ABSTRACT
The study assessed the emotional reactions and perceptions of stigmatization among family caregivers of Lassa fever patients. Six focus group discussions were held among 48 purposively selected and consenting family caregivers in a Lassa fever treatment facility in South-South Nigeria during an outbreak. An interview guide structured to elicit views and perceptions on Lassa fever, reactions to the news of a positive result stigma, sources of emotional and social support was used for data collection. Data were transcribed, coded, and analyzed along thematic areas. Awareness of Lassa fever was high among the participants. Reactions to a positive test result included emotions of panic, denial, anxiety, and fear. Some respondents expressed their unwillingness to disclose a positive test result; some felt Lassa fever was stigmatized in the community and by healthcare workers. Majority turned to religion as a source of emotional support. Family caregivers of Lassa fever patients experienced varied emotional reactions upon receipt of the news of a positive test result. Some caregivers had been stigmatized by health workers or feared stigmatization at community level. Psychosocial support was obtained from religion and emotional support from survivors and isolation ward healthcare workers. Community health education should be sustained to avoid stigmatization of victims. Pre- and post-test counselling, access to relevant information and psychosocial support should be made available family care givers.
Key words: Fear, Lassa fever, stigma.
Outbreaks of highly infectious diseases create a public health crisis as they increase morbidity and mortality, disrupt routine preventive and curative health services, and overstretch medical infrastructure. Under certain circumstances such as rising mortality from the disease, poor public understanding of transmission and perceived severity of the disease, infectious disease outbreaks generate a social response by the public that can potentially disrupt the social milieu and cohesion of communities. A social response in this context means the behavioural or emotional display of concern shown by the public in response to an outbreak (Fast et al., 2015). Such responses include panic, frustration and fear, and in extreme cases, stigmatization and violence against persons believed to have the disease (Fast et al., 2015). Public health precautionary measures that include exclusionary practices to the affected can further exacerbate this social response with the introduction of stigmatization and discrimination against persons perceived to be responsible for the outbreak. Such reactions have been reported during Severe Acute Respiratory Syndrome (SARS) outbreak in Hong Kong (Cheng, 2004)and Ebola outbreak in Uganda (Kinsman, 2012). Outbreak response strategies then will include both an epidemiological and a social process. The epidemiological process is required to identify appropriate containment measures and culminates in the initiation or scale up of public health actions that eventually control the outbreak (Kinsman, 2012). The social response addresses the public’s reaction to the disease.
Stigmatization is the process of negative discrimination against people with certain physical, behavioural, or social attributes (Barrett and Brown, 2008; Perry and Donini-Lenhoff, 2010; Fischer et al., 2019). Applied to infectious disease outbreaks, social stigmatization results from a perceived link between a person or persons known or perceived to have the disease, be a carrier or a contact to an infected person (UNICEF, 2020). Such negative perceptions and treatment can impact negatively on those with the disease, extending to their family caregivers and communities (United Nations Childrens' Fund [UNICEF], 2020). Social stigma represents an obstacle to infectious disease outbreak control. Fear of stigmatization can lead to concealment of and denial of Lassa fever symptoms. Delay in seeking medical attention leads to late detection, delayed onset of treatment and community spread of the disease (Barrett and Brown, 2008). Indirect effects of discrimination and social marginalization of infected person or their families are neglect and poverty, further increasing their susceptibility to Lassa fever. Stigmatized populations may display distrust towards public health authorities and resist government assistance even at the expense of their health and wellbeing (Barrett and Brown, 2008). Violence against a stigmatized group has been known to occur (Perry and Donini-Lenhoff, 2010). Social stigmatization may be extended to family caregivers, who are vital to provide financial, emotional and physical care and support to the sick (Oyebode, 2003). Family caregivers accompany patients to the health facility and may assist with admission formalities. In situations where health workers are in short supply and overstretched, family caregivers to patients in general wards may be called upon to assist with a variety of bedside activities such as bathing, dressing and feeding (Islam et al., 2014).
Lassa fever is a highly infectious haemorrhagic illness caused by a virus belonging to the family Arenaviridae. It is spread from the Mastomys natalensis rodent reservoir to man through contact with rodent excreta or urine in food or during hunting and processing of rats for consumption. Human to human spread occurs within households during care for sick relatives or in health care settings (Bonwitt et al., 2017). Lassa fever seasonal outbreaks occur annually in Sierra Leone, Guinea and Nigeria. Sporadic outbreaks have been reported in Ghana, and Ivory Coast, Senegal and Mali (Ogbua et al., 2007). In Nigeria, the number of states reporting Lassa fever has increased from 19 in 2017 to 27 in 2020 (Nigeria Centre for Disease Control [NCDC], 2017). Edo state records the highest number of cases annually.
