ABSTRACT
Adherence to antiretroviral therapy is of critical importance because even minor deviations from the prescribed regimen can result in viral resistance. Multiple factors influence adherence among people living with human immune virus. But at present little is known about the patient’s experience and adherence when taking such complex regimens. The major aim of the study was to assess factors associated with antiretroviral treatment adherence among people living with human immune virus A facility based cross-sectional study design was used, with systematic sampling technique on 300 adult patients on antiretroviral therapy. Factors associated with adherence to antiretroviral drugs were analyzed with bivariate and multivariate logistic regression. A total of 300 patients on antiretroviral therapy involved in this research and despite requirement of complete or near complete adherence to antiretroviral therapy only 205(68.3%) were found to be adherent. The bivariate and multivariate logistic regression showed that factors like mild depression (AOR=3.24) 95% CI(2.04-8.67), moderate depression (AOR=3.06) 95%CI(1.61-5.67), alcohol abuse (COR=2.562) p=0.049, current khat chewing (COR=2.85) p=0.025, disclosure status (COR=0.426) p=0.004, presence of opportunistic infection (AOR=5.44) 95%CI(1.833-16.10), and presence of comorbid disease (COR=4.256) p=0.002 showed association to adherence to antiretroviral therapy. Generally about three out ten patients on antiretroviral therapy were found to be non-adherent to antiretroviral regimen in Bale zone. Depression and the presence of opportunistic infection are adversely linked to adherence status of these patients.
Key words: Adherence, highly active antiretroviral therapy (HAART), ART Clinic, Bale.
One point eight million people died of Human Immuno Virus (HIV) in the year 2010, of whom those living in sub Saharan Africa were 1.2 million. Major improvement has been made in delivering lifesaving treatment for people living with HIV. There are now 6.6 million people globally on the treatment of anti-retroviral therapy (ART), of which more than 5 million are in Africa (UNAIDS, 2010).
The adjusted HIV prevalence for Ethiopia in 2005 was 3.5% (urban 10.5% and rural 1.9%). The situation of HIV epidemic in Amhara, Oromia, Addis Ababa, and SNNPR is worse than other regions. Together these regions accounted for 86.6% of all PLWHA in Ethiopia. The HIV epidemic continues to pose a threat to the development of Ethiopia where 1.3 million people are living with the virus, 744,100 are orphaned due to Acquired Immune Deficiency Syndrome (AIDS). AIDS accounted for an estimated 34% of all young adult deaths (15-49 years) in Ethiopia and 66.3% of all young adult deaths (15-49 years) in urban Ethiopia (EDHS, 2005; MOH, 2008).
Adherence to antiretroviral therapy (ART) is of critical importance because even minor deviations from the prescribed regimen can result in viral resistance (APA, 2000; Bangsberg et al., 2000). Studies of ART continue to indicate that a near-perfect adherence is required to adequately repress viral replication (Demasi et al., 2001; Gibb et al., 2003).
Adherence can be measured in several ways such as counting prescriptions filled (pill counting), care givers’ reports, and drug-blood level monitoring and self-report by patients. Multiple factors influence adherence among patients with HIV/AIDS. Such factors include patients’ age, regimen complexity, drug side-effects, advanced HIV disease and patients’ mental health (Donenberg and Pao, 2005). Other factors include unfamiliarity with the implications of having a chronic, potentially deadly disease, the complex impact of ART on interpersonal relationships, depression and hopelessness, lack of accurate information, and issues related to local cultural frameworks (e.g. illness ideology) (Murray et al., 2009).
As the world gears toward increasing access to antiretroviral treatment in the developing world it is critical to understand factors (motivators and barriers) that influence adherence to antiretroviral and apply the lessons learnt in improving existing and new programs. Available research in Ethiopia has shown that our understanding of factors associated with ART adherence is limited, and related literature in the study area is remarkably scarce. Understanding the predictors of adherence in the local context is a forefront agenda in Ethiopia, where little is known and scaling up of ART program is in progress.
