Full Length Research Paper
ABSTRACT
INTRODUCTION
Globally, before 1990, 1600 women were estimated to die each day as a result of complications during pregnancy or childbirth. However, a large proportion of these deaths are preventable (Jowett 2000). In 2015, about 99% of maternal deaths resulting from pregnancy related complications occurred in low and middle income countries where there is a prevalence of high fertility rates, a low skilled birth attendants, and weak health systems (UNICEF, 2009). From this percentage, sub-Saharan Africa covers makes up 66% (WHO, UNICEF,UNFPA, 2015). These maternal deaths result from direct complications during delivery such as hemorrhage, sepsis, obstructed labour, hypertensive disorders of pregnancy and septic abortion (Austin et al., 2014; Biswas et al., 2016; WHO, UNICEF, UNFPA, 2015; World-Health-Organisation n.d.; Valentino and Kenya, 2009; UNICEF, 2009; Thaddeus and Maine, 1994; Singh et al., 2016; Odusola, 2013). The reduction of maternal mortality from obstetric complications cannot be possible unless women exposed to such complications receive timely and adequate obstetric care (Saaka et al., 2017; Ganle, 2016; Broughton et al., 2016; Engmann et al., 2016). Maternal mortality majorly occur due to distance and consequent delay in treatment during childbirth (Irene Figa, 2000). Also, according to 2013 World Health Statistics, showed that there are gaps in maternal mortality between the poor and rich regions. A high number of maternal and newborn deaths in some areas of the world occurs as a result of inequalities to access health services; this indicates the discrepancy between rich and poor(7,8). As a result, an average maternal mortality in countries with low income, lower middle income, upper middle income and high income groups were 410, 260, 53, and 14/100,000 live births, respectively (WHO, UNICEF, UNFPA 2015).
Similarly, the proportion of mothers that do not survive childbirth compared to those that survive in low and middle income regions is still 14 times higher than that of the developed regions (Action, 2015). From this finding, Sustainable Development Goal (SDG) is working to reduce the global maternal mortality ratio to less than 70 per 100,000 live births and to end preventable deaths of newborns as much as possible to 12 per 1000 live birth in each country until 2030 (Derek et al., 2015). Before 1990 in this country, the maternal mortality was high due to problems emanated from both supply and demand. For supply, lack of qualified health professionals, inaccessibility of health facilities, unavailability of medical supplies, and drugs for those who are in need and hard to reach areas were issues that weaken the health system until the country introduced a 20-year health sector development program in 1977, which is being implemented (Banteyerga, 2011). As regards demand, lack of awareness, negative attitude and poor and harmful traditional practices were prior causes for maternal mortality back in the 1990s (WHO, 2016; WHO, UNICEF, UNFPA, 2015; World-Health-Organisation n.d.). In 1990, it was 1250 per 100,000 live births (WHO, 2016); but currently it has reduced to one third, from 1250 to 412 per 100,000 live births. This puts Ethiopia 31st in the world with average MMR of 412 (273-551) per 100, 000 live births in 2016 (WHO, 2016; FDRE MOH, 2016). In poor and marginalized areas, cost, distance, and the time needed to access care are major barriers for effective utilization of maternal and child healthcare services (IN HEALTH, 2015).
A number of innovative strategies to overcome cost, distance, and time barriers to access care were identified and evaluated; they include, community financial incentives, loan/ insurance schemes, and maternity waiting homes. In these areas or regions where maternal and neonatal mortality is high due to inaccessibility of facilities, the strategy to reduce such issue is very vital (World-Health-Organisation n.d.). A maternity waiting home was launched in 1950s and resulted in visible effect to reduce maternal and newborn mortality (WHO, 1996). In Canada, Nicaragua, Guatemala, Timor-Leste Finland carried out major efforts to reduce maternal and neonatal mortality (Cortez, 2012; Ruiz et al., 2013; Singh et al., 2017; WHO, 1996). The alleviation of maternal mortality catastrophe, so named Maternity Waiting Homes (MWHs) or Maternity Waiting Areas (MWAs), has various names at different settings with similar objective. Although there were plenty of challenges from supply and demand, its utilization had positive impacts in the improvement of maternal and child health in countries launched earlier and later. MWH is defined as a residence near a health facility with emergency obstetric care (EmOC) for mothers who are far from facilities to reside there until delivery and a part of postpartum period. In Africa, most western and eastern African countries were started to use MWHs and studies were conducted to assess the gaps, effectiveness and related topics. For instance Ghana in west Africa, Liberia in east Africa Ethiopia, Eritrea, Zambia, Zimbabwe, Kenya, Malawi were MHWs were launched and various studies were conducted to assess the gaps from different perspectives.
