ABSTRACT
Voluntary counseling and testing (VCT) for HIV is essential and critical way for prevention, care and treatment of HIV. It allows early detection of illness, reducing transmission, morbidity and mortality from it. But youth knowledge and attitude towards HIV testing services is not universal. The aim of this study was to assess knowledge, attitude, practice and factors associated with VCT for HIV among University Students in Ethiopia. Institution based cross sectional study was conducted among University students in Ethiopia using pretested, structured self-administered questionnaire. Single proportion formula was used to calculate the sample size (361). Multistage sampling with stratified sampling technique was used. Data was analyzed using SPSS version 16.0 with chi square test, bi-variate and multivariate analysis via OR, AOR, p-value and confidence interval. Binary logistic regression was used. Out of 361 sample 93.6% of them responded, with 178 (52.7%) male and most are below 25 years. Majority were single, orthodox in religion, and from urban residence. 86% of them have heard of voluntary testing for HIV and know that having early test will prevent future spread of HIV. Based on the scoring 66% are knowledgeable about VCT. Almost 60% of participants were willing to undergo the test and 80% advices their friends to have test. Also 40.5% had good attitude toward test for HIV and 65.7 and 29.6% were ever tested and tested in the previous year respectively. Fear of HIV test results, stigma, and service related factors were major barriers for testing. Being male (AOR=1.607, CI: (1.01-2.57) p value= 0.047) and first year (AOR= 3.25, 1.33 – 8.83) were significantly had lower odds of being knowledgeable than females and seniors respectively. Those who were not knowledgeable have two times odd of poor attitude (AOR=1.901(1.20-3.02) P=0.006)). Students from urban (AOR=2.088, CI: (1.273- 3.425) P=0.004), unseparated family (AOR=2.24CI: (1.02-4.92) P=0.045) and with poor attitude (AOR= 1.76 CI: (1.08-2.89) p=0.024) were more likely not to have test than counterparts. Knowledge and attitude towards HIV testing is not satisfactory. Freshman students are the target for behavioral interventions. Improving awareness and attitude of students through peer to peer discussion and other packages is crucial to increase the practice and ultimately combat HIV in higher institutions.
Key words: Attitude, HIV/AIDS, Knowledge, University, voluntary counseling and testing (VCT), associated factors.
Abbreviation:
A/OR, Adjusted/ odds ratio; CI, confidence interval; HIV/AIDS, Human immunodeficiency virus/acquired immunodeficiency syndrome; VCT, voluntary counseling and testing.
HIV/AIDS remain major public health concern worldwide. Globally, 34.0 million people were living with HIV at the end of 2011. Estimated 0.8% of adults aged 15-49 years worldwide are living with HIV. Even if it is global pandemic, Sub-Saharan Africa remains most severely affected, where 4.9% of adults are infected. Thus this region account for 69% of the people living with HIV worldwide. Caribbean, central Europe and Asia have 1% prevalence of HIV among adults (UNAIDS, 2012). In Ethiopia, sero prevalence rate of 1.5% among 15-49 aged population with highest rate occurring among women (1.9%) and 1% among men (EDHS, 2011). HIV/AIDS goes beyond public health concerns because it primarily affects adult populations which greatly undermine the social and economic structures of developing countries (Admassu et al., 2006). Owning to this great burden of infection, Ethiopia has launched different prevention strategies like condom promotion, HIV counseling and testing, behavioral changes and others since 1985 (FHAPCO, 2007).
There are three options of HIV testing and counseling namely voluntary counseling and testing (VCT), client initiated and mandatory HIV screening. VCT is one of effective strategy in tackling HIV/AIDS (WHO, 2003).
VCT is essential and critical gateway for HIV prevention, care and treatment. Thus this allows early detection of illness, reducing transmission, morbidity and mortality from it (FHAPCO, 2007). VCT is also an effective strategy for facilitating behavioral change for both clients, whose test result is either negative or positive (FHAPCO, 2007; Zelalem et al., 2013). Testing for HIV is advocated as international arena for HIV prevention. The Ethiopian government developed guidelines since 1996 focusing on couple, youth and other VCT for HIV. It is also showed that VCT is instrumental in bringing about behavioral change, reducing unprotected sex and helping reduce the incidence of HIV and other sexually transmitted diseases (Admassu et al., 2006).
