ABSTRACT
Disclosure of HIV positive status to sexual partners, friends or relatives is crucial for HIV prevention and care implementation strategies. Hence, it is important to explore factors determining individuals to disclose their HIV positive status in order to achieve a goal of zero new HIV infection. Facility based mixed cross-sectional study was conducted from July to August, 2013 among 361 HIV positive adults attending Axum Health Facilities. They were selected through systematic random sampling. Data were collected by trained counselors and ART nurses and then entered into SPSS version 20 databases. Bivariate and multivariable logistic regression models were used to identify predictors of HIV positive status disclosure at 95% confidence intervals and p-value of less than 0.05. Among 361 respondents, 289 disclosed their HIV status to someone and 151(41.8%) to intimate partners. In the multivariate logistic regression analysis, variables significantly associated at p-value <0.05 were married; knowing partner’s HIV status and membership in an HIV-Support Group were positive predictors of disclosure. These findings were supported by qualitative study in which fear of discrimination, fear of breaking confidentiality and fear of families make them to conceal their status. The rate of HIV positive status disclosure among HIV positive adults has remained low. Marital status of respondents, knowledge of partners’ HIV status and being member in Anti- HIV/AIDS Association were identified as predictors of HIV positive status disclosure. Addressing the issues of disclosure was recommended to encourage free disclosure and coping with negative reactions, which is a crucial way for adherence to treatment.
Key words: Adult, Axum health facilities, Ethiopia, HIV positive disclosure.
Disclosing one’s HIV status to a sexual partner means talking honestly about sexual orientation, possible drug use and results of tests. These are often taboo subjects that are difficult to talk about openly and honestly in most societies (Mbonu et al., 2011).
Disclosure is something that every person living with HIV experiences and struggles with. The process is complex and fraught with mixed emotions and the outcomes can be unpredictable and difficult to handle. Despite the difficulty disclosure might pose, non-disclosure has detrimental impacts on the person living with HIV and is associated with personal distress, loneliness and social isolation (Rapid Response Service, 2013).
Self-disclosure of sensitive information is generally thought to have beneficial effects on an individual's health, by lowering stress, and leading to better psychological health. Disclosure may motivate sexual partners to seek testing, change behavior and ultimately decrease transmission of HIV. The exchange of information about one's HIV status with a prospective partner is associated with safer sexual practices (Legasion, 2012). Failure to disclose HIV positive status could lead to unsafe sexual practice which in turn increases the risk of infecting a sexual partner, and may lead to couples re-infection with new strains and transmission to child. This may result in lack of getting access to care and support, loss of opportunities to prevent new infections (Kassaye et al., 2005).
Disclosure offers a number of important benefits to the infected individual and to the general public. Disclosure of HIV test results to sexual partners leads to less anxiety and increased social support among many women. Disclosure is also crucial to the individual’s health in today’s context of accelerated highly active anti-retroviral treatment use, to gain social and emotional support, to ensure proper adherence to treatment and better therapeutic efficacy (WHO, 2012).
The outcomes of HIV disclosure can be stressful but also rewarding. There is not a ‘rule of thumb’ for when outcomes or consequences might be positive or negative. But overall, evidence suggests positive reactions to disclosure outweigh negative ones. For instant studies in Hawasa reveals that following disclosure, partner reaction was positive for 40.7% and for 33.3% of the women with regular partner and non-regular partner respectively. It was negative for 59.3% of the women with regular partner and for 66.7% of the women with non-regular partner (Gari et al., 2010).
In most studies from both developing and developed country settings, HIV status disclosure to sexual partners was associated with positive outcomes including increased social support, acceptance, kindness, decreased anxiety and depression, and strengthening of relationships. While fear of negative outcomes was a major reported barrier to HIV status disclosure, most individuals who chose to disclose reported experiencing positive social outcomes as a result of their disclosure including support and understanding from partners (WHO document summary, 2012).
Therefore, this study aims to explore determinants of HIV positive status disclosure and associated factors among HIV positive adults which will help to examine relevant information that decision makers and managers can use to address the problem and in turn will contribute a lot toward achieving a goal “zero new infection”.
Though information pertaining to HIV positive status disclosure is needed, there is little knowledge is known in Ethiopia and the study conducted in the study area lacks qualitative information from disclosed & non disclosed adults (Haileselasie et al., 2015).
