired Immune Deficiency Syndrome; ANC, antenatal care; AOR, adjusted odds ratio; ART, antiretroviral treatment; ARV, antiretroviral; BSS, behavioral surveillance survey; C.I, confidence interval; COR, crude odds ratio; FHAPCO, federal HIV/AIDS prevention and control office; FHI, Family Health International; HCT, HIV counseling and testing; HIV, Human Immunodeficiency Virus; KM, kilometer; MDG, Millennium Development Goal; MTCT, mother-to-child transmission; PMTCT, prevention of mother-to-child transmission; SD, standard deviation; SDG, sustainable development goal; UNAIDS, United States Agency for International Development; UNICEF, United Nations Children’s’ Emergency Fund; VCT, Voluntary Counseling and Testing; WHO, World Health Organization.
Globally, an estimated 36.7 million (30.8-42.9 million) people were living with HIV in 2016, of which 17. 8 million (15.4-20.3 million) were women and 2.1 million (1.7-2.6 million) children under 15 years of age. An estimated 1.0 million (830,000-1.2 million) AIDS related deaths occurred globally in 2016, of which 120,000 (79,000-160,000) were children under 15 years of age. The burden of the epidemic continues to vary considerably among regions with 25.6 million people living with HIV in 2016 living in Africa alone, which accounts for nearly 70% of the overall global burden (WHO, 2016, 2017). The vast majority of this number occurring in Sub-Saharan Africa, low- and middle- income countries (AVERT, 2017).
According to the Federal HIV/AIDS Prevention and Control Office (FHAPCO), 741,478 people are living with HIV, with 16,865 AIDS related deaths in Ethiopia in the year 2015 (FHAPCO, 2015). The pediatric HIV population in Ethiopia are mostly those vertically infected in earlier years when MTCT rates were high but the coverage and effectiveness of PMTCT in the country was low (FDRPCO, 2014).
Mother-to-child transmission (MTCT) of human immune virus (HIV) refers to the transmission of HIV from an HIV-positive woman to her child during pregnancy, labour, delivery or breastfeeding. It can take place in utero, during labour, delivery and postnatally through breastfeeding [WHO, 2010]. It is the most common way that children become infected with HIV (WHO/PMTCT, 2016). Ninety-five percent of HIV infected children acquired the infection through mother-to-child transmission during pregnancy, around the time of labour and delivery, or during breast feeding (WHO/UNICEF, 2007). Mother-to-child HIV transmission (MTCT) accounts for the vast majority of more than 700,000 estimated new HIV infections in children worldwide annually (USPEF, 2017). In 2015, there were roughly 2.1 million new HIV infections, 150,000 of which were among children. Most of these children live in sub-Saharan Africa and were infected via their HIV-positive mothers during pregnancy, childbirth or breastfeeding (AVERT, 2016).
In the absence of prevention of mother-to-child transmission (PMTCT) services, 30 to 40% of pregnant women with HIV will pass the disease to their infants during pregnancy, delivery, or breastfeeding (Colvin et al., 2008; WHO, 2006). Effective interventions of PMTCT can reduce the risk to below 5%, and effective PMTCT programme require women and their infants to receive a cascade of interventions including uptake of antenatal services and HIV testing during pregnancy, use of antiretroviral treatment (ART) by pregnant women living with the virus, safe childbirth practices and appropriate infant feeding, uptake of infant HIV testing and other post-natal healthcare services (WHO/UNICEF, 2007).
In 2011, a Global Plan was launched to reduce the number of new HIV infections via MTCT by 90% by 2015. The World Health Organization (WHO) promotes a comprehensive approach to PMTCT programme which includes: Prevention of new HIV infections among women of childbearing age, preventing unintended pregnancies among women living with HIV, preventing HIV transmission from a woman living with HIV to her baby, providing appropriate treatment, care and support to mothers living with HIV and their children and families (WHO/UNICEF, 2007; WHO/PMTCT, 2016).