It has potential preventive effects on HIV transmission and serves as a gate way to other services. It includes both testing for HIV status and counseling on different issues. Counseling should guarantee confidentiality and include information about HIV transmission and personal discussion about an individual’s risk. This enables people to make informed decisions about their future. Thus upgrading and expanding this service is critical for preventing HIV pandemic among youths (WHO (2003). Thus youth friendly counseling is appropriate for this age group.
Testing for HIV (VCT) is the process by which an individual undergoes counselling which would enable him or her to make an informed choice about being tested for HIV. It has comprehensive role in prevention of HIV. Knowledge and attitude towards VCT is not universal (FHAPCO, 2007; Awoke and Yilma, 2008). Despite its great role uptake or utilization rate is poor mainly due to poor behavioural education communication, attitude and fear of stigma and result especially among youths (Awoke and Yilma, 2008).
Various studies showed low VCT utilization and poor attitude towards VCT but adequate awareness among university students. Fear of HIV test results, stigma, and not feeling at risk of HIV infection were major causes for non-uptake of VCT among university students (Abiy et al., 2009; Leta et al., 2012; Museve et al., 2013; Meda, 2013; Zelalem et al., 2013). Another study shows that the level of knowledge towards VCT, being male, senior student and attitudes of students about VCT are associated with VCT uptake (Tsehaye et al., 2010). Among students in the year before study, only 43.5% were tested (VCT registration, 2013).
University students are mostly in adolescent age group accompanied with freedom from family control may increase risk of acquiring HIV/AIDS. In contrast VCT is one main behavioural tool to combat the pandemics. Its use is determined by perception and other related factors. Thus this present study aimed to assess the knowledge, attitude and utilization of VCT and its associated factors among university students in Ethiopia. It will also inform concerned bodies with the current body of the problem among university students. It will ultimately help in planning appropriate, accessible, safe and confidential HIV counselling service in campus. It will show level VCT utilization among students and factors which hinder utilization, giving strategic directions and possible optional interventions to halt HIV pandemic among adolescent in university.
Study design
Institution based cross sectional study was carried out among regular Wolkite university students in South Ethiopia. It is found in Ethiopia, located around 169 km from capital city Addis Ababa. In 2013/14 academic year, a total of 3715 students under seven colleges with above 30 departments were enrolled. The university has one student clinic with one VCT center. In previous academic year VCT service served 616 students with counseling. But in 2013/14 academic year it was not functioning well. It was conducted from May 18 to 26, 2014.
Sampling and sample size
Multistage sampling was employed to access the study units. First it was stratified in to seven colleges; out of this four colleges were selected by simple random sampling method. Then three departments from each of the four selected colleges were selected departments from each of the four selected colleges were selected by simple random sampling. Considering that the student’s year of stay may affect their VCT uptake, the sample size per department was proportionately allocated. Thus the total sample size was allocated proportionately to each selected college, department, and year of study based on total population per stratum. Sample size was proportionally allocated to four selected colleges. And then departments were selected from each college to make sample representative.
Single proportion formula was used to estimate adequate sample size using prevalence of having VCT from other similar study as 0.585 (Girmay et al., 2011), marginal error 5 and, 95% confidence interval and total size of 3714(N).
Where n is sample size, taking marginal error (d) as 5 at 95% Confidence interval.
Thus the sample size became 360 and since the total population is less than 10,000, correction formula was used the sample size become 328. Finally considering non response rate of 10%, the final sample size became 361.
Data collection and analysis
Data was collected using pretested self administered questionnaire consisting of socio demographic information, knowledge, attitude and practice and some associated factors questions. Pretest was conducted in similar university on 36 students. Based on feedback from respondents and the analysis of pretest data necessary amendment in language, measurement, way of questioning and other areas was done. Final draft of tool was used for actual data collection. The data collected on knowledge and attitude was score based on the cutoff point above mean of the sum points of each questions. Correct answer was labeled as one and the counter part as zero. Thus value above mean of all respondent was considered as knowledgeable and good attitude. While counter parts are labeled as not knowledgeable and poor attitude.
