ABSTRACT
Diabetes is a complex chronic disease that affects not only an individual’s physical health, but can also have a profound impact on mental wellbeing. The aim of this study was to assess the prevalence of DRD among subjects with type 2 diabetes (T2DM) using Diabetes Distress Scale-17 (DDS-17) and to see its correlation with glycemic control and treatment modalities. A cross-sectional study of 400 T2DM subjects (200 men and 200 women) aged between 25 to 65 years who visited the tertiary care centre for diabetes in South India between April 2017 and May 2018 were included in this study. Subjects with T1DM, gestational diabetes mellitus (GDM) and psychiatric illness were excluded. The total score of DDS-17 was calculated by taking a sum of the 17 items’ results and then dividing the total by 17. Clinical validation of the DDS suggests that the following thresholds of severity should be applied when interpreting the scores: little or no distress < 2.0, moderate distress = 2.0 - 2.9, and high distress ≥ 3.0. The mean age of men and women was 52.0 ± 8.4 and 51.7 ± 8.1 years, respectively. The mean score in women was 2.79 ± 1.52 as compared to men (1.62 ± 0.83) (p<0.001). The study findings highlighted that women had high levels of distress in managing diabetes as compared to men. Diabetes distress should be considered as a significant health problem and steps should be taken for effective management by lifestyle modifications, coping with their stress and diabetes.
Key words: Diabetes distress, HbA1c, emotional burden, type 2 diabetes (T2DM), South India.
Diabetes is one of the most common chronic diseases, estimated to affect more than 400 million people worldwide. Prevalence is predicted to reach 642 million by 2040, and is anticipated to be the 7th leading cause of death by 2030. Diabetes affects not only an individual’s physical health, but can also have a profound impact on mental wellbeing (Mathers et al., 2006; Ogurtsova et al., 2017). It is a complex, chronic disease which requires patient self-management, involving daily decisions concerning diet, physical activity, blood glucose monitoring, and consistent medication adherence (Fowler, 2008). Diabetes complications are a significant cause of increased morbidity and mortality among people. In addition, the substantial burden of impaired functioning and the demands of self management can contribute to significant emotional distress (Deshpande et al., 2008).
Diabetes distress has been defined across domains relating to: diabetic regimen like monitoring of blood glucose, dietary control, increasing physical activity, interpersonal or relational issues, referring to conflicts with careers, partners and friends, emotional burden such as feeling demotivated, unsupported emotionally, misunderstood and worrying about future complications (Polonsky et al., 2005). When an individual is diagnosed with diabetes, the coping resources they possess are insufficient to manage the illness threat, thus triggering emotional distress; that is, they experience high levels of emotional distress stemming from concerns and worries associated with their diabetes and its management (Fisher et al., 2012).
Diabetes distress refers to the unique, often hidden emotional burden and worries that are part of the spectrum of patient experience when managing a severe demanding chronic disease like diabetes (Gonzalez et al., 2011; Schetman et al., 2002). It may be sometimes misdiagnosed as depression and has links to problematic glycemic control and difficulties with self-care behaviors. It causes frustration with diabetes management and patients experience fear about potential complications with erratic blood glucose levels (Fisher et al., 2009, 2010).
Underlying causes of diabetes distress include feeling powerless about controlling diabetes, excessive worries about long-term complications, frustration with management tasks, fear that food constraints are controlling their life, poor confidence with regards to quickly identifying hypoglycemia, fear of embarrassment and potential risk of life, negative social perceptions, fear about being treated differently, less attractiveness to employers, family and friends over or under-involvement, treated as overly fragile and insufficient help or support (Gonzalez et al., 2011; Schetman et al., 2002). There is sparse data available on this topic, hence this study planned to assess the prevalence of DRD among subjects with type 2 diabetes mellitus (T2DM) using Diabetes Distress Scale-17 items (DDS-17) and to see its correlation with glycemic control and treatment modalities.