According to WHO, Ethiopia is one of the top 10 priority countries accounting for 75% of the global PMTCT service need. It was estimated that the effective scaling up of PMTCT interventions in these countries would prevent over 250,000 new infections annually (WHO/UNICEF, 2007). Despite there has been an increase in the number of health facilities providing prevention of mother-to-child transmission (PMTCT) services in Ethiopia, the proportion of women who receive HIV test during pregnancy as well as HIV-positive pregnant women who receive antiretroviral drugs (ARVs) for PMTCT remains low. This is believed to be due to weak referral linkages, poor male partner involvement, inadequate awareness and low utilization of available PMTCT services, limited use of antenatal and postpartum services, HIV-related stigma and discrimination, the uneven quality of care in antenatal and obstetric settings, insufficient community involvement and low prevalence of institutional delivery (FDRE, 2012; ESPS, 2012; EPHI, 2009).
Ethiopia developed a national guideline on Prevention of Mother-to-Child Transmission (PMTCT) of HIV infection which adopts the PMTCT strategy of WHO/UNICEF/UNAIDS emphasizing primary prevention of HIV infection, prevention of unintended pregnancies among HIV infected women, prevention of HIV transmission from infected women to their infants, and treatment, care and support of HIV infected women, their infants and their families. Most recently, a revised strategy for accelerated implementation of the PMTCT programme was endorsed, with an “opt out” strategy recommended by international PMTCT guidelines. In the ‘opt-out’ strategy, HIV counseling and testing is offered to all women during pregnancy, delivery and postnatally (FDRE, 2012; FHAPCO/MOH, 2007). Despite remarkable achievements on HIV prevention and control, there is a wide concern all over the country and efforts for PMTCT have been lagging behind (FHAPCO, 2010). In response to these challenges and to rapidly expand PMTCT service facilities, the government has developed a rollout plan comprising systematic preparation, planning, capacity building, strengthening logistics and supply, coordination of concurrent activities at national, regional and district levels. On the same line, the five-year strategy for intensifying multi-sectorial response underscores the need for concerted effort to address current gaps in prevention, treatment and care including strengthening PMTCT services (FDRE, 2012).
In Oromia national regional state, alike the national context, PMTCT of HIV/AIDS was one of the crucial foci of the regional health care programs. According to Horo Guduru zone annual report of 2011, PMTCT service was initiated in the zone since 2008. On the other hand, according to the annual performance report of the federal HIV/AIDS prevention and control office (FHAPCO) for 2010, Oromia region got low performance on PMTCT service in the country (EPHI, 2009; FHAPCO, 2010).
PMTCT services are one of the vital areas that need to be ensured for achievement of the sustainable development goals (SDGs) related to health, particularly SDG 3. HIV counseling and testing during pregnancy is the pre-requisite for application of PMTCT interventions. It is the first point of all PMTCT services and crucial for success of subsequent PMTCT programmes.
Prevention of mother to child transmission of HIV/AIDS is one of the national priority programmes of the Federal Ministry of Health (FMOH) and utilization of the service by pregnant women has been of vital health concerns in the country. Despite PMTCT has nationally been regarded as one of the important strategies to prevention of HIV/AIDS, particularly mother-to-child transmission of the infection, there are only few studies showing utilization of PMTCT services in different parts of the country; and utilization status of the service in Horo Guduru Wollega Zone is not yet investigated. Therefore, filling this gap the current study assessed PMTCT service utilization among women having ANC visit in selected public health facilities in the area. The finding provides program planners at various levels with updated information as to implementation of PMTCT programmes. It has particular relevance at local level in providing updated information on PMTCT service utilization of the community and direct future efforts.
Study design, setting and population
Facility-based cross sectional study was conducted from February to March 2016 among mothers attending ANC in selected public health facilities in Horo Guduru Wollega zone which is one of the eighteenth zones in Oromia region, located 314 km west of the capital Addis Ababa. The Zone shares internal borders with West Shewa, East Wollega of Oromia region and West Gojam Zone of Amhara Region. Currently the Zone is divided into nine rural districts and one town administration. The total population of the Zone for the year 2015/2016 was estimated to be about 700,000, and with an estimated 25,486 pregnant women. There is one public hospital, 39 public health centers, and 185 health posts in the zone. Each of ten districts in the zone had one health facility offering various PMTCT services.