Data was entered to SPSS version 16.0. Then it was analyzed via descriptive statistics like frequency, crosstabs and tables. Both bi-variate and multivariate analysis was carried out. To identify factors associated with the outcome variable binary logistic regression was used. The outcome variables are knowledge level, attitude towards VCT and practice of VCT. All the three dependents are binary outcomes. A significant level of 0.25 at bi-variate analysis and some important variables from previous studies were considered for multivariate analysis. Sex, family place of residence, year of study, having boy/girlfriend are some of the variables included in multivariate analysis. Both crude and adjusted odds ratio (AOR) were calculated with their 95% confidence interval and P value. Also mean comparison via t- test and ANOVA was used to test whether the knowledge and attitude score varies between groups. A P value below 0.05 was considered as statistical significant association.
Data quality was assured through care full training for data collectors, close supervision during data collection, pretested questionnaire and daily checks of the collected data was applied. The research was reviewed and ethically adopted by the university independent Research ethical review committee. Then a written informed consent considering their free will to participate in the study, confidentiality of their information and each participant was giving informed consent on separate paper and then they are eligible for the questionnaire. All possible ethical cares were respected throughout conduct of this research project.
Socio demographic Information
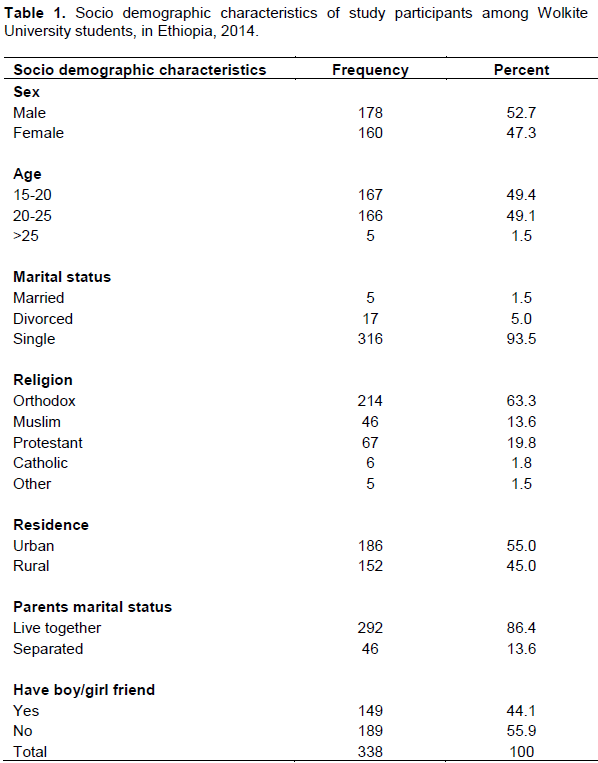
From total sample of 361, 338 (93.6%) responded to the questionnaire, and, 178 (52.7%) were males. Majority of study participants 333 (98.5%) were below 25 years old, 316 (93.5%) were single, 17 (5%) were divorced. Over two thirds 214 (63.3%), 67 (19.8%), and 46 (13.65) were orthodox, protestant, and Muslim religion. More than half (55%) are from urban resident. Almost half, 153 (45.3%) of their family livelihood depend on farming, while 8 (26.3%) work as government employees. Majority, 292 (86.4%) of parents of study respondents lived together (Table 1).