While 80% of infections are subclinical, 15 to 20% of infected persons develop clinical illness that requires hospitalization in designated treatment facilities where isolation precautions and restricted access regulations prevent nosocomial transmissions.
Reports of patients and their family caregivers alienated by health care workers and the community have followed a laboratory confirmation of Lassa fever or other viral haemorrhagic fevers (Kuriansky and Toriello, 2016; Mmadu-Okoli, 2019; Richmond and Baglole, 2003). Aside from this, Lassa fever patients and their caregivers are often left in the dark as to the nature of treatment, isolation and the need for it, and how to protect themselves during hospital stay with their sick patients.
No study has been conducted to assess stigmatization or discrimination among family caregivers of Lassa fever patients in Nigeria. A study of psychosocial state and perceived stigma among family caregivers is pertinent to inform the design of interventions to provide psychosocial support to caregivers.
Study area
The study was conducted at Irrua Specialist Teaching Hospital (ISTH) in Edo State, Nigeria. The tertiary facility is located in Irrua, the headquarters of Esan Central Local Government Area. Commissioned on 21st of November 1991, the institution provides comprehensive preventive, promotive, curative, and rehabilitative health services to the people of Edo and neighbouring states. It is a centre of training for medical professionals and nurses, and home to the Institute of Lassa Fever Research and Control (ILFRC), the designated national centre for the management of Lassa fever. The hospital has several out-stations from where outreach services are provided to surrounding communities.
Study population
Purposive sampling technique was used for participant recruitment.
Purposive sampling involves identifying and interviewing persons whose contributions would be most informative in addressing the research questions and unravelling the phenomenon of interest (Fergie et al., 2013). This method was chosen because the study sought to get first-hand information from family members who were involved in any manner in care of the patient. Thus, consenting blood relatives of Lassa fever confirmed patients admitted for not less than 24 h in the Lassa fever isolation ward of the ILFRC and who were with the patient for not less than 24 h prior to and during the time of admission and aged over 18 years were recruited.
Study design
Qualitative research methods were chosen as the study sought to explore the personal experiences of family caregivers of Lassa fever patients, and document in their own words, the range of emotional and psychological states they went through during the period, without presenting them with preconceived options from the researcher (Mohajan and Mohajan, 2018). With the scarcity of published data on the topic, this method generates information that provides the framework upon which future quantitative studies to investigate associations can be conducted.
The study was conducted between December 2017 and March 2018, which coincided with the outbreak of Lassa fever.
Data collection
Focus group discussions (FGD) were used for data collection. FGDs involve organized discussions with a group of persons to gain insight into their views , experiences and perspectives on a topic (Sharif and Masoumi, 2005). This method was chosen as it is easy to conduct, and the interaction of participants in the group allows for the exploration of all the dimensions of a subject matter simultaneously (Vazquez-Lago et al., 2012)
Six FGDs were held with groups consisting of 6 to 9 participants with a mix of educational level, sex and ethnicity in each group. Four scientific officers of ISTH and the head matron of the isolation ward, who had been trained on data collection for a FGD by the researchers, supported with group formation, note-taking, audio cassette recording, time keeping and observation were used. The researchers moderated all the sessions. With the aid of a FGD guide, discussion topics were introduced. Opening, topical and probing questions were asked. Opening questions were typically “icebreakers” that served as preludes to topical questions; they were used to stimulate interest in the group process, and to elicit the participants’ initial perceptions about the general theme. Topical questions directly addressed the topical themes. Probing questions were follow-up questions to obtain more details and clarifications on responses given to topical questions. The general topical themes for the discussions included: awareness of Lassa fever, perceptions of stigma by health workers and the community, sources of emotional and social support, and planned behavioural change in favour of adoption of preventive practices.
The sitting arrangement at each session allowed easy eye contact and hearing between the facilitators and the participants. The participants were encouraged to talk freely and spontaneously. Discussions during the FGDs were written down as field notes and audio taped. Each session lasted for 1 to 2 h as allowed by the participants.
Data analysis
All audio recordings were transcribed verbatim, and speeches recorded in pidgin English were transcribed to English and content-analysed by a process of repeatedly listening to the recordings and reading through the notes, identifying common threads in relation to the questions. Broad themes were coded and used to organize the information hived out from the expressions of thoughts and experiences of the participants. Codes were further broken down into sub-themes. Findings were presented in prose and formed the basis for generating the discussion and recommendations.