MATERNITY WAITING HOMES IN ETHIOPIA
MATERIALS AND METHODS
RESULTS
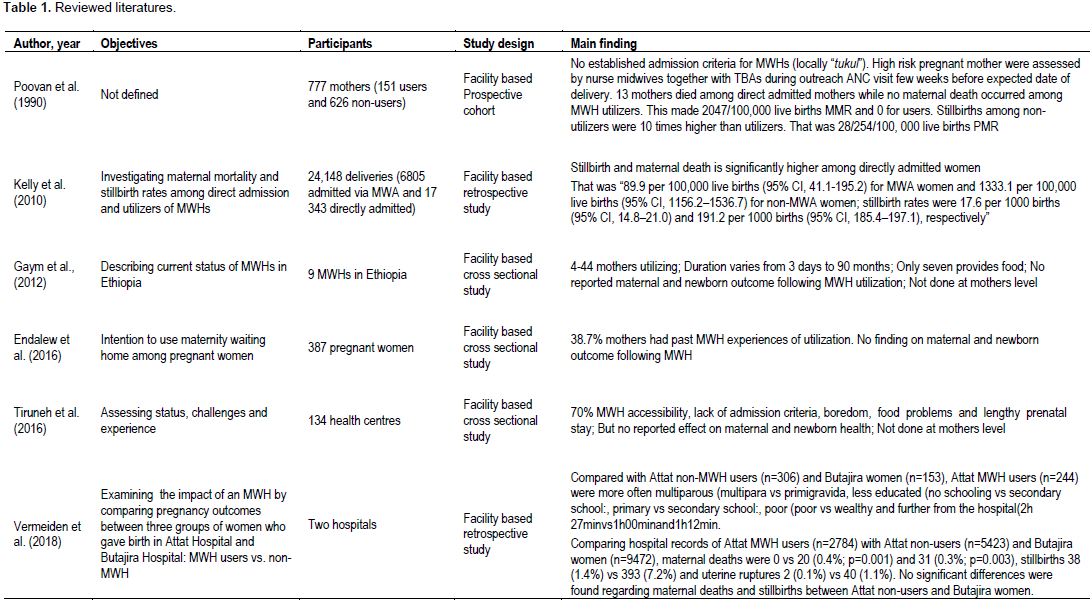
After establishing inclusion and exclusion criteria, six papers met the inclusion and exclusion criteria from all the above databases for further review in the study. All were facility based studies conducted in Ethiopia from 1990s and late 2000s (Endalew et al., 2016; (Gaym et al., 2012; Kelly et al., 2010; Poovan et al., 1990; Tiruneh et al., 2016). Three assessed the outcome and three were focused on the experience, coverage, predictors and contexts of MWHs in Ethiopia. In 1990, a hospital based prospective cohort with objective of MWHs effects on perinatal and maternal outcome was done (Poovan et al., 1990). Here, 151 mothers used and 635 mothers did not utilize the MWHs, from 1987 to 1990. This study showed that the perinatal mortality among non-utilizers mothers were ten times more than non-utilizers; about 28 and 254 perinatal death per 100,000 live births with RR =0.46 95% CI (0.33-0.66). Also, there is a visible difference in maternal mortality among users and nonusers of MWHs. No mother died among the users and there was 2047 MMR per 100,000 live births. This claimed that there is likely less risk of maternal and perinatal mortality among users than nonusers of MWHs. Another 22 years retrospective hospital based study conducted in Atat hospital was done in 2010. This showed that there is significant association between maternal and perinatal birth with MWHs utilization(Kelly et al. 2010). In this study, in a total of 24,148 deliveries, 6805 mothers attended MWHs and 17343 mothers did not utilize MWHs.