In this cross-sectional study, 400 T2DM subjects (200 men and 200 women) aged between 25 to 65 years who visited the tertiary care centre for diabetes in South India between April 2017 and May 2018 were included. Patients with type 1 diabetes (T1D), gestational diabetes, cancer, psychiatric illness, and patients unwilling to participate were excluded from the study. DDS2 was first used for preliminary screening purpose to help the subjects familiarize with the content of DDS17. If a patient answered affirmatively to the DDS2 questions, then DDS 17 can be administered to define the extent of the distress.
Diabetes distress scale (DDS)
DDS is a validated 17- item self-report measure with each item scored on a Likert scale from 1 (no distress) to 6 (serious distress) concerning distress experienced over the last month (Fisher et al., 2012; Schetman et al., 2002). The scale yields four reliable subscales via item mean scores: emotional burden (e.g., “feeling angry, scared, and/or depressed when I think about living with diabetes,” “feeling overwhelmed by the demands of living with diabetes”), physician-related distress (e.g., “feeling that my doctor does not take my concerns seriously enough,” “feeling that my doctor does not give me clear directions on how to manage my diabetes”), regimen-related distress (e.g., “feeling that I am often failing with my diabetes routine,” “not feeling confident in my day-to-day ability to manage diabetes”), and interpersonal distress (e.g., “feeling that friends or family do not appreciate how difficult living with diabetes can be,” “feeling that friends or family are not supportive enough of self-care efforts”). The regimen distress scale assesses perceived problems with diabetes self-management. The total score is derived as the mean of all 17 items. Internal reliability of the total scale was excellent (α = 0.95). All scales are treated as continuous variables. Clinical validation of the DDS suggests that the following thresholds of severity should be applied when interpreting scores: little or no distress < 2.0, moderate distress = 2.0-2.9 and high distress ≥ 3.0 (Fisher et al., 2012; Schetman et al., 2002).
Statistical analysis
Values reported are mean ± standard deviation (SD) or number and percentages. Statistical comparison between different groups were made using independent samples t-test and Pearson correlation was done to find out the association between age, HbA1c and distress dimensions and total distress. SPSS version 20 was used for statistical analysis. A ‘p’ value of <0.05 was considered as statistically significant.
The mean age of men was 52.0 ± 8.4 and women 51.7 ± 8.1 years. Table 1 shows the distress levels among men and women. Analysis of DDS-17 results indicated that 77.5% of study subjects had moderate to high DRD based on the total score of the questionnaire. It was found that 22.5% of men and about 55% of women were screened positive for moderate to high levels of DRD on a DDS-17 scale with women having significantly higher DRD levels than men (p<0.001).
Table 2 presents the DDS 17 individual domain scores by gender. In total, analysis of DDS-17 scale indicated that women had higher levels of distress (mean score of 2.79 ± 1.52) as compared to men (1.62±0.83) (p<0.001). HbA1c was significantly higher in women with high combined distress and high emotional distress compared to men. The mean scores for the total and individual components of DDS-17 were analyzed separately. It was found that women showed high distress in emotional burden domain as compared to men. In other domains like physician related, regimen related and interpersonal distress, women showed moderate distress, whereas men showed little or no distress.
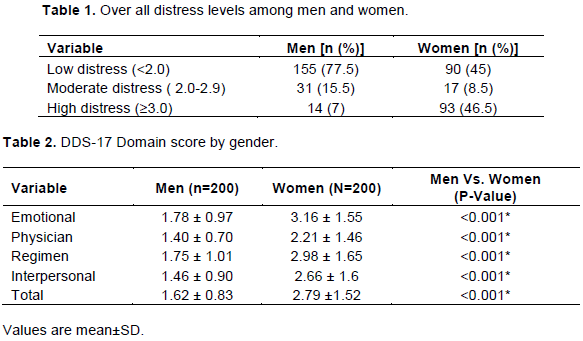
Figure 1A clearly depicts the gender-wise details on emotional burden and interpersonal related distress based on low, moderate and high distress levels among men and women. In emotional burden domain, 55.5% of women showed high distress, whereas it was only 13.5% in the case of men (p<0.0001). In physician related distress, 6% of men expressed high distress levels whereas it was 37% in women (p<0.0001). Figure 1B shows the gender-wise details on regimen and interpersonal related distress based on low, moderate and high distress levels among men and women. Regimen related distress indicated that 11.5% of men and 49.5% of women showed high distress levels. In interpersonal related distress, 14% of men and 2% of women indicated moderate distress levels, whereas 44.5% of women and 7% men indicated high distress level.