Ethical considerations
Ethical approval was obtained from the Research ethics committee of ISTH. Participants were informed that the sessions were to be recorded and played back for transcribing and assured of the confidentiality of information provided. All participants were made to sign an informed consent form prior to the start of each session.
Background information on respondents
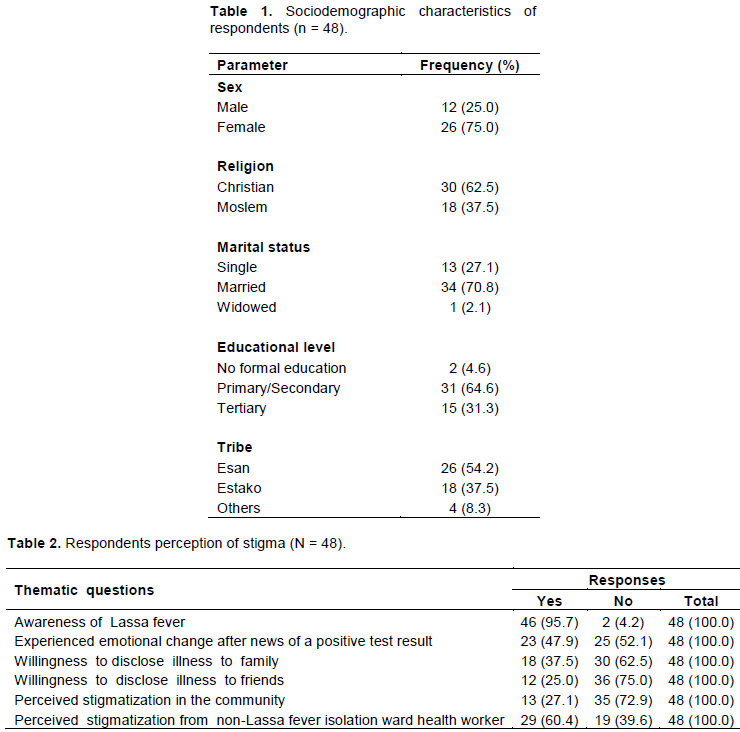
In all, 48 family caregivers participated in the FGDs. Twenty-four (50.0%) of the respondents were in the 26 to 45 years age bracket, 18 (37.5%) were aged ≥45 years, and 6 (12.5%) were ≤ 25 years. The distribution of respondents saw more females, 36 (75.0%) than males 12 (25.0%). Two (4.6%) respondents had no formal education, 31 (64.6%) had primary or secondary level, 15 (31.3%) had tertiary level of education. Twenty-six (54.2%) were of Esan origin, 18 (37.5%) were Estako speaking and 4 (8.3%) were from other tribes. Thirty (62.5%) respondents were Christians and 18 (37.5%) Moslems (Table 1).
Participants were open and actively engaged as sessions were viewed as an opportunity to actively express themselves on a topic they saw as important to their well-being and that of their patients.
Respondents’ awareness of Lassa fever prior to illness encounter
Participants were questioned on their general knowledge of Lassa fever including the vector, mode of transmission and prevention. Almost all respondents had previously heard of Lassa fever from several sources including health workers, school, colleagues, and the media. Two (5.2%) respondents claimed they only knew of the disease when their relatives fell victims (Table 2). One, a 41-years-old male participant only heard of Lassa fever after his brother who had fever and was admitted in a private clinic failed to respond to anti-malarial and Augmentin treatment. He remarked; “For a while the doctor thought we were dealing with fake drugs. Eventually he sent my brother’s blood to Otibhor and the result was Lassa fever”. The second claimed she had never heard of Lassa fever as she lived in Abuja and was spending her annual leave with her mother when the illness began. Four (10.5%) participants described the multimammate rodent vector correctly as the ‘rat with multiple breasts. A 36-years-old male respondent gave the local name for the rodent as ‘Ukhainle’ implying ‘a rat with a bad smell’.
Majority mentioned unsanitary environments, spreading food to sun-dry on the ground, bush burning and leaving raw food uncovered as risk factors for infection.