Knowledge and attitude towards VCT
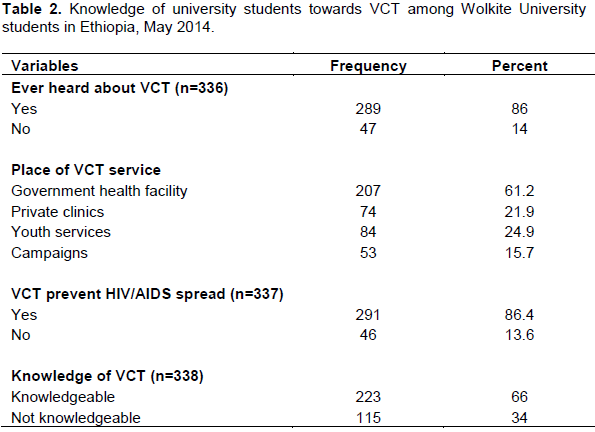
Out of 336 respondents, 289 (86%) ever heard of VCT for HIV. Among those who have heard of VCT, 219 (66.8%) got information from mass media and 45 (13.7%) and 28 (8.5%) got it from anti AIDS clubs and friends respectively. Almost all 336 (99.4%) know that it is important for person to undergo VCT. Regarding place where VCT is given 207 (61.2%) mentioned government health facility, while 84 (24.9%) and 74 (21.9%) mentioned youth clubs and private clinics respectively. Majority, 291 (86.4%) know that early VCT for HIV prevents its future spread. Only 145 (45.3%) responded positively to the question that obese and healthy looking people may have HIV infection. And almost two thirds 223 (66%) are knowledgeable about VCT, while the rest are not knowledgeable. The mean knowledge and attitude scores were not significantly different between male and female (p value >0.05) (Table 2).
Attitude and practice towards VCT
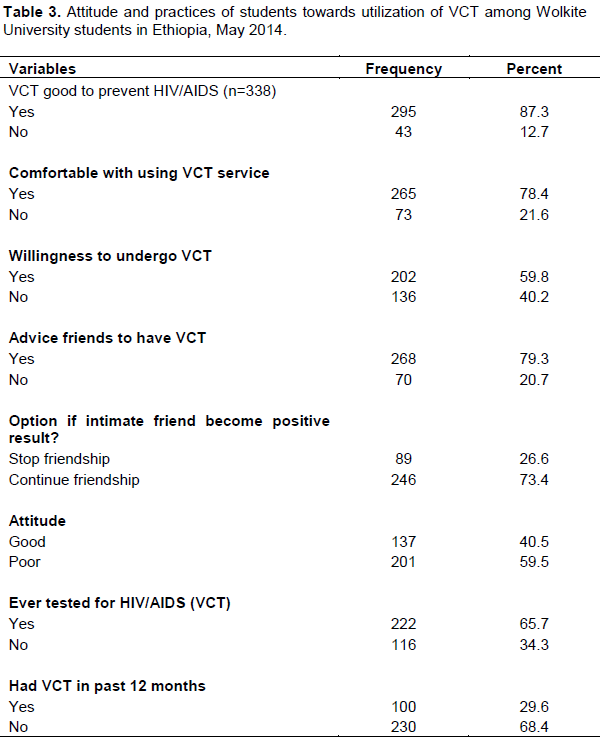
More than three fourth of them 295 (87.3%) and 265 (78.4%) perceive VCT as good and they were comfortable in VCT service respectively. While 202 (59.8%) were willing to undergo VCT and 268 (79.3%) would advise their friends to undergo VCT. Interestingly 246 (73.4%) said that they would continue their friendship if their intimate friends gets positive HIV test result (Table 3.).
About 222 (65.7%) of students had ever undergone VCT, while only 100 (29.6%) have had VCT in the past year. Among those who had tested, 119 (35.2%) and 78 (23.1%) had undergone VCT at government institutions and private clinics respectively. Regarding habit discussion with parents about HIV and other sexual issues 185 (54.7%) had habit of discussion. 211 (62.4%) and 60 (17.8%) preferred face to face and through secret letter as way of obtaining their test result (Table 3.).
Regarding time preference to have test for HIV/AIDS, 138 (40.8%) and 97 (28.7%) preferred weekend and working time as convenient time respectively. While to history of sexual behavior 74 (21.9%) had history of sexual intercourse. Majority 259 (76.6%) reported that they had never chewed khat and 212 (62.7%) had never drank alcohol (Table 3). Fear of positive test results, the service not being accessible, and fear of stigma by friends were the major constraints for testing for HIV.