Study area and period
The research was conducted in all hospitals and selected health centers in Bale Zone. Bale Zone is one of the administrative zones found in Oromia regional state. Based on the 2007 Census conducted by the CSA, this Zone has a total population of 1,402,492, an increase of 15.16% over the 1994 census, of whom 713,517 are men and 688,975 women; with an area of 43,690.56 km
2, Bale has a population density of 32.10/km
2. While 166,758 or 26.20% are urban inhabitants, a further 44,610 or 3.18% are pastoralists. A total of 297,081 households were counted in this Zone, which results in an average of 4.72 persons to a household, and 287,188 housing units. Robe, the capital of the zone is found 430 km south East of Addis Ababa. Bale is bordered on the south by the
Ganale Dorya River which separates it from
Guji, on the west by the
West Arsi Zone, on the north by
Arsi, on the northeast by the
Shebelle River which separates it from
East Hararghe and West
Hararghe, and on the east by the
Somali Region. The study was conducted starting from January 2015 to February 2015.
Study design
Facility based cross sectional study was conducted at ART clinics in hospitals and health centers in Bale Zone. Patients’ cards were reviewed and the patients were interviewed during data collection.
Population
Source population
All patients on HAART at ART clinics in hospitals and health centers in Bale Zone.
Study population
A sample of patients on HAART at ART clinics in all four hospitals and health centers in Bale zone at the period of data collection.
Inclusion and exclusion criteria
Inclusion criteria
All adult patients on ART. Patients who attended ART are at least for 6 months.
Exclusion criteria
Patients who are critically ill or unable to communicate due to cognitive impairment.
Sampling and sample size determination
Sample size determination
The required sample size was determined by considering the following assumptions for interview questionnaires: Since similar literatures done in the same or similar place were not available for using proportion. The percentage of adherent patients at Yirgalem hospital, that is, 74.2% (Amberbir et al., 2008). So the proportion = 74.2%. Confidence interval = 95%; Margin of error = 5%, and Non-response rate = 10%
The formula for calculating the sample size is:
Since total population of patients on ART in hospitals and health centers of Bale zone are 3816, nf = n/1+n/N = 294.16/1+2944.16/ 3816 = 273
Finally 10% non-response rate was added which resulted in final sample size of 300. The number of samples that were withdrawn from respective hospitals was determined proportionally.
Data collection procedures
Structured questionnaires and interview was used in the study. In addition to the questionnaire, data collection format was developed by the principal investigator to collect data from patient card in respective study participants. The questionnaire was developed first in English and translated to Afan Oromo with the help of language expert. The questionnaire contains both close ended and open ended questions. It had parts that assess socio demographic, social drug use, adherence and Patient health questionnaire 9 (PHQ9). PHQ9 was used to assess depression. Four items Validated Morisky Scale was used to judge the adherence status of the study participants. The local languages version questionnaire was back translated to English to proof consistency. The data collection was carried out by three nurses and two health officers at four hospitals and one health center. They were trained for one day by the principal investigators prior to data collection.
Data quality assurance
The questionnaire was pre-tested with 10 patients of Dodola hospital before the actual data collection. Training was given for data collectors and questionnaire was prepared by English and local languages (Afan Oromo and Amharic languages). Data collectors were instructed to check the completeness of each questionnaire at the end of each interview. The principal investigators rechecked completeness of the questionnaire and prepared the questionnaire for data entry.
Methods of data analysis
The data were cleaned, coded, entered to Epi info 7 before analysis. The data were exported to SPSS version 20 and analyzed. Factors associated with adherence to ART were analyzed with bivariate and multivariate logistic regression. All factors with a p-value <0.25 in the bivariate logistic regression analysis were further entered into the multivariate model to control confounding effects. P<0.05 was used as statistically significant.
Ethical considerations
The study was conducted after approval is secured from Madda Walabu University Research and technology transfer directorate bureau. This bureau also wrote formal letter of permission to the four hospitals to permit access of data and cooperate. Finally oral consent was obtained from each study participants before making interview and confidentiality was secured. In addition all the responses were kept confidential and anonymous and participants were be able withdraw from the study at any time during interview.