Sampling
Sample size was determined using single population proportion formula by considering proportion (p) of PMTCT service utilization Accordingly, the final sample size was calculated to be 398. Among one public hospital and 39 health centers found in the zone, randomly selected four health centers the one hospital purposively included in the study. Accordingly, Fincha health center, Jarte health center, Guduru health center Hareto health center and Shambu District hospital were included in the study. The desired sample size was allocated proportionally based on the estimated average case flow of each health facility, and study participants from each health facility were recruited by using systematic sampling technique.
Data collection and analysis
Data was collected by using a structured interviewer administered questionnaire which was developed after reviewing different literatures. Exit interviews were conducted among mothers attending ANC services. After obtaining informed consent, the interviews were conducted at a private room in all the selected health facilities. Statistical package for social sciences version sixteen (SPSS 16.0) was used for data processing and analysis. Bivariate analysis with crude odds ratio (COR) used to assess variables crudely associated with PMTCT service utilization and select candidate variables for multivariable analysis. Those variables with p-value ≤ 0.25 in the bivariate analysis were considered as candidate for multivariable analysis. Finally, multiple logistic regression analysis providing adjusted odds ratio (AOR) with 95% confidence interval (C.I) was performed to identify factors independently associated with PMTCT service utilization of mothers. In this final model p-value ≤0.05 was used to claim statistical significance.
Socio demographic characteristics
A total of 378 pregnant mothers receiving ANC services participated in the study. Age of the mothers ranged between 20 and 43 years with mean (±SD) of 28.60 (±6.0) years. With regard to residence, 179 (52.6%) of the mothers were from rural and 199 (47.4 %) from urban settings. The largest proportion, 288 (76.2%) of respondents were Oromo in their ethnicity. Regarding ANC visit, 266 (66%) of mothers were having their first ANC visit, while the rest 112 (34%) had had repeated ANC follow-up (Table 1).
Reported knowledge of mothers of PMTCT services
Among the respondents, 320 (84.6%) had ever heard of mother to child transmission (MTCT) of HIV, for whom health workers and social media such as radio and television were the common source of information. Out of those who reported to have the information, 313(82.8%) reported that HIV can be transmitted during pregnancy and 280 (74%) reported that HIV can be transmitted during labour and delivery. On the other hand, 228 (60.3%) of mothers reported that utilization of ANC service is important for PMTCT, and 208 (55%) recognized institutional delivery to be important for PMTCT. The larger proportion (289 (76.5%)) of the mothers reported availability of ARV prophylaxis for HIV positive pregnant mothers to be used for PMTCT while the rest 89 (23.5%) reported as having no information about prophylaxis for positive pregnant mothers (Table 2).
Mothers’ perception towards PMTCT services
Among the respondents, 329 (87%) had favorable attitude towards the PMTCT service provision in terms of client handling by service providers, while about 49 (13%) claimed uncomfortable service provision. The majority [346 (91.5%)] of respondents had favorable attitude on pretest counseling given by service providers, while 43 (11.4%) claims no better counseling given by service providers. On the other hand, 291 (77%) were comfortable with the waiting time in the facilities while the rest 87(23%) were complaining of long waiting time for the services (Table 3). Mothers’ belief on timing appropriate for HIV counseling and testing was assessed. In this regard, 278 (73.5%) believed it is appropriate to get tested any time, and 25 (6.6%) believed on testing during pregnancy (Figure 1).