Maternal mortality was 89.9 per 100 000 live births (95% CI, 41.1–195.2) for women who utilized MWHs and 1333.1 per 100 000 live births (95% CI, 1156.2–1536.7) for non-utilizers; stillbirth rates were 17.6 per 1000 births (95% CI, 14.8–21.0) and 191.2 per 1000 births (95% CI, 185.4–197.1). Consequently, there is a significant difference and advantage in decreasing maternal and perinatal mortality among utilizers than non-utilizers. The third study which was still facility based was done recently in 2012 with objective of describing the existing situations of MWHs in Ethiopia (Gaym et al., 2012). The overviews of the last thirty years history of MWHs were described. They only got information from the Federal Ministry of Health about the existing MWHs in five regions of the country. Based on this information, they assessed only nine facilities (eight hospital and one health center) with MWHs. This study tried to assess the admission criteria, challenges, numbers of utilizers per each MWHs and duration of the stays. In addition cesarean section rate was higher among utilizers than non-utilizers. The strengths revealed the introduction period of MWHs in Ethiopia as it was started in 1985. The weaknesses in this study and the described issues are not representatives of the country’s status of MWHs phenomena in the last thirty years. This is because they used data from FMoH, which include only five regions, nine MWHs, and have not assessed the maternal and perianal mortality rate mentioned and studied on MWHs.
Very recently, facility based cross sectional study in 2016 assessed the status quo of MWHs and the experiences and challenges of mothers using waiting homes. It included 134 health centers from four broad regions of the country. More so, it focus mainly on coverage, admission criteria, predictors or challenges as well as prevalence rate of utilization of MWHs among existing and functional MWHs (Tiruneh et al., 2016). However, the study never identified the impact and outcome of MWHs on maternal and perinatal mortality in detail. The last study was cross sectional facility based, aimed with assessing intention to use maternity waiting home among pregnant women in southwest Ethiopia. This showed that 38.7% of mothers had past history of MWHs utilization. About 48% women reported MWHs are very important to get better pregnancy outcome(Endalew et al., 2016). However, only one study revealed different predictors of maternity waiting homes utilization. They were schematized as finance, lack of knowledge, privacy, social support, custom and cultural influences and lack of social support. About 50% of MWHs share the sleeping room and only 6% of MWH have curtains for their privacy. After admission to the MWHs, health care workers, especially midwives, performed an initial evaluation of pregnant women. About 87% MWHs reported that a midwife/nurse made round to mothers primarily to follow-up the current pregnancy (Gaym et al., 2012).
DISCUSSION
LIMITATIONS OF THE REVIEW
CONCLUSION
REFERENCES
|
Abdulkadir RW (2015). Knowledge, attitude and practice of mothers towards skilled delivery services in a maternity waiting home in Merti District, Isiolo County. Prime J. Soc. Sci. 4(8):1140-1154. |
|
|
Time for Global Action (2015). Sustainable Development Goals Fact Sheet, Available at: View. |
|
|
Andemichael G, Haile B, Kosia A, Mufunda J (2010). Maternity waiting homes: A panacea for maternal/neonatal conundrums in Eritrea. J. Eritrean Med. Assoc. 4(1):18-21. |
|
|
Austin A, Ana L, Rehana AS, Zohra SL, Jai KD, Zulfiqar AB (2014). Approaches to improve the quality of maternal and newborn health care: An overview of the evidence. Reproductive Health 11(Suppl 2):1-9. |
|
|
Banteyerga H (2011). Ethiopia ' s Health Extension Program : Improving Health through Community Involvement, Addis Ababa Ethiopia, 13(3): 46-49. |
|
|
Biswas A, Koustuv D, Abu Sayeed MA, Mervyn G, Halim MA (2016). Maternal complications in a geographically challenging and hard to reach district of Bangladesh: a qualitative study. F1000Research, 5(2417):1-9. |
|
|
Broughton E, Hermida J, Hill K, Nancy S, Mario C, Daniel G, Juana MF, Ximena G (2016). Evaluation of an Intervention to Improve |
