ABSTRACT
In the current conceptualization of disability, the social context plays a fundamental role. Traditionally, the family has been seen as the principal source of support for persons with schizophrenia. It has also been seen as the most reliable support of psychosocial therapies for schizophrenia. Recent research in Chile on the role of the family in defining and managing disability among persons with schizophrenia suggests that in many cases it may play a dysfunctional role. Interviews with care giving families in Santiago, Chile show that the parents and siblings of persons with schizophrenia often manifest and enforce traditional prejudices and attitudes about this mental illness making it difficult for them to lead inclusive, independent lives. Inclusion in society for persons with mental illness and/or incapacity requires that they have well paying full-time employment, and that they have the opportunity to form their own family with a beloved partner. Information obtained from 100 guardians/caregivers of persons with schizophrenia in Santiago, Chile contradicts concepts of inclusion for persons with mental illness and incapacity.
Key words: Schizophrenia, inclusion, family, mental disorders.
Mental disorders have worldwide importance (Patel et al., 2014). Recent research has documented their high prevalence, persistence, and adverse effects in many countries (Kessler et al., 2008). These are very important determinants of the disease burden globally, and have a clear and wide-ranging impact on life-cycle outcomes such as educational achievement, employment performance, marriage and divorce, and every day functioning (Alonso et al., 2014). The quality of life of individuals with mental disorders depends upon effective treatment, receiving support in the community, and their social inclusion (Padmavati, 2014; Leff and Warner, 2006). Since the mid-1960s, de-institutionalization has emptied large state-run asylums for the severely mentally ill in most industrialized nations and in some developing countries (Brazil, Chile and Panama) in Latin America (Minoletti,2016). The integration of persons with serious mental disorders in societies world-wide remains a very challenging problem (Okpaku and Biswas, 2014). Families of these individuals, when they are in contact with them, play a crucial role in their treatment and inclusion in social and economic roles (Neri, 2012).
Mental disorders in Chile, like other Latin American countries, are highly prevalent and have a substantial emotional cost (Minoletti et al., 2016; Vicente et al., 2006). Epidemiological surveys in Chile report that between 13 and 23% of adults have a current mental illness (Minoletti, 2012; Vicente et al., 2006). The most common lifetime diagnoses are agoraphobia, major depressive disorder, dysthymia, and alcohol dependence. There is limited survey data on the prevalence of other severe mental disorders. However, patient data suggests that 5% or more of adult Chileans have severe mental disorders including schizophrenia (Mundt et al., 2016; WHO, 2007). This prevalence rate of severe mental disorders puts them in the range of the United States which reports 4% for its adult populations (NIMH, 2017). Chile is one of the most progressive countries in Latin America in addressing the mental health needs of its citizens. Major mental health program reforms occurred there in 1993 and 2000 (Araya et al., 2001; WHO, 2007). With these major organizational changes, policy makers decentralized mental health services from large hospitals, where services were outmoded and there were reported human rights abuses, to community clinics where mental health care and education was integrated with primary care.
In the community clinics, patients with severe mental disorders such as schizophrenia, which required a higher level of treatment, were referred to specialized centers for more complex mental illness. After they were treated and stabilized, they returned to the community clinics where they saw primary care physicians who monitored them and maintained their treatment. The community based clinic mental health reforms which combined mental health services with primary care increased access to care and the number of Chileans receiving treatment (Ministry of Health (Chile), 2008). Another innovation associated with the reform and decentralization of mental health services has been the development of psycho-education interventions to reduce the burden of care and increase morale of caregivers (Gutierrez-Maldondo et al., 2008; Guitierrez-Maldondo, 2007). Currently, systematically evaluated, education programs with families of schizophrenics have reported positive outcomes for both caregivers and patients (Cavieres, 2017).
Although there have been major reforms and improvements in mental health services over the past 25 years in Chile, which have increased access to treatment and the number of individuals receiving treatment, the social and economic inclusion of adults with severe mental illness, particularly those with schizophrenia, is very limited (Chuaqui, 2015). The large majority of these individuals are unemployed and of those who are in the workforce, most are in "protected" jobs rather than in competitive well-paying positions. Furthermore, less than 25% of adults with schizophrenia in Chile live with a partner (most are separated or never married). In addition, social stigma against persons with mental illness continues to exist in most communities despite legal reforms and education programs against it (Chuaqui, 2015). Given this situation of isolation and social segregation of persons with schizophrenia in Chile, the family has a crucial role because it is the primary source of their social support in the community. Therefore, the problem of this study is the variable efficacy of the Chilean family in supporting the social inclusion of their adults with schizophrenia in Chilean society.