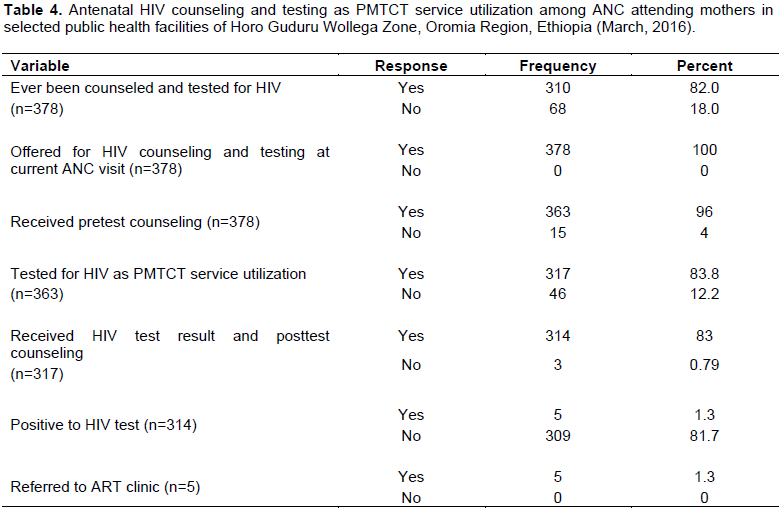
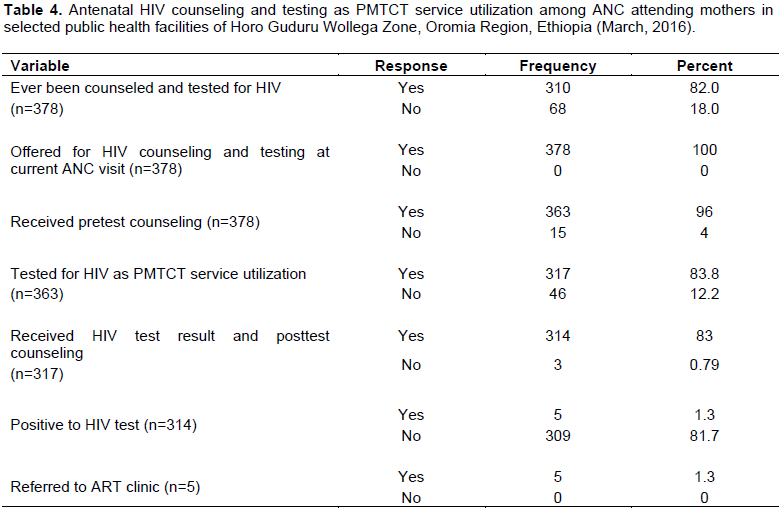
PMTCT service utilization of mothers
All of the study participants, 378 (100%) were offered for HIV counseling and testing at that particular ANC visit. Of these, 363 (96%) clients received pretest counseling, and 317 (83.8%) tested for HIV as PMTCT service utilization; while 61 (16.1%) of the mothers refused pretest counseling and refrained from HIV testing. Among those tested, 314 (83%) received their HIV test results and subsequently received posttest counseling. Out of those who counseled, tested and received their test results, 5 (1.3%) tested positive and were linked to ART clinic (Table 4). When the reason for refraining from HIV counseling and testing is assessed, among the total of 61 ANC clients who refused pretest counseling and refrained from testing, 26 (42.6%) refrained due to fear of stigma and discrimination by the society against potential positive test result, 20 (32.7%) due to their own fear of accepting positive test result, and 15 (24.5%) for being tested in the last three months (Figure 2).

Male partner involvement on utilization of PMTCT services
The majority, 354 (93.7%) of the study participants agreed on importance of discussion with partner about HIV counseling and testing. Nearly three fourth, 277 (73.3%) of mothers reported having less concern and no involvement of their male partners. Among the total of 317 mothers who took antenatal HIV counseling and testing as PMTCT service utilization at the current ANC visit, only 46 (14.5%) took the service together with their male partners (Table 5).