Socio-demographic characteristics
Participants
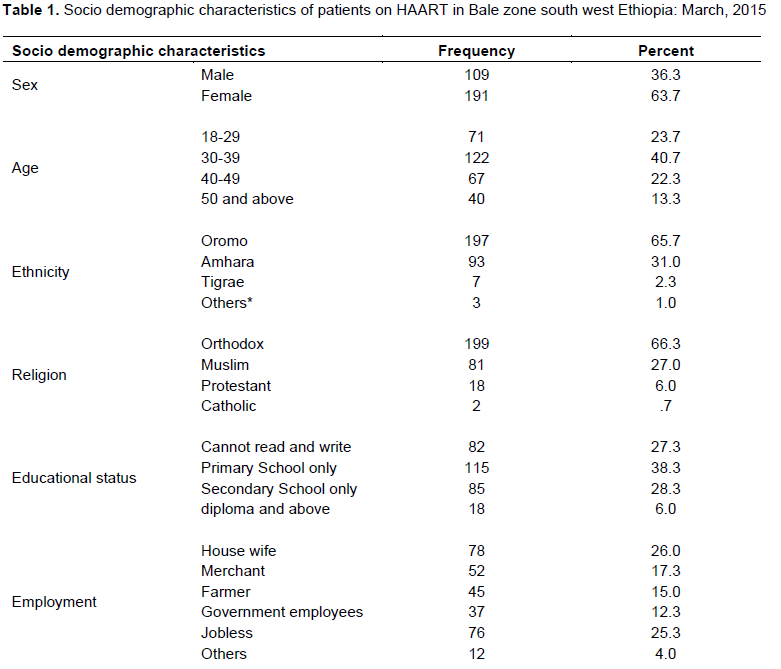
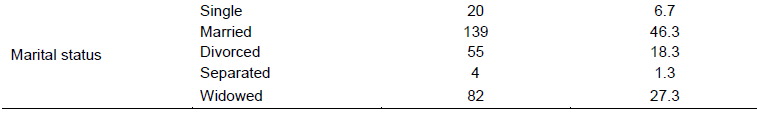
A total of 300 eligible clients were included in the chronic follow up unit during the study period, with the response rate of 100%. The study consisted of 191(63.7%) females. By ethnic classification, 197(65.7%) respondents were Oromos, 93(31.0%) were Amharas, 7(2.3%) were Tigrians, 1(0.3%) was Somali and the remaining 0.7% are others by ethnicity. Majority of the respondents, 199(66.3%) were orthodox Christianity followers and 81(27.0%) were Muslims. Regarding the residence place of the study participants, 122(40.7%) are residents of Robe town, whereas 72(24%) are residents of Goba town, 72(14%) are residents of Ginnir town. Regarding educational status of the study participants, 115(38.3%) have attended only primary school, 85(28.3%) have attended only secondary school, 82(27.3%) cannot read and write, whereas 18(6.0%) of the study participants have at least college diploma. The job category of the study participants show that 78(26.0%) were house wives, 76(25.3%) were jobless, 52(17.3%) were merchants, 37(12.3%) were government employees, 12(4.0%) were engaged in other jobs. The marital status analyses showed that 139(46.3%) were married, 55(18.3%) were divorced, 4(1.3%) were separated, 82(27.3%) were widowed, and 20(6.7%) were singles (Table 1).
Psychosocial description of the study participants
A total of 77 (25.7%) of the study participants were found to be depressed at different magnitude; 48(16.0%) were found to be mildly depressed, 24(8.0%) were moderately depressed, 5(1.7%) were moderate severely depressed. Regarding stigma status of the study participants 168 (56.0%) were moderately stigmatized, 124(41.3%) were mildly stigmatized whereas 8(2.7%) were severely. The disclosure status analyses showed that, 241(80.3%) of the study participants have disclosed their HIV infection status at least to their closest person, whereas 59(19.7%) of the study participants have not disclosed their HIV infection status even to their closest person. Regarding substance abuse, 19(6.3%) reported that they were abusers of alcohol during the data collection, 281(93.7%) reported that they were not abusers of alcohol (Table 2).