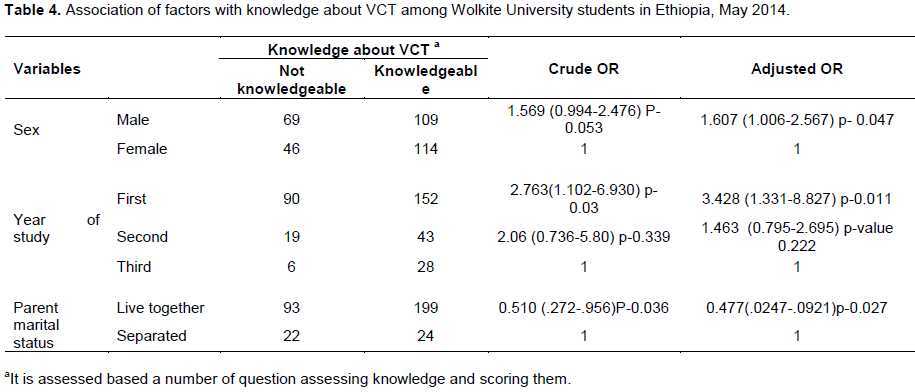
After adjusting for confounders males were two times more odds of being less knowledgeable about VCT (AOR=1.61, P=0.047). As the year of study advance the students are more likely to be knowledgeable. First year students were 3.4 times more likely to be less knowledgeable (AOR=3.428, P=0.011) than third year students. Students whose parents live together have a 53 percent likelihood of being less knowledgeable (AOR=0.48, P=0.027) (Table 4).
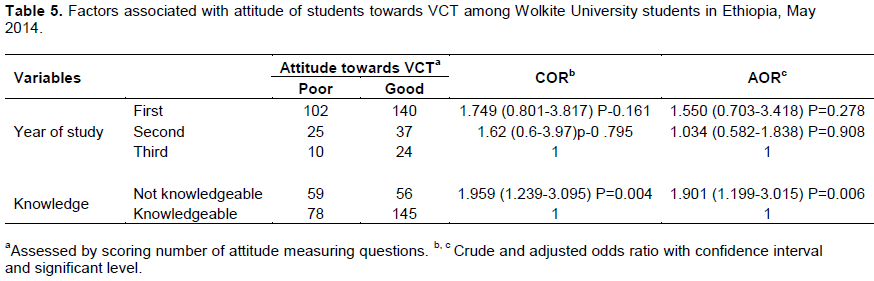
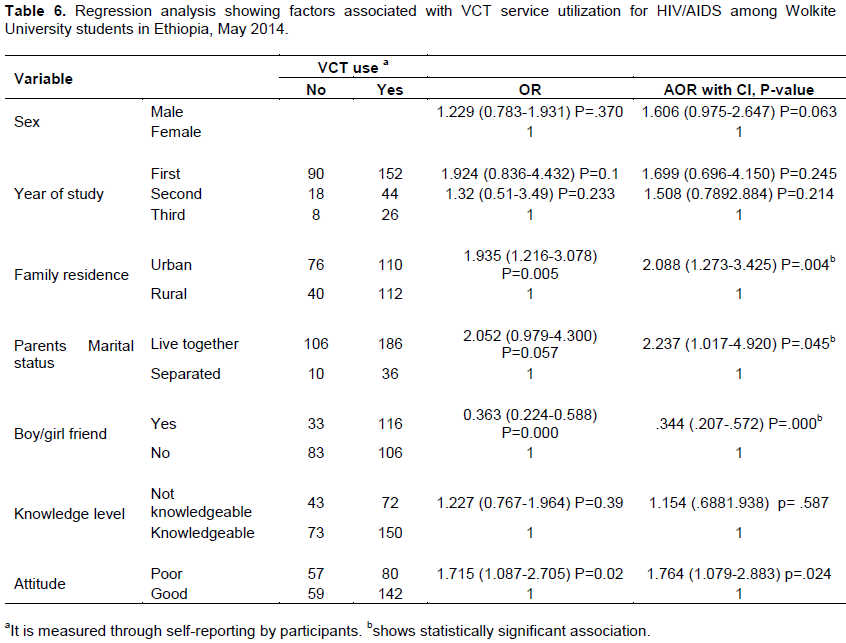
Year of study is associated with attitude towards VCT. Those who are not knowledgeable are almost two times more odds of poor attitude towards VCT than those knowledgeable (AOR=1.901, P=0.006) (Table 5). Family place of residence and parental marital status was found to be significantly associated with having VCT (Table 6).