Research questions
This study addresses two interrelated research questions: First, what is the role of the family in the social inclusion of adults with schizophrenia in Chile, and second, how does the family help these severely mentally impaired individuals meet key objective and subjective criteria of social inclusion?
Theoretical orientation
To address the research questions, we specified theoretical dimensions of social inclusion and then developed measurable criteria. This process was guided by the theoretical concepts and insights of the classical sociologists George Mead, Max Weber, and Emile Durkheim. Following the work of Mead (1973), we assume that the integration or inclusion of persons with schizophrenia (or other severe mental illness) in society requires that they assume social roles (for example, worker, partner or spouse, home owner or renter) that are personally fulfilling and esteemed by others in the community. We also accept the premise of Weber (1946) that individuals' personal goals (for example, work in a particular profession or area, have a partner, reside in a private home or apartment) originate in society and are socially sanctioned. Furthermore, after the work of Durkheim (1993), we maintain that complete social inclusion of persons with schizophrenia (or other severe mental illness) is a type of organic solidarity in which persons attain personally fulfilling work, relational, and residential goals in ways that conform with accepted community norms and are valued by others.
Objective and subjective criteria of full inclusion
To specify the study objective and subjective criteria of social inclusion, we applied the work of Schneider and Bramely (2008), and were informed by earlier work of Reker (1993) and Mikulsa-Meder (1992). The objective criteria of full social inclusion are:
(1) Have a well-paying personally fulfilling full-time job.
(2) Form a committed relationship or family with a spouse or partner.
(3) Live in your own apartment or house.
These objective standards are complemented by several subjective criteria:
(1) Individual psychosocial development is guided by personal values.
(2) Job, or work role, reflects vocational commitment and mental and physical capabilities.
(3) Occupational, relational, and residential inclusion produces increased autonomy and empowerment.
Sample
With the assistance of the National Health Service in Santiago, we recruited 100 adult schizophrenia patients and their guardians for this clinical sociology study. An attempt was made to recruit patients and guardians/caregivers who were representative of a wide social spectrum of Chilean society. Therefore, most of the patients received treatment in public mental health clinics while some others were treated in private clinics. All of the patients were considered to be medically compensated as a result of their medication and behavioral therapy. While it is assumed that the study patient sample and the sample of their guardians are representative of most schizophrenia patients and their guardians in Chile, there is no national database to which we can compare them. Furthermore, it must be emphasized that this is a clinical sample of individuals (schizophrenia patients and their guardians) who are difficult to enroll in a study. Their selection followed a purposive procedure as opposed to the random process utilized to obtain community samples. Following informed consent procedures of the National Fund for Scientific and Technological Development (FONDECYT), the Ministry of Health of the Government of Chile, and the University of Valparaiso, the consenting patients and guardians were interviewed by staff of the study project, "Schizophrenia and Family Discrimination, " (Chuaqui, 2015).
Measures
Demographic variables
The socio-demographic variables for patients included gender, age, education, employment status, marital status, relationship to guardian, aspiration for work, and aspiration for a partner. For the guardians of the patients, we had measures of occupational status and relationship to their patient. Age was a continuous measure, education was categorized by primary education, secondary education and higher education, employment status reflected employed in a competitive job, working in a protected or family position, and not in the workforce. Occupational status for guardians included a prestige based continuum of positions beginning with not working up to business executive in a large corporation. Relationships of patient to guardian and guardian to patient were indicated by categories of immediate and extended family members, and the coordinator/monitor in the group home where the patient resided. Also patients were queried about the type of job and personal relationship they aspired to have.
Patient behaviors
Guardians were given lists of behaviors that schizophrenia patients typically manifested when they were in crisis and when they were mentally stable due to medical compensation. Using a scale of 1 to 10, the guardians reported the extent to which each behavior, for example, aggressive verbal behavior, was a problem for them with the patient for which they were responsible. The higher the score assigned by the guardian to a specific behavior, for example, tries to harm him/herself, the less of a problem the behavior was perceived to be by the guardian. For the purpose of the data presentation, we grouped all of the guardian ratings of 1 to 5 on specific behaviors as indicating "more importance" and those rated 6 to 10 as "less important."