Most respondents had seen a rat in their house since the year started. Preventive measures mentioned included storing food in covered containers and avoidance of the consumption of garri soaked in water. Most respondents claimed they washed plates and utensils to store away till further use, however the majority admitted they never rinsed stored plates before use, as they assumed the plate was still clean. Majority agreed that cultural practices like sun drying food by the side of tarred roads should be stopped, and some argued for the return of sanitary inspectors to check and enforce sanitation around homes.
Despite this seemingly high level of awareness, a few participants were still of the view that some ‘spiritual force’ was still involved. According to a 31-year-old mother; “I still think somebody is responsible for my child’s illness, not just a rat”. A 45-year-old female participant said, “This my child’s illness is caused by witchcraft, as right from childhood we have been eating rat and have not come down with such an illness ”.
Reaction to the news of Lassa fever positive test result and support received
Participants reported varied responses to a positive test result. Denial, panic, anxiety and fear were common emotions mentioned (Table 2). Common responses in denial of the result were: “God forbid”, “it’s not my portion”, “It is not possible”, “How come?”. A few participants wanted the test repeated out of disbelief. A 30-year-old female said: “When the laboratory called me and told me the result, I was seriously afraid and in fact I started crying and asked God why me?”.
A few expressed anger and initially wanted the test to be re-run to confirm the diagnosis. This was vividly expressed by a 39-year old female participant who said “I was angry at the initial results from the laboratory, because of the seriousness of the disease, I even suspected they had made a mistake in the result. The disease is a serious one”.
A male participant whose relation’s blood sample first came out as negative, and returned positive after a re-run said: “I was happy when the first result came out negative, because I used to hear of one of our village men who died of that disease. But when they called me to say it was positive, I was angry, but what can I do? I eventually had to accept it and hope for the best”.
Some participant however expressed optimism. A 28-years-old female participant said: “As for me, I was not scared when I was told my mother had Lassa fever, in fact I thanked God that the illness can be diagnosed here in the state. I just believed it will be well”. This view was shared by a male respondent whose wife was treated for 4 days without remission of symptoms prior to the confirmation of her illness as Lassa fever. In his words: “I was not afraid since at least now we know what is wrong with her”. A few participants who did not experience any emotional change mentioned they knew someone who had been ill with Lassa fever and survived.
For many participants, these initial reactions eventually transitioned to acceptance of the result and accompaniment of the confirmed case to the isolation ward of the treatment facility. Many participants expressed disappointment over the fact that they were not provided information ahead of the result that would prepare them emotionally and psychological to receive the news, nor were they told what to expect in the coming days, including the purpose for isolating their loved ones. Some respondents however explained that when they confronted their doctors for further information about what next was to be done, they were satisfied with the information given.
Caregiver’s willingness to disclose nature of relative’s illness
The willingness to disclose the nature of disease affecting a loved one can be regarded as a reflection of self-stigma. Self-stigma occurs when people affected by a condition internalize negative public prejudices, stereotypes and attitudes toward them, and as a result experience unpleasant consequence within themselves (Maharjan and Panthee, 2019). Some respondents expressed they were afraid to tell other family members, particularly distant relatives and friends, about the confirmation of Lassa fever in their patient to avoid stigmatization. They feared they may be seen as people with poor environmental sanitation practices who harbour rodents in their houses and may transmit disease. A 36-year-old female participant’s response was: “I chose to hide my brother’s illness because am afraid of the way that neighbours will look at him when he recovers and comes home. ”
A 49-year-old female respondent cited an instance when a patient’s stepfather refused to visit the patient from the time he learnt the ailment was Lassa fever.
She concluded that the stepfather was either ashamed of the illness or afraid that he might become infected.
A 54-year-old woman said: “since the time my husband’s people knew he has Lassa fever; they have refused to visit us here. Even when I tell them I give them hand glove and nose mask; they will say no we don’t want to catch Lassa fever”
In contrast, the response from other participants was that they were not opposed to telling other people the nature of illness affecting their patient. In this group, those who had told others claimed the response they received was generally one of sympathy and best wishes for the sick. Other respondents had to inform relatives to obtain financial assistance. Four respondents needed to inform their employers for permission to take time off work to attend to their patient. They however expressed no fear of losing their jobs from stigmatization. Generally, family members were more likely to be informed of patients’ ill health than friends. Interestingly, one participant said his relatives responded promptly and positively when they heard of the problem (Table 2).