|
|
Chandramohan D (1995). The Effect of Stay in a Maternity Waiting Home on Perinatal Mortality in Rural Zimbabwe. J. Trop. Med. Hyg. 98:2061-267. |
|
|
Cortez R (2012). Maternity waiting homes and institutional birth in Nicaragua : policy options and strategic implications. Int. J. Health Plann. Manage. pp. 150-166. |
|
|
Derek O, Amy C, Farooq U (2015). Universal Sustainable Development Goals Understanding the Transformational Challenge for Developed Countries. Report of Study by Stakeholder Forum. |
|
|
Drewniak N, Zeitlin J (2014). Where does distance matter ? Distance to the closest maternity unit and risk of foetal and neonatal mortality in France. Eur. J. Public Health 24(6):904-909. |
|
|
Eckermann E, Deodato G (2008). Maternity waiting homes in Southern Lao PDR: The unique "silk home" Introduction: the Problem. J. Obstet. Gynaecol. Res. 34(5):767-775. |
|
|
ELS (nd). Planning a Critical Review, Edinburgh, United Kingdom. Available at: www.qmu.ac.uk/ELS. |
|
|
Endalew GB, Gebretsadik LA, Gizaw AT (2016). Intention to use Maternity Waiting Home among Pregnant Women in Jimma District, Southwest Ethiopia. Glob. J. Med. Res. 16(6):1-9. |
|
|
Engmann CM, Abraham H, Raymond A, Philip LA, Cheryl AM (2016). Addressing the continuum of maternal and newborn care in Ghana : implications for policy and practice. Health Policy and Planning 31:1355-1363. |
|
|
Ethiopian FMOH (2005). MWA Policy Document: National requirements of MWA to standardize services at the PHCUs., pp.1-4. |
|
|
FDRE MOH (2016). Ethiopia Demographic and Health Survey, Addis Ababa. Available at: View. |
|
|
Ganle JK (2016). Why Muslim women in Northern Ghana do not use skilled maternal healthcare services at health facilities : a qualitative study. BMC Int. Health Human Rights 15:10. |
|
|
Gaym A, Pearson L, Soe KW (2012). Maternity Waiting Homes In Ethiopia – Three Decades Experience. Ethiop Med. J. 50(3):209-219. |
|
|
IN HEALTH (2015). From MDGs to SDGs: General Introduction. Available at: View. |
|
|
Irene Figa T (2000). Maternal Mortality and the problem of Accessibility to Obstetric Care; The Strategy of Maternity Waiting Homes. Soc. Sci. Med. 42(10):1381-1390. |
|
|
Jody R, Lori E (2014). Promoting Access: The use of maternity waiting homes to achieve safe motherhood. Midwifery 29(10):1095-1102. |
|
|
Jowett M (2000). Safe motherhood interventions in low-income countries : an economic justification and evidence of cost effectiveness. Health Policy 53:201-228. |
|
|
Kelly J, Kohls E, Poovan P, Schiffer R, Redito A, Winter H, MacArthur C (2010). The role of a maternity waiting area (MWA) in reducing maternal mortality and stillbirths in high-risk women in rural Ethiopia. BJOG: An Inter. J. Obstet. Gynaecol. 117(11):1377-1383. |
|
|
Lonkhuijzen L, Margreet S, Rebecca N, Roosmalen J (2003). Use of maternity waiting home in rural Zambia. Afr. J. Reprod. Health 7(1):32-36. |
|
|
Lonkhuijzen L, Stekelenburg J, Roosmalen J (2012). Maternity waiting facilities for improving maternal and neonatal outcome in low-resource countries. Cochrane Database Syst. Rev. 8(3):CD006759. |
|
|
Lori JR, Munro-Kramer ML, Mdluli EA, Musonda GK, Boyd CJ (2016). Developing a community driven sustainable model of maternity waiting homes for rural Zambia. Midwifery 41:89-95. |
|
|
Lori JR, Garfee W, Michelle LM, Nene D, Carol JB (2014). It takes a village : a comparative study of maternity waiting homes in rural |
|
|
Liberia. The Lancet Global Health 2:11. |
|
|
Lori JR, Michelle LM, Sarah R, Garfee W, Bernice TD, Carol JB, Jennifer EM, Walter G (2013). Maternity waiting homes and traditional midwives in rural Liberia. Inter. J. Gynecol. Obstet. 123(2):114-118. |
|
|
Lori JR, Wadsworth AC, Munro ML, Rominski S (2013). Promoting access: The use of maternity waiting homes to achieve safe motherhood. Midwifery 29(10):1095-1102. |
|
|
Margaret EK, Sabrina H, Elysia L, Daniel V, Qixuan C, Festo M, Beatrice B, Godfrey M (2016). Who is left behind on the road to universal facility delivery? A cross-sectional multilevel analysis in rural Tanzania. Trop. Med. Int. Health 20(8):1057-1066. |
|