Qualitative data
The guardians were also asked to provide qualitative information on their relationships with their respective patients. Similarly, the patients were asked to describe their relationships with their guardians. The objective in gathering the qualitative information with open-ended questions was to give the guardians an opportunity to express in detail their level of satisfaction with their relationship with their patient and for the schizophrenia patients to do the same regarding their interactions with their guardian.
Analytic strategy
Using the study objective and subjective criteria of social inclusion, we addressed the research questions regarding the role of the family in the social inclusion of adults with schizophrenia in Chile with quantitative and qualitative data.
Sample characteristics
The study patient sample is evenly split between males and females (50.9 to 49.1). Most of the participants are grouped in the middle age ranges (25 to 49, 71.4; 50 to 74, 23.2). They are predominantly unemployed (46.4), or work in protected jobs (37.5), while less than one in five (16.1) are in the competitive work force. Very few (1.8) are married and live with their partner. The rest of the patients live alone. Nevertheless, almost half of the participants (0.45) reported that they wanted a stable relationship, and the large majority (0.74) want to work (Table 1).
Relationship
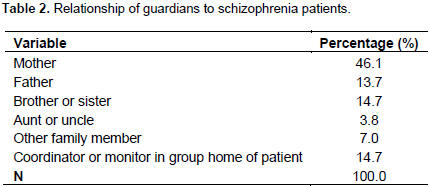
Most of the patients had a guardian who was an immediate (74.5) or extended (10.8) family member, while less than one in five (14.7) depend on a coordinator or monitor in a group home for this role (Table 2).
Occupation
The guardians were from households that predominantly were headed by individuals with occupations that were of high (36.6) or medium (29.5) prestige. Other smaller groups (28.6) were from working class families while a small percentage (5.3) lived in homes where the "bread winner" was unemployed (Table 3).
Patient behaviors
Using a list of behaviors that schizophrenia patients typically manifest (Ministry of Science, 2009) when they are in crisis, they show physical aggression, 45.1; shows verbal aggression, 51.0; destroys furnishings, 37.2; leaves home, 27.4; problems with neighbors, 24.5; legal problems with police, 24.2; strange behaviors, 56.8; attempts to hurt self, 30.4; difficult to control, 46.1; difficult to attend medical appointments, 39.2; withdraws into self ,64.7; remains in house, 49.0 (Table 4).
.png)
Guardian perceptions when patients are stable
The guardians also reported behaviors that schizophrenia patients often exhibit when they were stable (as a result of medical treatment): rarely speaks, 49.0; cannot live alone with economic support, 79.4; cannot live alone and meet economic needs, 84.3; skilled liar, 27.5; lack of personal hygiene, 22.5; unhelpful with household chores, 48.0; behaves in strange ways, 26.7; shows verbal aggression,16.7; acts like child, 46.0; not capable of a relationship, 72.5; withdraws into self, 52.9; remains in the house, 37.3 (Table 5).
Despite a progressive institutional environment in Chile, which supports the global objectives of social inclusion of persons with mental illness, including severe mental illness, the data collected in this study of a sample of adult men and women with schizophrenia shows very limited progress toward this goal. We found that the study objective and subjective measures of social inclusion, the patients with schizophrenia we interviewed remained for the most part marginalized. Although about 75% of the patients had secondary school or higher education, less than 20% worked in the competitive economy. Almost half were unemployed and about 40% performed protected work. Therefore, among this group of patients, relatively few could support themselves or make a significant financial contribution to support a household with a partner. This lack of resources is reflected in the fact that less than 2% of the patients reported being married. Overall, this group, in part was not fulfilling traditional adult work and martal/relational roles and was economically dependent on other family members and was vulnerable to thedebilitating stigma that is attached to the mentally ill in Chile and elsewhere.
Despite the social and economic marginality of this group, three out of four patients with schizophrenia said that they wanted to work, and almost half of them desired a stable personal relationship. The large gap between aspiration and reality for the large majority of the patients suggests that they experience a low level of life satisfaction and happiness.