Perceived stigmatization from health workers
A common thread running through all the FGDs particularly from those whose patients were referred from private and public health facilities in neighbouring local government areas and other states was that the care given by health workers to their patients changed dramatically when the Lassa fever confirmatory test result returned positive (Table 2). Such participants reported their relatives were almost abandoned or discriminated against by attending health workers for fear they may contract the disease, leaving caregivers to provide bedside care. During such times, they described the behaviour of the health workers as uncaring and unfriendly. They also felt aggrieved when health workers wore nose masks and hand gloves to attend to their patient, and they were neither given one, nor provided a reason for wearing personal protective gear. As a 47-year-old mother put it: “Imagine the doctor asked for nose mask to attend to my child. What about us his relatives?” As another respondent put it: “The nurses would probably have taken care of my brother if he did not have Lassa fever”.
In the words of a 27-year old female respondent: “I think the nurses and orderlies should have done more of the work as they are trained, and not left it to us. Who are we to complain to?”
A 41-year old female respondent said: “I and the driver that brought me had to carry my husband from the ward to the car. None of the staff there were willing to help me. Can you imagine that? “
Respondents whose relatives were referred from health facilities within close vicinity of the hospital reported less discrimination. An interesting finding was that a few respondents experienced some form of stigmatization from health workers at the emergency unit of the referral hospital, before the patient was transferred to the Lassa fever isolation ward of the treatment centre. Majority of the caregivers were satisfied with the psychological support given to them and their patients by staff in the Lassa fever isolation ward, as the staff were always encouraging them to be optimistic about recovery and kind towards their plight. They also expressed that they were never stigmatized in the Lassa fever isolation ward. They however all expressed that they would have expected to see more of the presence of the nurses attending to their relatives.
Fear of stigmatization from the community
Respondents were generally divided as to whether Lassa fever is still stigmatized in the community or not, with about 13 (27.1%) of the opinion that the disease was stigmatized (Table 2). Those who felt there was no stigma believed awareness of Lassa fever had increased with the sensitization organized by government. Some others opined that Lassa fever was just like any other sickness and could affect anyone. In the words of a 54-year-old woman: “Let them laugh if they want to, nobody knows who will get Lassa tomorrow”. One reason given to support the opinion that Lassa fever was not stigmatized was that they knew of persons who had recovered from Lassa fever and were living peacefully in their communities. Mention was also made of the fact that contact tracing teams from the local government public health department were well received at the homes of confirmed cases when they visited to line list and follow-up contacts.
Other respondents however maintained that Lassa fever still carried stigma in the community. A male participant said he planned to relocate his family to a new apartment when his patient was discharged because he feared what his neighbours will say. One respondent cited the instance of someone she knew who was sacked from work because she was admitted in the isolation ward for Lassa fever treatment.
Perceived stressors during the admission period and sources of psychological support for caregiver
Participants were asked about their emotional state and coping techniques while their loved ones were on admission. Some respondents shared that they were under varying levels of emotional stress borne out of the fact that they were not allowed to see their patients as often as they would have loved to due to the isolation and restricted entry protocol in place in the Lassa fever treatment centre. Some respondents expressed their worry that clinical staff of the isolation ward were not always in the ward to attend to the needs of their patients. A 24 years old female participant said: “My mum has not been sleeping well because my brother is restless at night, and there is no nurse to monitor him.”
The lack of accommodation for caregivers, particularly those who came from distant locations, was also a source of stress as they were exposed to wind, rain, and mosquitoes at night in make-shift shelters around the isolation ward. Three respondents who had vehicles said they slept in their cars.
Respondents claimed their source of emotional succour came from their religious belief that God will heal their loved ones. A 36- year-old female participant said: “When we were admitted, I had to call my pastor and tell my prayer group. I also sent prayer requests to several prayer meetings”. A few others claimed they were encouraged by stories of recovery they heard from survivors who they met in the ward and those in the communities. A 45-year-old female participant said: “One patient told me to calm down, that in a few days my son will be better. That helped me a lot’. Majority expressed satisfaction with the quality of treatment given to their relatives as evidenced by the marked improvement in symptoms since they came to the treatment centre. This was another source of emotional support to them, as they felt hopefully and reassured with the mindset that staff on ground were competent.
The study set out to understand the psychological state of family caregivers of Lassa fever patients with a goal to identify areas where psychosocial support would be beneficial. The high level of awareness of Lassa fever among participants reflects the success of public health education campaigns and sensitization programs organized by the state and local government authorities, WHO, NCDC and ISTH over the years. However, the gaps in knowledge and poor practices that increased individual risk of infection were evident, as some respondents were ignorant of or held misconceptions about the cause of the disease and rodent vector, and some food hygiene practices were poor. These gaps in knowledge and preventive health behaviour should be addressed in future public health enlightenment programs on Lassa fever, especially the washing of eating utensils before use.