Factors associated with adherence
Despite requirement of complete or near complete adherence to HAART only 205(68.3%) were found to be adherent. The bivariate and multivariate logistic regression showed that factors like mild depression (AOR=3.24) 95% CI(2.04-8.67), moderate depression (AOR=3.06)95%CI(1.61-5.67), alcohol abuse (COR=2.562) p=0.049, current khat (fresh leaf of Catha edulis containing cathinone, amphetamine like compound) chewing (COR=2.85)p=0.025, disclosure status (COR=0.426) p=0.004, presence of opportunistic infection (AOR=5.44) 95%CI(1.833-16.10), presence of comorbid disease(COR=4.256)p=0.002showed association to adherence to HAART. Whereas factors like age, sex, educational status, employment status, marital status, stigma, cigarette smoking, social support and duration on the HAART failed to show significant association with adherence to HAART.
Literatures state that the non-adherence to HAART ranges from 10 to 92% (Bartelett, 2002); in this study the prevalence of adherence was found to be 68.3%. It agrees with findings of Bartelett et al. (2002). Our finding showed worse adherence status compared to findings from Atlanta and Spain where the adherence where adherence was found to be 80 and 90%, respectively. But the level of adherence to HAART in Bale Zone was found to be slightly better than the prevalence of adherence in Cape Town, South Africa where the prevalence of adherence was found to be 63%. Coming to findings from different parts of Ethiopia the study conducted in Jimma University specialized hospital showed self-reported adherence to be 94.3% which is far better than our finding but we doubt about the tool they have utilized to assess adherence as they have used self-reported adherence measuring style which is more prone to recall bias than Validated Morisky Scale. Prevalence of adherence to HAART in Yirgalem Hospital was found to be 74.2% which is not by far better than our finding.
Regarding the factors associated with adherence to HAART, studies in Addis Ababa showed that factors like travels, depression and drug adverse effects showed association to non-adherence to HAART. In our study,
depression and presence of opportunistic infection is linked to non-adherence, but drug adverse effect showed no significant association with adherence in both bivariate and multivariate logistic regression, this may be because of overlapping of symptoms of HIV/AIDS and adverse effects of HAART which will make identification of adverse effects more difficult in health facilities with relatively low infrastructure and experts like Bale Zone. As only two cases of adverse effect were reported out of total 300 respondents, this may be due to underreporting of adverse effects. Studies from India have shown that oxidative stress is linked to Non-Neuclotidal reverse transcriptase Inhibitors (NNRTI) and Neuclotidal reverse transcriptase Inhibitors (NRTI) use (Sharma, 2014). Despite high utilization of NNRTIs and NRTIs in Ethiopia, our study has not revealed much adverse effects; may be due to the above mentioned reason.
The study in Yirgalem showed that the prevalence of all types of depression among patients on HAART to be 98.28% which is far more our finding which is 25.7%. This may be due to failure of utilization of validated tool to measure depression; the study assessed depression by asking the respondents whether they have ever witnessed depression. But our finding is almost similar with study taken by Jimma university specialized hospital which reported the prevalence of depression among patients on HAART to be 28.65%. Study in Ahmadu Bello University Teaching Hospital, Zaria, Nigeria also revealed depression 21.3% of patients on HAART (Olisah et al., 2010).The finding of this study also agrees with our finding.
Factors like gender, race, age, ethnicity and literacy have showed inconsistent results in predicting adherence according to Ammassari et al. (2002) study; this is similar with our finding which showed no significant association between adherence and factors like sex, age, ethnic group, educational status and marital status.
The binary logistic regression depicted that alcohol abuse, current chat chewing status are adversely liked with adherence to HAART, this finding is partly supported by the findings of Stephen Magura which linked alcohol abuse to adherence to HAART adversely (Magura et al., 2011). But these factors failed to show significant association in multivariate logistic regression in our case, this may be due to lower level of substance abuse in Bale Zone compared to Bronix, New york City
Generally in this study we have tried to assess the variables with standardized tools like validated Morisky scale for adherence, PHQ 9 for depression and Stigma scale for stigma determination this could be taken as main strength of the study. But intermittent service from health centers and stopping of giving ART service by some health centers forced as to get data from sites of referral of the patients. Some of the variables like adverse effects are difficult to measure because of the overlapping of the symptoms of HIV/AIDS and adverse effect of HAART. It also requires prolonged follow up and expert utilization which is not accomplished by our study.