Figure 2 shows the distress levels in relation to age groups. It was observed that the levels of diabetes distress decreased with increasing age. On examining the differences between the highly distressed and moderately/ mildly distressed groups, significant relationship was noted between domain scores, age and HbA1c levels. In total, there was a strong statistically significant positive correlation between HbA1c and diabetes distress domain score; emotional burden (r=0.95, p<0.001), physician related distress (r=0.91, p<0.001), regimen related distress (r=0.98, p<0.001) and interpersonal distress (r=0.94, p<0.001). Age also was negatively correlated with individual domain score; emotional burden (r=-0.15, p<0.001), physician related distress (r=-0.15, p<0.001), regimen related distress (r=-0.16, p<0.001) interpersonal distress (r=-0.14, p<0.001) (Table 3).
Diabetes distress is a common health problem which frequently co-exists with T2DM (Islam et al., 2013; Lloyd et al., 2018; Nanayakkara et al., 2018). The present study highlighted that 22.5% of men and about 55% of women were screened positive for moderate to high DRD on a DDS-17 scale. Another study using DDS-17 total scores (Aljuaid et al., 2018) also reported that T2DM subjects were more likely to have DRD especially women when they belonged to the low income, unemployed or had any diabetes complications. Similar results were also observed in our study which indicated high levels of diabetes distress in women.
An earlier study conducted in USA (Fisher et al., 2012) using the DDS-17 scale showed that 51.3% of the screened participants have moderate to high DRD. Similar distress proportions were shown from the studies conducted in Bangladesh (48.5%), China (43%) and Canada (39%) using DDS-17 (Islam et al., 2013; Wong et al, 2017; Zhou et al., 2017). Emotional burden was considered as the most important domain in measuring diabetes distress especially among women. This study finding is consistent with the study conducted in the Bangladesh (Islam et al., 2013) population.
The current study showed a positive correlation between both DRD total score and emotional distress with the glycemic control. It was noted that those who had high levels of DDS had poor glycemic control. Similar finding was also observed in other populations (Islam et al., 2013; Kuniss et al., 2017; Aljuaid et al., 2018). Diabetes related distress generally shows a closer association with glycemic control. This finding is consistent with another study conducted by Gonzalaz et al. (2011). DDS showed closer association with glycemic control than depression and appears to be more common and chronic than depression in adults with T2DM as shown by Fisher et al. (2010). International survey data also confirmed and suggested that emotional well-being is the domain of functioning most negatively affected by diabetes, second only to physical health (Nicolucci et al., 2013).
It was also observed in the current study that as the age increased the diabetes distress levels decreased. This finding is consistent with the earlier study conducted by Fisher et al. (2012) which documented the positive association of DD with age. This may be attributed to their gradual adjustments towards their diabetes life style modifications. The following are the limitations of the current study. Parameters like level of education, socioeconomic status, employment have not been evaluated in association with DDS. Secondly, a comparative level of distress was not assessed in subjects with oral antidiabetic drugs, insulin or combination. The factors associated with DRD should be explained and need to be further studied indepth to formulate proper guidance and empowerment in diabetes management plan.
This study highlights that women had high levels of distress in managing diabetes as compared to men. Diabetes distress should therefore be considered as a significant health problem and steps should be taken for effective management like lifestyle modifications as well as methods to cope with their stress and diabetes.
The authors have not declared any conflict of interests.
The authors appreciate the help rendered by Sriram Ramachandran (Bio-statistician) for analyzing the data and all diabetes patients who participated in the study.
REFERENCES
|
Aljuaid MO, Almutairi AM, Assiri MA, Dhifallah MA, Khaled A (2018). Diabetes related distress assessment among type 2 diabetes patients. Journal of Diabetes Research 1-10.
Crossref
|
|
|
|
Deshpande AD, Harris-Hayes M, Schootman M (2008). Epidemiology of diabetes and diabetes-related complications. Physical Therapy 88:1254-1264.