The responses of the guardians in this study, about 85% of whom were members of the schizophrenia patients' immediate or extended family, suggest that the family in Chile primarily protects members who are severely mentally ill from harming themselves or others in the community, tries to assure their compliance with medical treatment and psycho-social therapy, and generally encourages them to assume to the sick role and adapt to traditional norms regarding persons with mental illness. This protective (as opposed to empowering) behavior of the guardians is rooted in basic attitudes expressed by them regarding their patient/family member who was being treated and was stable.
Around 80% said that the patient was not capable of living alone regardless of the availability of financial support. 70% had the opinion that their patent was not capable of having a stable relationship, and nearly one-half of them reported that their patient acted like a child and rarely speaks with family and friends. Despite their protective behavior and traditional attitudes toward their patient, there is qualitative evidence that they are dissatisfied with how they are performing their guardian role. This is a negative sentiment also voiced by guardians/care givers of adults with mental illness in other studies (Padavati, 2014; Neri et al., 2012; Gutierrez-Maldonado and Caqueo-Urízar, 2007). One of the study guardians, who was probably representative of the group, made the following observation:
"I think the most terrible thing for a human being, and for a mother, is to have to make decisions for another. I told the doctor...I prefer, however terrible it may be, for a person to lose a foot. Even if he loses a limb or his sight, he still has his mind and can make decisions. However, to be dependent on others to make decisions is the most terrible thing there is."
The guardian's angst was echoed in the words of one of the schizophrenia patients who felt over-protected and longed for greater autonomy.
"A lot of overprotection, they have overprotected me a lot. They have accustomed me to overprotection, and I know that this state cannot last forever. It does not empower me, but I have a desire to be more autonomous and to grow as a person."
In the analysis of the role of the family in the social inclusion of adults with schizophrenia in Chile, we have found that the guardians generally do not believe that the patients for which they have legal responsibility are capable of attaining major goals of social inclusion, that is, holding a job in the competitive economy, maintaining a stable personal relationship, or living alone with or without family financial assistance. Further, they do not appear to endorse the subjective criteria of inclusion for the patients, that is, empowerment and autonomy. Despite these findings that indicate that the families play a protective role toward their patients, there is also evidence that they are not comfortable in this type of role. Furthermore, this data can be interpreted with a different concept or lens. In this alternative case, we would substitute the concept of integration for that of inclusion. Applying this more limited concept, we assume that integration is achieved when the person follows social norms, even if they do not work in the competitive economy, maintain a stable personal relationship, or live alone on their own resources.
Taking the clinical perspective of most health professionals, patients are integrated or have achieved "normalization" when they follow treatment norms/schedules, and are medically stabilized and exhibit "normal" social behavior.A key point here is that the processes of social integration and inclusion can, and often do, coincide. When a schizophrenic patient, or other person with severe mental illness, lives with their family of origin and has no major conflicts with them, is compliant with treatment, and is not perceived by others as a threat to themselves or the community, they have a much better quality of life than if they lived permanently in a mental hospital. Nevertheless, we believe that for these individuals we should continue to attempt full social inclusion as indicated by residential independence, good employment in the competitive economy, and maintenance of a long-term personal relationship or marriage. The trend toward social inclusion of those with severe mental illness is now clear in Chile and in other countries of Latin America. What we have attempted to do with this analysis is to show the family barriers to social inclusion that continue to exist. There must be cultural change of both families and health professionals in support of greater social inclusion. At present, there are social movements of persons with diagnosed disorders who are calling for legal and structural reforms. A new mental health law is being promoted in Chile.
The authors have not declared any conflict of interests.
James G. Linn,Ph.D. is grateful to the University of Valparaiso program," Academic Visits", which made it possible for him to be a Visiting Professor and contribute to the research activities and this manuscript.
REFERENCES
|
Alonso J, Chatterji S,He Y, Kessler R (2014). Burden of Illness in Essentials of Global Mental Health. In Samuel O. Okpaku eds. New York: Cambridge University Press. pp. 11-24.
|
|
|
|
Araya R, Rojas G, Fritsch R, Acuna J, Lewis G (2001). Common mental disorders in Santiago, Chile; prevalence and socio-demographic correlates. Brit. J. Psychiatry. 178:228-233.