Bivariate analysis
Bivariate analysis was performed to see crude association of each of individual explanatory variables with PMTCT service utilization of the mothers. In the bivariate analysis, age above 35 years, residence, mothers educational status, male partner involvement during antenatal HIV testing, service providers’ perceived handling of clients, partner’s perceived reaction towards mother’s HIV test result had significant association with PMTCT service utilization (with p-value ≤ 0.05). All the variables with p-value ≤ 0.25 in the bivariate analysis were selected for multivariable analysis, while mother’s occupation, current marital status and number of ANC visit had p-values above 0.25 and hence excluded from further processing (Table 6).
Multiple logistic regression analysis
Multiple logistic regression analysis with Backward Logistic Regression (LR) method was performed to identify independent predictors of PMTCT service utilization expressed in terms of utilization of antenatal HIV counseling and testing. All variables which had p-value ≤ 0.25 in the bivariate analysis were entered in to multiple logistic regression model. Accordingly, age category, residence, mother’s educational status, place of delivery for the last child, partners’ occupation, male partner involvement during antenatal HIV testing, service providers’ perceived handling of clients, and partner’s perceived reaction towards mother’s HIV test result were entered in to the model. Among these, age, residence, mother’s educational status, male partner involvement during antenatal HIV testing, and service providers’ perceived handling of clients were significantly associated with PMTCT service utilization of mothers. Women in their advanced age (35-44 years) were about 63% less likely to be tested for HIV for PMTCT as compared to those in their earlier age (25-34 years) (AOR=0.367; C.I=0.139-0.967). Similarly women from rural settings were 43% less likely to be tested for HIV for PMTCT as compared their counterparts from urban settings (AOR= 0.57; C.I=0.063-0.90). It was observed that women with formal education were about 6 times more likely to get tested for HIV for PMTCT service as compared to those who had no formal education (AOR=5.7; C.I=1.13-15.7). Those women who reported to have involvement of their male partners during antenatal HIV counseling and testing were about 4.5 times more likely to get tested for HIV as part of PMTCT service when compared to their counterparts with no partner involvement (AOR=4.49; C.I=2.12-31.2). Mothers’ perception on service providers’ handling of clients was also affecting utilization of the services. In this regard, mothers who perceived that the service providers’ were unfriendly to clients were 76% less likely to get HIV testing for PMTCT service as compared to those who had favorable attitude (AOR=0.24; C.I=0.08-0.72) (Table 7).

PMTCT service utilization
Antenatal HIV counseling and testing is the pre-requisite for application of PMTCT interventions. It is the first point of PMTCT services, and utilization of the service is crucial for success of subsequent PMTCT programmes. In this study, 83.8% of the study participants were tested for HIV on their current ANC visit as part of PMTCT service, and 83% received their test result and subsequently received posttest counseling. This figure was lower when compared with the national recommendation set forth in the national PMTCT guideline, which recommends that every pregnant woman coming ANC visit to health facilities should get HIV counseling and testing (FHAPCO/MOH, 2007). The finding is, however, comparable with that of the study from Western Amhara region in which 94.8% of ANC clients were tested for HIV and received their test result (Worku, 2007). According to another study conducted in Addis Ababa, 92.6% of women attending ANC service were willing to be tested for HIV (Maedot et al., 2007). The figures observed consistently from these reports seems to be effected from the fact that HIV counseling and testing is offered at ANC services for every pregnant mother as an “opt out” strategy and mothers who did not receive their test result could be due to fear of accepting potential positive result and discrimination from family and community. Male partner’s involvement with PMTCT service utilization was poor in this study as only 14.5% of mothers who took antenatal HIV counseling and testing used the service together with their male partner.
Factors associated with PMTCT service utilization
In the current study age, residence, educational status, male partner involvement during antenatal HIV testing, and service providers’ perceived handling of clients were affecting PMTCT service utilization of mothers. It was observed that mothers from rural settings were less likely to utilize PMTCT services as compared to their urban counterparts. This finding is in line with that of the study conducted in Western Amhara region which showed that women who lived in urban settings utilized HIV testing more than those who lived in rural settings (AOR=1.75; CI=1.16-2.64) (Worku, 2007). This could be explained by the fact that women in urban settings have better accesses to ANC/PMTCT services, better education, information and awareness about the services when compared to those in rural settings.