Generally about three out ten patients on HAART were found to non-adherent to HAART in Bale zone. Depression was detected in about one patient in every for patients on HAART. Depression and the presence of opportunistic infection are adversely linked to adherence status of these patients. Other factors like substance use and disclosure status showed association in binary logistic regression but failed to show significant association in multivariate logistic regression. Factors like age, sex, educational status, occupation, marital status, duration on HAART, recent CD4 count and presence of adverse effect failed show any significant association with adherence to HAART.
All the authors declare there is no conflict of interest. All the authors participated and contributed equally.
REFERENCES
|
Ammassari A, Trotta MP, Murri R, Castelli F, Narciso P, Noto P, Vecchiet J, D'Arminio Monforte A, Wu AW, Antinori A (2002). Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. J. Acquir. Immune Defic. Syndr. 31 Suppl 3:S123-S127.
Crossref
|
|
|
|
Amberbir A, Woldemichael K, Getachew S, Girma B, Deribe K (2008). Predictors of adherence to antiretroviral therapy among HIV-infected persons: a prospective study in Southwest Ethiopia. BMC Public Health 8:265.
Crossref
|
|
|
|
|
APA (2000). Practice guideline for the treatment of patients with HIV/AIDS. Am. J. Psychiatry 157:11.
|
|
|
|
|
Bangsberg DR, Hecht FM, Charlebois ED, Zolopa AR, Holodniy M, Sheiner L, Bamberger JD, Chesney MA, Moss A (2000). Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. AIDS 14(4):357-66.
Crossref
|
|
|
|
|
Bartelett JA (2002). Adressing the challenges of adherence. J. Acquir. Immune Defic. Syndr. 29 Suppl 1:S2-10.
Crossref
|
|
|
|
|
DeMasi RA, Graham NM, Tolson JM, Pham SV, Capuano GA, Fisher RL, Shaefer MS, Pakes GE, Sawyerr GA, Eron JJ Jr (2001). Correlation between self-reported adherence to highly active antiretroviral therapy and virologic outcome. Adv. Ther. 18(4):163-73.
Crossref
|
|
|
|
|
Donenberg GR, Pao M (2005). Youths and HIV/AIDS: Psychiatry's role in a changing epidemic. J. Am. Acad. Child Adolesc. Psychiatry 44(8):728-47.
Crossref
|
|
|
|
|
EDHS (2005). Ethiopia Demographic and Health Survey reports.
|
|
|
|
|
Gibb DM, Goodall RL, Giacomet V, McGee L, Compagnucci A, Lyall H (2003). Paediatric European Network for treatment of AIDS Steering Committee. Adherence to prescribed antiretroviral therapy in HIV infected children in the PENTA 5 trial. Pediatr. Infect. Dis. 22:56-62.
Crossref
|
|
|
|
|
Magura S, Rosenblum A, Fong C (2011). Factors associated with medication adherence among psychiatric outpatients at substance abuse risk. Open Addict. J. 4:58-64.
Crossref
|
|
|
|
|
Ministry of Health (MOH) (2008). Federal Democratic Republic of Ethiopia, Ministry of Health national HIV/AIDS prevention and control. AIDS in Ethiopia. pp. 46-49.
|
|
|
|
|
Murray LK, Semrau K, McCurley E, Thea DM, Scott N, Mwiya M, Kankasa C, Bass J, Bolton P (2009). Barriers to acceptance and adherence to Antiretroviral therapy in urban Zambian women: a qualitative study. AIDS Care 21(1):78-86.
Crossref
|
|
|
|
|
Olisah VO, Baiyewu O, Sheikh TL (2010). Adherence to highly active antiretroviral therapy in depressed patients with HIV/AIDS attending a Nigerian university teaching hospital clinic. Afr. J. Psychiatry 13:275-279.
Crossref
|
|
|
|
|
Sharma B (2014). Oxidative Stress in HIV Patients Receiving Antiretroviral Therapy. Curr. HIV Res. 12:13-21.
Crossref
|
|
|
|
|
UNAIDS (2010). United Nations program on HIV and AIDS Global report.
|
|