|
Mramba L, Faiza AN, Charles O, Davies K (2010). Reasons for low utilization of a maternity waiting home in rural Kenya. Inter. J. Gynecol. Obstetr. 108(2):152-153. |
|
|
Odusola A (2013). Accelerating progress on maternal health in Africa: lessons from emerging policy and institutional innovations. Working Paper No, New York: UNDP. |
|
|
Poovan P, Kifle F, Kwast BE (1990). A maternity waiting home reduces obstetric catastrophes. World Health Forum 11:440-445. |
|
|
Ruiz MJ, van Dijk MG, Berdichevsky K, Munguía A, Burks C, García SG (2013). Barriers to the use of maternity waiting homes in indigenous regions of Guatemala: a study of users' and community members' perceptions. Culture, Health Sexuality 15(2):205-218. |
|
|
Saaka M, Paul A, Robert k, Mohammed A, Abdul RM (2017). The effect of social behavior change communication package on maternal knowledge in obstetric danger signs among mothers in East Mamprusi District of Ghana. Globalization Health 13(19):1-12. |
|
|
Sialubanje C, Karlijn M, Elisa MK, Marit SGP, Davidson HH, Robert ACR (2015a). Husbands' experiences and perceptions regarding the use of maternity waiting homes in rural Zambia. Int. J. Gynaecol. Obstet. 133:108-111. |
|
|
Sialubanje C, Karlijn M, Elisa MK, Marit SGP, Davidson HH, Robert ACR (2015b). Improving access to skilled facility-based delivery services : Women's beliefs on facilitators and barriers to the utilisation of maternity waiting homes in rural Zambia. Reproductive Health 12(61):1-13. |
|
|
Sialubanje C, Karlijn M, Davidson HH, Robert ACR (2017). Personal and environmental factors associated with the utilisation of maternity waiting homes in rural Zambia. BMC Pregnancy and Childbirth, 17(136):1-14. |
|
|
Singh K, Ilene S, Eunsoo TK Clara L, Ann P (2017). Reaching vulnerable women through maternity waiting homes in Malawi. Int. J. Gynecol. Obstet. 136:91-97. |
|
|
Singh K, Story WT, Moran AC (2016). Assessing the Continuum of Care Pathway for Maternal Health in South Asia and Sub-Saharan Africa. Mat. and Child Health J. 20(2):281-289. |
|
|
Sundu S, Mwale OG, Chirwa E (2017). Antenatal Mothers' Experience of Staying in a Maternity Waiting Home at Malamulo Mission Hospital in Thyolo District Malawi : A Qualitative, Exploratory Study. Women's Health Gynecol. 3(1):1-10. |
|
|
Thaddeus S, Maine D (1994). Too far to walk: maternal mortality in context. Soc. Sci. Med. 38(8):1091-1110. |
|
|
Tiruneh GT, Belaynew WT, Ali MK, Wuleta AB, Nebreed FZ, Tewabech GW, Ephrem TL (2016). Maternity waiting homes in Rural Health Centers of Ethiop: The situation, women's experiences and challenges. Ethiop. J. Health Dev. 30(1):19-28. |
|
|
United Nations Children's Fund (UNICEF) (2009). The state of the world's children: Maternal and newborn health. 2009, Geneva. |
|
|
Valentino LM, Kenya N (2009). Maternal and newborn health and emergency transport in sub-Saharan Africa. InInternational Forum for Rural Transport Development (IFRTD).(Unpublished Report) 2009. Available at: View. |
|
|
Vermeiden T, Floris B, Girmay M, Asheber G, Thomas A, Jelle S (2018). Factors associated with intended use of a maternity waiting home in Southern Ethiopia : a community-based cross- sectional study. BMC Pregnancy and Childbirth 18:1-9. |
|
|
World Health Organization (WHO) (1996). Maternity Waiting Homes: A review of experiences, Available at: View. |
|
|
World Health Organization (WHO) (2016). WHO Maternal Mortality Factsheet. WHO, pp. 1-4. Available at: View. |
|
|
WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division (2015). Trends in Maternal Mortality : 1990 to 2015, Geneva, Switzerland. Available at: View. |
|
|
Wild K, Kelly P, Barclay L, Martins N (2015). Agenda setting and evidence in maternal health: connecting research and policy in Timor-Leste. Front. Public Health 3(212):1-9. |
|
|
Wilson JB, Collison AHK, Richardson D, Kwofie G, Senah KA, Tinkorang EK (1997). The maternity waiting home concept: the Nsawam, Ghana experience. Int. J. Gynecol. Obstet. 59(2):165-172. |
|
Copyright © 2024 Author(s) retain the copyright of this article.
This article is published under the terms of the Creative Commons Attribution License 4.0