Furthermore, the study indicated that mothers in their late age of pregnancy (34-44 years) were about less likely to utilize PMTCT services as compared to women in their earlier ages. This finding agrees with the study conducted in Jimma zone, southwest Ethiopia, in which pregnant mothers who were in the earlier 15 to 29 years of age utilized PMTCT services more likely than their counterparts in the later age category (Hussein et al., 2011). In contrast, a study conducted in Nekemte town, Ethiopia, indicated that the percentages of willingness to utilize HIV counseling and testing among pregnant mothers increased as age increased (Hasen, 2009). The possible reason for the difference among the findings might be due to differences in the study settings; that is the current study considered ANC clients from both rural and urban settings, whereas mothers participated in the later study of Nekemte town were women only from urban settings.
In the current study maternal education was positively associated with utilization of HIV counseling and testing services. It was observed that mothers who had formal schooling were about 6 times more likely to utilize the service as compared to those who had no formal schooling. This finding is supported by the finding from the study conducted in Kenya, in which women who were more educated were more likely to use VCT services. In line, a study conducted in Uganda indicated that mothers who had educational level beyond seven years of primary school were almost three times more likely to report willingness to be tested when compared to those who did not complete primary school or had not been educated at all (Bajunirwe and Muzoora, 2005). The link with educational status could be directly explained that those educated have better knowledge of MTCT HIV/AIDS and better understanding of benefits of PMTCT service utilization and could be more likely to respond to health promotion messages (Namazzi, 2010). For instance, a study conducted on acceptability of HIV counseling and testing services at Dilchora Hospital, Dire Dawa, Ethiopia, revealed that knowledge on MTCT was significantly determining acceptance of the service among ANC clients (Maedot et al., 2007).
It was observed from the current study that 16.1% of the study participants refused pretest counseling and refrained from HIV testing, of which 76.5% due to fear of stigma and discrimination following potential HIV positive test result. This is in congruent with similar studies from Addis Ababa, Ethiopia, in which women’s perceived ability to cope with positive result and perceived negative community response determined voluntary counseling and testing (VCT) acceptance of the study participants (Abebaw et al., 2009). According to a study conducted in Ghana, stigmatization and discrimination constitutes a big challenge that 73.9% of women who had not been tested for HIV were willing to do it only if anonymity is strictly ensured. The study magnifies stigma, fear of potential positive test result, and issue of confidentiality to be among important factors affecting utilization of the services (Addo, 2005). It has been estimated that over 50% of vertical HIV transmissions from mother-to-child globally can be attributed to the cumulative effect of HIV stigma and discrimination when accessing PMTCT services, and HIV-related stigma and discrimination affect a pregnant woman's decision to enroll in PMTCT programmes (WHO/PMTCT, 2016). The important point to be noted from these findings is that HIV stigma and discrimination in the community continues to be a big challenge to the implementation of PMTCT programs and utilization of the services.
Male partner involvement during antenatal HIV counseling and testing was determining PMTCT service utilization of mothers. A study conducted in South Africa revealed that increased male participation, enhanced communication, HIV counseling and testing, adherence, sero status disclosure increase couples’ communication and encourage adherence to PMTCT services (Peltzer et al., 2011). Similarly, a study conducted in Cameroon also pointed out that male involvement is necessary for improving women’s utilization of PMTCT services. It has been linked to greater uptake of testing, greater uptake of anti-retroviral drugs, increased condom use, increased communication and support for infant feeding choices (Bissek et al., 2011). According to another study, among the strongest predictors of women’s’ willingness to accept HIV test was the woman's perception that her husband would approve her test result; women who thought their husbands would approve their test result were almost six times more likely to report willingness to be tested as compared to those who thought their husbands would not approve it (OR=5.6; CI=2.8-11.2) (Bajunirwe and Muzoora, 2005). Similarly, different studies from Addis Ababa, Ethiopia, indicated that involvement of male partner has significant association with women’s acceptance of voluntary HIV counseling and testing (Jebessa and Teka, 2005; Abenet, 2007). As revealed from a study conducted in West Amhara region, Ethiopia, partner participation in VCT and couple counseling is found to increase success of PMTCT programs (Worku, 2007). Men’s participation in ANC/ PMTCT is usually affected by socio cultural barriers centered to cultural beliefs and traditional gender roles (Nkuoh et al., 2010).