Despite the good level of awareness, the initial emotional reactions expressed by some participants on reception of the news of disease shows that some level of fear and dread of the disease still exists in the community. Similar reactions have been documented from studies on other highly infectious diseases (Bali et al., 2016; Van Bortel et al., 2016). This finding highlights the need for emphasis on risk communication to allay the fears of the public and clear misconceptions. Media reports of an outbreak have the capacity to fuel public anxiety out of proportion to the reality of the actual threat of an infectious disease to health especially when official information is either absent or considered untrustworthy (Person et al., 2004). Even in instances where official information is communicated promptly, competition among media houses to gain news popularity and report new developments may lead to an exaggeration of the outbreak, fuel public fears (World Health Organization, 2005). Public health authorities should work with media houses to ensure that messaging on Lassa fever is delivered in such a manner that transfers accurate and concise information with emphasis on allaying fears. It may also be necessary to monitor the content of media reports aired during outbreaks of Lassa fever to ensure that messages do not create panic.
The manner in which laboratory test results are communicated to patients and their caregivers influences the way the result is accepted by the receiver and may contribute to the initial reactions they experience (Monsonego et al., 2011; World Health Organization, 2005). Pre-test counselling at the time when a request for a Lassa fever test is made, and post-test counselling when a result is relayed to the patient, particularly if it is a positive result should be built into guidelines for management of Lassa fever and other viral haemorrhagic fevers.
People affected or infected with a disease would seek more information about the disease from credible sources such as a health provider, and would want to participate in decision making regarding their care (Sengupta et al., 2011). Where the opportunity for such an interaction is non-existent, anxiety, panic and fear set in. Caregivers who perceive a better understanding of a disease are on the other hand less anxious. Health providers should ensure caregivers are provided sufficient information to clear any doubt.
The existence of social stigmatization towards Lassa fever victims was expressed by some participants. Stigma has also been reported in other infectious disease outbreaks (Pappas et al., 2009; Sengupta et al., 2011). Self-stigmatization is reflected in the unwillingness of some participants to inform other persons about their sick patients and has been documented in previous studies (Sengupta et al., 2011). Self-stigma prevents the family caregiver from assessing the financial, material and other resources that would otherwise be available through a wider network of friends, relatives and social groups (Barrett and Brown, 2008; Fischer et al., 2019). Self-stigma needs to be addressed by intensified community sensitization during outbreaks to correct erroneous beliefs about the transmission, and provision of counselling services and psychosocial support to caregivers.
Patients and family caregivers who fear social stigmatization may be unwilling to provide correct information to contact tracing teams to prevent them from visiting their homes. This was observed during the Ebola outbreak in Sierra Leone (Olu et al., 2016). Home visits by contact tracers also have the potential to create tension among neighbours of affected households. Appropriate community messaging on Lassa fever will also help to maintain the balance between the need to implement public health control measures that include exclusionary practices and treatments and a community understands of transmission risk. As was mentioned during the interview, there are reports of people who lost their jobs because they were patients, and were not reinstated until government authorities intervented (Pai, 2019).
Some respondents attested to the marginalization of their patients by health workers in referring health facilities and in the emergency department of ISTH prior to admission in the Lassa fever isolation and treatment centre. This may not be unrelated to the health care workers’ fears of contracting the disease, fear that is amplified by poor understanding of the disease, stories of deaths in health workers from nosocomial infection with Lassa fever during previous outbreaks and the non-availability of personal protective equipment, a perineal problem in public hospitals (Idigbe et al., 2019).
Respondents were generally satisfied with the empathy received from Isolation ward staff. However, the concerns about the less than optimal care provided to their loved ones expressed by some respondents merits attention, as similar findings have been documented in studies that examine the effect of isolation precautions on patients and their family caregivers (Abad et al., 2010). Isolation protocol adds emotional stress to family caregivers (Radtke et al., 2019). It is important that health providers in treatment centres make efforts to mitigate the negative effects of isolation on caregivers by providing patient and family-centred care, while protecting the caregiver from contracting the disease. Identification of a dedicated caregiver, training on infection prevention and control and allowing for timed visits to in-patients may help the caregiver appreciate the peculiarities of case management in an isolation centre and relieve some anxiety. Pre-admission protocols should include counselling to family caregivers. Lassa fever survivors can be called upon to assist with psychological support to caregivers as the study showed some respondents found this action useful.