Crossref
|
|
|
|
|
Fisher L, Mullan JT, Arean P, Glasgow RE, Hesslar D, Masharani U (2010). Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both crosssectional and longitudinal analyses. Diabetes Care 33:23-28.
Crossref
|
|
|
|
|
Fisher L, Mullan JT, Skaff MM, Glasgow RE, Arean P, Hessler D (2009). Predicting diabetes distress in patients with type 2 diabetes: a longitudinal study. Diabetes Medicine 26:622-627.
Crossref
|
|
|
|
|
Fisher L, Hessler DM, Polonsky WH, Mullan J (2012). When is diabetes distress clinically meaningful? Establishing cut points for the Diabetes Distress Scale. Diabetes Care 35(2):259-264.
Crossref
|
|
|
|
|
Fowler MJ (2008). Microvascular and macrovascular complications of diabetes. Clincal Diabetes 26:77-82.
Crossref
|
|
|
|
|
Gonzalez JS, Fisher L, Polonsky (2011). Depression in diabetes: have we been missing something important? Diabetes Care 34:236-239.
Crossref
|
|
|
|
|
Islam RM, Karim MR, Habib SH, Yesmin K (2013). Diabetes distress among type 2 diabetic patients. International Journal of Medicine and Biomedical Research 2:113-124.
Crossref
|
|
|
|
|
Kuniss N, Rechtacek T, Kloos C, Müller UA, Roth J, Burghardt K, Kramer G (2017). Diabetes-related burden and distress in people with diabetes mellitus at primary care level in Germany. Acta Diabetologica 54(5): 471-478.
Crossref
|
|
|
|
|
Lloyd CE, Nouwen A, Sartorius N et al. (2018). Prevalence and correlates of depressive disorders in people with Type 2 diabetes: results from the International Prevalence and Treatment of Diabetes and Depression (INTERPRET-DD) study, a collaborative study mcarried out in 14 countries. Diabetic Medicine 35:760-769.
Crossref
|
|
|
|
|
Mathers ACD, Loncar D (2006). Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine 3:e442.
Crossref
|
|
|
|
|
Nanayakkara N, Pease A, Ranasinha S, Wischer N, Andrikopoulos S, Speight J, de Courten B, Zoungas S (2018) Depression and diabetes distress in adults with type 2 diabetes: results from the Austrailian National Diabetes Audit (ANDA) 2016. Scientific Report 8:7846.
Crossref
|
|
|
|
|
Nicolucci A, Burns KK, Holt R, Comaschi M, Hermanns N, Ishii H, Kokoszka A, Pouwer F, Skovlund SE, Stuckey H, Tarkun I, Vallis M, Wens J, Peyrot M; DAWN2 Study Group (2013). Diabetes attitudes wished and needs second study (DAWN 2):cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes, Diabetic Medicine 30:767-777.
Crossref
|
|
|
|
|
Ogurtsova KJD, Fernandes R, Huang Y, Linnenkamp U, Guariguata L, Cho NH, Cavan D, Shaw JE, Makaroff LE (2017). IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040, Diabetes Research and Clinical Practice 128:40-50.
Crossref
|
|
|
|
|
Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, Jackson RA (2005). Assessing psychosocial Distress in diabetes: development of the Diabetes Distress Scale, Diabetes Care 28(3):626-631.
Crossref
|
|
|
|
|
Schetman JM, Nadkarni MM, Voss JD (2002). The association between diabetes metabolic control and drug adherence in an indigent population. Diabetes Care 25:1015-1021.
Crossref
|
|
|
|
|
Wong EM, Afshar R, Qian H, Zhang M, Elliott TG, Tang TS (2017). Diabetes distress, depression and glycemic control in a Canadian- based specialty care setting, Canadian Journal of Diabetes 41(4):362-365.
Crossref
|
|
|
|
|
Zhou H, Zhu J, Liu L, Li F, Fish AF, Chen T, Lou Q (2017). Diabetes-related distress and its associated factors among patients with type 2 diabetes mellitus in China. Psychiatry Research 252:45-50.
Crossref
|
|