It was observed that service providers’ perceived handling of clients affecting PMTCT service utilization of mothers as those mothers who perceived unfriendly handling by service providers were less likely to utilize the service. This finding is in agreement with that of the study conducted in Addis Ababa, Ethiopia, in which 76.8% of women who have positive attitude towards testing process at facilities determine VCT utilization for PMTCT (Abenet, 2007); and also supported by another study from Arba Minch, Southern Ethiopia (Sanou et al., 2016). This implies that the service providers’ handling of clients has great contribution to utilization of the services, and clients’ perception and attitude towards service providers or the service provision has great impact to acceptance of the services.
This study has tried to assess the level of utilization of PMTCT services and tried to investigate some factors affecting it. We believe that using the same sex (female nurses) who were not working in the health facilities where the study is based for data collection could have assured friendly communication in providing unbiased data for the study. The cross sectional nature of the study in ascertaining cause effect relationship between PMTCT service utilization and the explanatory variables under consideration we declare as limitation of the study.
The utilization of antenatal HIV testing as PMTCT service utilization was lower when compared with the national recommendation. This gap provides program planners, local health offices with important information regarding PMTCT service utilization of the community, and would serve as important evidence to direct effective future efforts. Age, residence, educational status, male partner involvement during antenatal HIV testing, and service providers’ perceived handling of clients were affecting PMTCT service utilization of mothers.
The authors have not declared any conflict of interests.
REFERENCES
|
Abebaw D, Demrow A, Abera M (2009). Determinants of acceptance of voluntary HIV testing among antenatal clinic attendees at Dilchora Hospital, Dire Dawa, Ethiopia. Ethiop. J. Health Dev. 23(2):141-147.
|
|
|
|
Abenet TK (2007). Assessment of male partners influence on pregnant women towards voluntary HIV testing and support on PMTCT in hospitals of Addis Ababa.
|
|
|
|
Addo VN (2005). Pregnant women's knowledge of and attitudes to HIV testing at Komfo Anokye Teaching Hospital, Kumasi. Ghana Med. J. 39(2):50-54.
|
|
|
|
Bajunirwe F, Muzoora M (2005). Barriers to the implementation of programs for the prevention of mother-to-child transmission of HIV: A cross-sectional survey in rural and urban Uganda. AIDS Res. Ther. 2(1):10.
Crossref
|
|
|
|
Bissek ACZK, Yakana IE, Monebenimp F, Chaby G, Akondeng L, Angwafor SA, Lok C, Njamnshi AK, Muna WF (2011). Knowledge of pregnant women on mother-to-child transmission of HIV in Yaoundé. Open AIDS J. 5:25-28.
Crossref
|
|
|
|
Colvin M, Gorgens A, Kasedde M (2008). Analysis of HIV prevention response and modes of HIV transmission: UNAIDS Regional Support Team for Eastern and Southern Africa, 2009.
|
|
|
|
Ethiopia Federal HIV/AIDS Prevention and Control Office (FHAPCO) Ministry of Health (MOH) (2007). Guidelines on Prevention of Mother-to-Child Transmission of HIV.
|
|
|
|
Ethiopia Federal HIV/AIDS Prevention and Control Office (FHAPCO) (2010). Annual Performance Report of Multispectral HIV/AIDS Response.
|
|
|
|
Ethiopia Public Health Institute (EPHI) (2009). Report on the Round Antenatal Care Sentinel HIV Surveillance in Ethiopia.
|
|
|
|
Ethiopian Society of Population Studies (2012). Maternal Health Care Seeking Behaviour in Ethiopia: Findings from EDHS 2005: Ethiopian Society of Population Studies: In-depth Analysis of the Ethiopian Demographic and Health Survey 2005.