Crossref
|
|
|
|
|
Cavieres A (2017). Psycho-education interventions implemented in clinical settings in Chile. Presentation given in the seminar, The role of the family in the social inclusion of persons with schizophrenia, July 18, 2017, School of Medicine of the University of Vapariso, Valparaiso, Chile.
|
|
|
|
|
Chuaqui J (2015). Sociology of Health: Chile 2008-2015. Santiago: RIL Publications, pp. 25-91.
|
|
|
|
|
Durkheim E (1993). The Rules of the Sociological Method. Madrid, Morata. pp. 52-76. Available at:
View
|
|
|
|
|
Gutierrez-Maldonado J, Caqueo-Urízar A (2007). Effectiveness of a psycho-educational intervention in Latin American families of patients with schizophrenia. Qual. Life Res. 16(5):739-47.
Crossref
|
|
|
|
|
Gutiérrez-Maldonado J, Caqueo-Urízar A, Ferrer-García M (2008). Effects of a psycho-educational intervention program on the attitudes of health perceptions of relatives of patients with schizophrenia. Soc. Psychol. Psychiatric Epidemiol. 44(5):343-348.
Crossref
|
|
|
|
|
Kessler RC, Angermeyer M, Anthony JC, De Graaf RON, Demyttenaere K, Gasquet I, Kawakami N (2008). Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health
|
|
|
|
|
Leff J, Warner R (2006). Social Inclusion of People With Mental Illness, New York: Cambridge University Press. pp. 9-87.
Crossref
|
|
|
|
|
Mead G (1973). Spirit, Person, and Society. Barcelona, Paidos. pp.1-50.
|
|
|
|
|
Mikulsa-Meder J (1992). Clinical state of patients with schizophrenia who are employed and unemployed. Psychiatric Policy 26(1&2):97-103.
|
|
|
|
|
Ministry of Health (Chile) (2008). Health Facilities, Santiago, Chile.
|
|
|
|
|
Minoletti A (2016). The Reform of Mental Health Services in Chile:1991-2015. Paris: Psychiatric Information pp.1-90.
|
|
|
|
|
Minoletti A, Sepúlveda R, Horvitz-Lennon M (2012). Twenty years of mental health policies in Chile. Int. J. Mental Health. 41(1):21-37.
Crossref
|
|
|
|
|
Mundt A, Kastner S, Larrain S, Fritsch R (2016). Prevalence of mental disorders at admission to penal systems in emerging countries: A study from Chile. Epidemiol. Psychiatric Services. 5(5): 441-449.
Crossref
|
|
|
|
|
Neri AL, Yassuda MS, Rojas M (2012). Relationship between gender, age, family conditions, physical and mental health, and social isolation of elderly caregivers. Intern. Psychogeriat. 24:472-483.
Crossref
|
|
|
|
|
NIMH (National Institute of Mental Health) (2017). Prevalence of mental disorders in the United States. Available at www.nimh.nih.gov./health/statistics
|
|
|
|
|
Okpaku S, Biswas S (2014). History of Global Mental Health in Essentials of Global Mental Health. Samuel O. Okpaku. New York: Cambridge University Press. pp. 1-10.
Crossref
|
|
|
|
|
Padmavati R (2014) Stigmatization and Exclusion in Essentials of Global Mental Health. Samuel O. Okpaku. New York: Cambridge University Press. pp. 85-92.
Crossref
|
|
|
|
|
Patel V, Minas H, Cohen A, Prince M (2014). Global Mental Health: Principles and Practice, New York: Oxford. pp. 3-26.
|
|
|
|
|
Reker T, Andrews A, Chetnee R (1993). Current practice of psychiatric occupational rehabilitation. Psychiatric Praxis 20(3):95-101.
|
|
|
|
|
Schneider J, Bramely C (2008). Towards social inclusion in mental health. Advances in Psychiatric Treatment 14(2):131-138.
Crossref
|
|
|
|
|
Vicente B, Kohn R, Saldavia S, Baker C, Torres S (2006). Lifetime and 12th month prevalence of DSM-III-R disorders in Chile. Am. J. Psychiatry. 163(8):1362-1370.
Crossref
|
|
|
|
|
Weber M (1946). Essays in Sociology. New York, Oxford. pp. 114-139.
|
|
|
|
|
WHO (World Health Organization) (2007). Research on mental illness prevalence in Chile.
|
|