Students from urban (AOR=2.088, P=0.004) and parents live together (AOR=2.24, p=0.045) are two times not to undergo testing for HIV. Those having boy friend had 64% less odds of not having VCT (AOR=0.344, P=0.000). Having poor attitude is significantly associated with two times higher odds of not undergoing VCT (AOR=1.72, P value=0.024) (Table 6).
Majority about 66% were knowledgeable about VCT for HIV/AIDS based on knowledge score, with 86% had ever heard of VCT for HIV and 86.4% were aware of VCT prevent HIV transmission. Similar study showed 81.6% students were heard of VCT (Girmay et al., 2011). While other studies shows 86% were knowledgeable (Zelalem et al., 2013) and similarly in Kenya (Museve et al., 2013). This discrepancy may relate to the scoring system and the information communication system in the area regarding VCT. Since the campus was young it had no well organized testing and education program for the students. Students were not well aware of the services given like having counseling, partner advising rather percept that VCT is like having blood testing only. Thus this gap should be narrowed through communication.
In this study 87.3% perceived that having VCT is good to prevent HIV/AIDS while more than half (60%) were willing to have VCT. This shows that students had optimistic attitude towards VCT. And more than two third responded they did not stigmatize if their friends test become positive. Similar studies showed 88% (Girmay et al., 2011), 76.9% and 82% (Abiy et al., 2009) were willing to undergo VCT. But these should be seen in consideration of possible social desirability bias. And surprisingly only 40% of students had a good attitude towards VCT while other study reports higher level, 73.3% (Zelalem et al., 2013). This might be sampling composition, information accessibility and the variation while measuring the variable, keeping possibility of higher desirability bias in second or under reporting in the former study.
In this study 65.7% (95% CI: 60.8%-70.6%) of the students reported as they ever had VCT and only 29% had tested in 2012. This low testing rate partially attributed to lack of functioning VCT center in the campus. While study among university students showed 61.8% (95% CI: 56.5%-67.04%) (Zelalem et al., 2013) and 58.5% (95% CI: 55-62%) (Girmay et al., 2011) had ever had VCT. There is no significant difference in proportion of ever tested. This testing rate might be result of country’s extensive work on service provision and increased accessibility to knowledge and services of testing through campaigns and integrated networks (FHAPCO, 2007).
In addition being male (AOR=1.607 (1.006-2.567) and first year (AOR=3.428 (1.33-8.83) were less likely to be less knowledgeable of VCT. Similarly to previous studies (Alemayehu, 2010; Zelalem et al., 2013) females are more knowledgeable. The result is conjunction with the previous results.
Level of education and knowledge about VCT were positively associated with good attitude. As level of year of study in the campus increases their attitude towards HIV test become good. And those who are knowledgeable have good attitude towards test. This emphasizes the effect of knowledge and academic stage on improvement of positive attitude or behavioral change. First year students are less likely to undergo test (P>0.05). As the students stay more they acquire information about the VCT and will have the test.
VCT use was associated with sex, year of study, parental marital status, place of residence and having boy/girlfriend. Those females tend to use VCT more likely. It supported by female are more knowledgeable, thus tend to had VCT more likely than males. While study in Malawi showed no association between sex and knowledge about VCT (Ntata et al., 2008). Students who report of having boy/girlfriend were significantly associated with test. It could be due to the fact students who enter to relationship have better communication and understanding of sexual issues.
Knowledge and attitude towards testing were associated with testing for HIV. Those students with good attitude were 1.76 more odds for not undergoing VCT. This emphasizes that importance of attitude change on the utilization of service. Since perceived benefit and risks will improve utilization, knowledge is also important. And fear of result, in availability of service and stigma are major barriers for not had test for HIV. Other studies supported these (Museve et al., 2013; Zelalem et al., 2013). While previous study (Zelalem et al., 2013) showed urban, male were more likely to use VCT. It might be due to variation in sample composition. But those knowledgeable had less of odds of not having VCT for HIV (Zelalem et al., 2013). In general this study used mean knowledge and attitude score to assess knowledge and attitude might have distorted the final result of the study. The issue of respondents’ social desirability and other bias should be taken in to consideration for the result.