View
|
|
|
|
Federal Democratic Republic of Ethiopia (2012). Country Progress Report on HIV/AIDS Response.
|
|
|
|
Federal Democratic Republic of Ethiopia HIV/AIDS Prevention and Control Office (2014). Country progress report on the HIV Response, 2014.
|
|
|
|
Federal HIV/AIDS Prevention and Control Office (FHAPCO). Ministry of Health Ethiopia (2015). HIV Epidemic Estimates, global, 2015.
View
|
|
|
|
Hasen T (2012). Acceptability of provider initiated HIV counseling and testing in pregnant mothers attending ANC at Nekemte town government health facilities. Sci. Technol. Arts Res. J. 1(3):24-30.
Crossref
|
|
|
|
Hussein M, Jira C, Girma B (2011). Assessment of effective coverage of HIV prevention of pregnant mother to child transimission services in Jimma Zone, South West Ethiopia. Ethiop. J. Health Sci. 21(Suppl 1):1-7.
|
|
|
|
Jebessa S, Teka T (2005). Knowledge and attitude towards mother to child transmission of HIV and it's prevention among post natal mothers in Tikur Anbessa and Zewditu Memorial Hospitals, Addis Ababa. Ethiop. J. Health Dev. 19(3):211-218.
|
|
|
|
Maedot P, Haile A, Lulseged S, Belachew A (2007). Determinants of vct uptake among pregnant women attending two ANC clinics in Addis Ababa City: unmatched case control study. Ethiop. Med. J. 45(4):335-342.
|
|
|
|
Namazzi JA (2010). Determinants of using voluntary counseling and testing for HIV/AIDS in Kenya. J. Manage. Policy Pract. 11(5):89-96.
|
|
|
|
Nigatu T, Woldegebriel Y (2011). Analysis of the prevention of mother-to-child transmission (PMTCT) service utilization in Ethiopia: 2006-2010. Reprod. Health 8(1):6.
Crossref
|
|
|
|
Nkuoh GN, Meyer DJ, Tih PM, Nkfusai J (2010). Barriers to Men's Participation in Antenatal and Prevention of Motherâ€toâ€Child HIV Transmission Care in Cameroon, Africa. J. Midwifery Women's Health 55(4):363-369.
Crossref
|
|
|
|
Peltzer K, Jones D, Weiss SM, Shikwane E (2011). Promoting male involvement to improve PMTCT uptake and reduce antenatal HIV infection: a cluster randomized controlled trial protocol. BMC Public Health 11(1):778.
Crossref
|
|
|
|
Sarker M, Sanou A, Snow R, Ganame J, Gondos A (2007). Determinants of HIV counselling and testing participation in a prevention of motherâ€toâ€child transmission programme in rural Burkina Faso. Trop. Med. Int. Health 12(12):1475-1483.
Crossref
|
|
|
|
United States President's Emergency Plan for AIDS Relief. Prevention of Mother-to-Child Transmission.
View
|
|
|
|
Worku T (2007). Utilization of PMTCT services among pregnant woman in western Amhara region Ethiopia. MPH thesis.
|
|
|
|
World Health Organization (WHO) (2006). Definitions of HIV for Surveillance and Revised Clinical Staging and Immunological Classification of HIV-Related Disease in Adults and Children; WHO, Geneva, Switzerland.
|
|
|
|
World Health Organization (WHO) (2010). PMTCT Strategic Vision 2010–2015: Preventing mother-to-child transmission of HIV to reach the UNGASS and MDGs.
View
|
|
|
|
World Health Organization (WHO) (2016). HIV/AIDS: Data and statistics.
View
|
|
|
|
World Health Organization (WHO) (2017). Global Health Observatory (GHO) Data HIV/AIDS Reports.
View
|
|
|
|
World Health Organization (WHO) PMTCT Guidelines (2016). Prevention of Mother-To-Child Transmission (PMTCT) of HIV.
View
|