Strengths and limitations
The study’s limitations and strengths are common to qualitative studies. The low number of respondents may not capture the broader range of views of Lassa caregivers especially from other parts of the country. The interactive nature of the study is a strength as it enabled a broad range of ideas on psychosocial experiences of family caregivers to be explored than would have been possible if another methodology was used for data collection.
Lassa fever continues to exert reasonable psychological strain on family caregivers brought on by real or perceived self and society stigma. Health workers should ensure appropriate counselling of confirmed cases and their families at the times of breaking the news of a Lassa positive test result. Appropriate and sustained community messaging on Lassa fever will help to reduce stigmatization. Stigmatization of Lassa fever patients by healthcare providers in non-Lassa fever treatment facilities should be discouraged. Rather, health providers should be given the necessary training and commodities to build their confidence to support suspected or confirmed cases to referral centres where specific care will be provided. Survivors may be called upon to support psychological services and counselling to patients and family caregivers.
The authors have not declared any conflict of interests.
The authors appreciate the caregivers who participated in this study. The authors are also grateful to the Matron Rebecca Atafo, Rita Esumeh, Benevolence Eboh, Racheal Ominu and Rosemary Giwa who assisted with the conduct of the FGD.
REFERENCES
|
Abad C, Fearday A, Safdar N (2010). Adverse effects of isolation in hospitalised patients: A systematic review. Journal of Hospital Infection 76(2):97-102.
Crossref
|
|
|
|
Bali S, Stewart KA, Pate MA (2016). Long shadow of fear in an epidemic: Fearonomic effects of Ebola on the private sector in Nigeria. BMJ Global Health 1(3).
Crossref
|
|
|
|
|
Barrett R, Brown PJ (2008). Stigma in the Time of Influenza: Social and Institutional Responses to Pandemic Emergencies. The Journal of Infectious Diseases 197(s1):S34-S37.
Crossref
|
|
|
|
|
Bonwitt J, Sáez AM, Lamin J, Ansumana R, Dawson M, Buanie J, Lamin J, Sondufu D, Borchert M, Sahr F, Fichet-Calvet E (2017). At Home with Mastomys and Rattus: Human-Rodent Interactions and Potential for Primary Transmission of Lassa Virus in Domestic Spaces. The American Journal of Tropical Medicine and Hygiene 96(4):935-943.
Crossref
|
|
|
|
|
Cheng C (2004). To be paranoid is the standard ? Panic Response to SARS outbreak in the Hongkong special administrative region. Asian Perspective 28(1):67-98.
|
|
|
|
|
Fast SM, González MC, Wilson JM, Markuzon N (2015). Modelling the propagation of social response during a disease outbreak. Journal of the Royal Society, Interface 12(104):20141105.
Crossref
|
|
|
|
|
Fergie G, Hunt K, Hilton S (2013). What young people want from health-related online resources: a focus group study. Journal of Youth Studies 16(5):579-596.
Crossref
|
|
|
|
|
Fischer L, Mansergh G, Lynch J, Santibanez S (2019). Addressing Disease-Related Stigma During Infectious Disease Outbreaks. Concepts in Disaster Medicine, 1-6.
Crossref
|
|
|
|
|
Idigbe I, Musa Z, Amoo O, Salu O, Ezechi ORA, Omilabu S (2019). Stigma Associated with Lassa-Fever among Healthcare Workers in Ondo State, Nigeria by Ifeoma Eugenia Idigbe Research Fellow Nigerian Institute for Medical Research. In Abstract presented at the Lassa at 50 conference in Abuja, January 2019. Abjua Nigeria.
|
|
|
|
|
Islam MS, Luby SP, Sultana R, Rimi NA, Zaman RU, Uddin M, Nahar N, Rahman M, Hossain MJ, Gurley ES (2014). Family caregivers in public tertiary care hospitals in Bangladesh: risks and opportunities for infection control. American Journal of Infection Control, 42(3):305-310.
Crossref
|
|
|
|
|
Kinsman J (2012). "A time of fear": local, national, and international responses to a large Ebola outbreak in Uganda. Globalization and Health 8(1):15.
Crossref
|
|
|
|
|
Kuriansky J, Toriello AA (2016). The psychosocial aspects of a deadly epidemic: what ebola has taught us about holistic healing. California: ABC-CLIO LLO. Retrieved from
View
|
|
|
|
|
Maharjan S, Panthee B (2019). Prevalence of self-stigma and its association with self-esteem among psychiatric patients in a Nepalese teaching hospital: A cross-sectional study. BMC Psychiatry 19(1):347.