Generally knowledge, attitude and practice of students towards VCT are relatively unsatisfactory. Different information education communication and peer to peer discussion are of great value. Sex, year of study and parent marital status is associated with knowledge about VCT. This will enable to target specific group in case where whole is not feasible. Senior students and those who are knowledgeable are significantly associated with good attitude. Having good attitude is significantly associated with greater use of having test. Students who engage in relationship use significantly more likely to had test.
The authors have not declared any conflict of interests.
REFERENCES
|
Abiy A, Getnet M (2009). Perception of High School Students towards Voluntary HIV Counseling and Testing, using Health Belief Model in Butajira, SNNPR. Ethiop. J. Health Dev. 23(2):149-155.
|
|
|
|
Admassu M, Fitaw Y (2006). Factors affecting acceptance of VCT among different professional and community groups in North and South Gondar Administrative zones, north west Ethiopia. Ethiop. J. Health Dev. 20(1):24-31.
Crossref
|
|
|
|
Alemayehu B (2010). Knowledge, Attitude, and Practice of Voluntary Counseling and Testing for HIV among University Students, Tigray, Northern Ethiopia. Momona Ethiop. J. Sci. 2(1):108-118.
|
|
|
|
Awoke M, Yilma M (2008). Linkage between VCT and reproductive health services (FP, ANC and delivery) in two public facilities of rural Ethiopia. Ethiop. J. Health Dev. 22(2):159-163.
|
|
|
|
EDHS (Ethiopian Demographic Health Survey) (2011). Ethiopia Demographic and Health Survey Ethiopia Demographic and Health Survey. I. International. Addis Ababa, Ethiopia, Central Statistical Agency. pp. 253-256.
|
|
|
|
FHAPCO (Federal HIV prevention and control Office) (2007). Guidelines for HIV Counseling and Testing in Ethiopia Federal HIV/AIDS Prevention and Control Office. Introduction. Addis Ababa, Federal Ministry of Health: 2-4.
|
|
|
|
Girmay T, Melkie E, Solomon M (2011). Assessment of voluntary counseling and testing service utilization and associated factors among Debre Markos University Students, North West Ethiopia: a cross-sectional survey. BMC Public Health 13(243):1-12.
|
|
|
|
UNAIDS (Joint United Nation program on HIV/AIDS) (2012). UNAIDS Report on Global AIDS Epidemic. Global Report on global AIDS epidemic, UNAIDS: 8-12.
|
|
|
|
Leta TH, Sandøy IF, Fylkesnes K (2012). Factors affecting voluntary HIV counseling and testing among men in Ethiopia: a cross sectional survey. BMC Public Health 12:438-442.
Crossref
|
|
|
|
Meda L (2013). Assessing factors influencing university students to uptake voluntary counselling and testing (VCT) of human immune deficiency virus/acquired immune deficiency syndrome (HIV/AIDS). J. AIDS HIV Res. 5(6):173-180.
|
|
|
|
Museve J, Gongera E, Constantine L (2013). An Analysis of Uptake in HIV Voluntary Counselling and Testing Services: Case of Mount Kenya University Students, Kenya. Public Policy Admin. Res. 3(4):16-20.
|
|
|
|
Ntata P, Muula A, Siziya S, Kayambazinthu E (2008). Gender differences in university students' HIV/AIDS-related knowledge and sexual behaviours in Malawi: a pilot study. J. Soc. Aspects HIV/AIDS 5:201-206.
|
|
|
|
Tsehaye T, Bikes D, Mengesha A, Bayeh A (2010). Assessment of factors associated with voluntary counseling and testing uptake among students in Bahir Dar University:A case control study. Ethiop. J. Health Dev. 17-23.
|
|
|
|
WHO (World Health Organization) (2003). Increasing access to HIV testing and counseling WHO. Geneva, Switzerland, WHO 19-21.
|
|
|
|
Zelalem A, Yalew A, Shiferaw Y, Alemu A, Birhan W, Mathewose B, Tachebele B (2013). Knowledge, attitude and practice towards voluntary counseling and testing among university students in North West Ethiopia: a cross sectional study. BMC Public Health 13(714):2-7.
|