Crossref
|
|
|
|
|
Mmadu-Okoli C (2019). Lassa Fever: Why the Nigerian government should fund disease diagnostics for epidemic preparedness - Nigeria Health Watch. Retrieved October 17, 2019, from
View
|
|
|
|
|
Mohajan H, Mohajan HK (2018). Qualitative Research Methodology in Social Sciences and Related Subjects Qualitative Research Methodology in Social Sciences and Related Subjects. Journal of Economic Development, Environment and People 7(1):23-48.
Crossref
|
|
|
|
|
Monsonego J, Cortes J, da Silva DP, Jorge AF, Klein P (2011). Psychological impact, support and information needs for women with an abnormal Pap smear: Comparative results of a questionnaire in three European countries. BMC Women's Health 11(1):18.
Crossref
|
|
|
|
|
Nigeria Centre for Disease Control (2017). 2016/2017 Lassa fever outbreak in Nigeria: Situation report. Retrieved from
View
|
|
|
|
|
Ogbua O, Ajuluchukwub E, Uneke CJ (2007). Lassa fever in West African sub-region: an overview. Journal of Vector Borne Diseases 44(1):1.
|
|
|
|
|
Olu OO, Lamunu M, Nanyunja M, Dafae F, Samba T, Sempiira N, Kuti-George F, Abebe FZ, Sensasi B, Chimbaru A, Ganda L (2016). Contact Tracing during an Outbreak of Ebola Virus Disease in the Western Area Districts of Sierra Leone: Lessons for Future Ebola Outbreak Response. Frontiers in Public Health 4:130.
Crossref
|
|
|
|
|
Oyebode J (2003). Assessment of carers' psychological needs. Advances in Psychiatric Treatment 9(1):45-53.
Crossref
|
|
|
|
|
Pai B (2019). Lassa fever: Edo state warns against stigmatization - Voice of Nigeria. Voice of Nigeria.
|
|
|
|
|
Pappas G, Kiriaze IJ, Giannakis P, Falagas ME (2009). Psychosocial consequences of infectious diseases. Clinical Microbiology and Infection. Blackwell Publishing Ltd.
Crossref
|
|
|
|
|
Perry P, Donini-Lenhoff F (2010). Stigmatization Complicates Infectious Disease Management. AMA Journal of Ethics 12(3):225-230.
Crossref
|
|
|
|
|
Person B, Sy F, Holton K, Govert B, Liang A (2004). Fear and Stigma: The Epidemic within the SARS Outbreak. Emerging Infectious Diseases 10(2):358.
Crossref
|
|
|
|
|
Radtke K, Dash R, Swoboda S, Lipsett P (2019). Determining the Psychological Impact of Isolation Precautions on Families of ICU Patients.
Crossref
|
|
|
|
|
Richmond JK, Baglole DJ (2003). Lassa fever: epidemiology, clinical features, and social consequences. BMJ (Clinical Research Ed.) 327(7426):1271-1275.
Crossref
|
|
|
|
|
Sengupta A, Rand C, Perl TM, Milstone AM (2011). Knowledge, awareness and attitudes regarding methicillin-resistant staphylococcus aureus among caregivers of hospitalized children. Journal of Pediatrics 158(3):416-421.
Crossref
|
|
|
|
|
Sharif F, Masoumi S (2005). A qualitative study of nursing student experiences of clinical practice. BMC Nursing 4(1):6.
Crossref
|
|
|
|
|
UNICEF (2020). Social stigma associated with COVID-19. Retrieved August 29, 2020, from
View
|
|
|
|
|
Van Bortel T, Basnayake A, Wurie F, Jambai M, Koroma AS, Muana AT, Hann K, Eaton J, Martin S, Nellums LB (2016). Psychosocial effects of an Ebola outbreak at individual, community and international levels. Bulletin of the World Health Organization 94(3):210-214.
Crossref
|
|
|
|
|
Vazquez-Lago JM, Lopez-Vazquez P, López-Durán A, Taracido-Trunk M, Figueiras A (2012). Attitudes of primary care physicians to the prescribing of antibiotics and antimicrobial resistance: a qualitative study from Spain. Family Practice 29(3):352-360.
Crossref
|
|
|
|
|
World Health Organization. (2005). Outbreak Communication Best practices for communicating with the public during an outbreak. Geneva, Switzerland. Retrieved from
View
|
|