Therefore, this study aims to explore determinants of HIV positive status disclosure and associated factors among HIV positive adults which will help to examine relevant information that decision makers and managers can use to address the problem and in turn will contribute a lot toward achieving a goal “zero new infection”.
Study setting
Institution based mixed cross-sectional study was carried out in Axum Health Facilities. Axum is located in the Central zone of Tigray, Northern part of Ethiopia. It is located 235 km away from Mekelle, the capital of Tigray and 1030 km north of Addis Ababa, the Federal Capital of Ethiopia. Aksum is situated in the highlands of Northern Ethiopia; it symbolizes the wealth and importance of the civilization of the ancient Aksumite kingdom, which lasted from the 1st to the 8th centuries AD. It was the original capital of the kingdom of Axum which dates back some 2,000 years to when it was the hub of the Axumite Empire. In the town there are one General Hospital (Axum St. Marry Hospital) and two Health Centers (Millennium and Axum Health Centers). The hospital provides medical, surgical, gynecological obstetrics and pediatrics care. Currently above 3558 people living with HIV/AIDS (PHAs) are routinely utilizing the hospital services with 2560 Pre Art and 998 ART. The Axum Health Center has commenced ART service in 2007 and provides a service for 156 pre ART and 142 ART clients (Axum woreda health office, 2012).
Sample size and sampling techniques
Sample size was determined by using a single population proportion formula which considers the proportion of HIV positive status result disclosure to sexual partner is 69% (Deribe, 2005), with marginal error of 5% at 95% confidence interval. Then by adding 10% non- response rate, the final sample size was calculated to be 362. A systematic random sampling procedure was used to select eligible participants from each ART unit. Every “5th” HIV positive adults who came for the ART follow-up was selected. Hence, every 5th individuals who came to receive pre ART or ART service was selected for the interview until the required sample size was obtained.
Qualitative in-depth interviews were conducted among 12 HIV positive individually to explore personal live experiences on HIV positive status disclosure.
Operational definitions
HIV positive status disclosure: The act of informing HIV positive status to any one (sexual partner, parents, families or friends). Positive outcome of disclosure: are outcomes which facilitate or encourage an individual to disclose HIV positive status.Negative outcomes of disclosure: are those outcomes (such as stigma and rejection, divorce, economic dependence) which lead an individual to conceal HIV positive status.
Data collection and analysis
Data were collected by structured and pre-tested interviewer administered questionnaire which was adopted after reviewing literature relevant to the objective of the research. The questionnaire was prepared in English first, translated into the local language (Tigregna) and back to English to assure consistency. The data were collected by trained counselor and ART nurses.
Data were entered into SPSS version 20 statistical software for analysis. Descriptive statistics were used to determine the magnitude of HIV positive status disclosure and reasons for disclosing HIV positive status. Odds ratios at 95% confidence intervals and P- value 0.05 were used to determine the significance and degree of association between dependent and independent variables. Multiple logistic regression analysis was carried out to see independent effect of each variable on the outcome.
Qualitative study
Participants were explained about the overall objective of the study prior to interview. Interviewees who participated in the qualitative component of the study were asked a series of broad, open-ended questions related to their experiences of disclosure by unstructured interviewing techniques such as probing. The interviewer encouraged respondents to explore what the experience was like for them. For example, particular attention was paid to discussions of how they told their partners of their positive status, what their concerns were, exactly how the partner responded, and how their relationship changed following disclosure.
In-depth interviews were audio recorded and then transcribed and then translated from Tigregna to English by verbatim. The transcript information was coded by investigators using thematic codes consistent with the study objective. Specific codes related to the object of interest were then selected and to find illustrative quotes to triangulate on specific findings from the quantitative findings.
Data quality assurance
The questionnaire was pre-tested in 20 HIV positive adults at Adwa Hospital two weeks before the actual data collection. Training was given for data collectors, supervisors and for three consecutive days. The training mainly dealt with the purpose of the study, handling ethical issues during data collection, and the method of data collection using the structured questionnaire. Data collectors were instructed to check the completeness of each questionnaire at the end of each interview. Supervisors rechecked for completeness of the questionnaire on daily basis of submission. Qualitative interviews were conducted in comfortable and sound proof place which sound records make clear. Deep insight of live experiences was probed using unstructured questionnaire.
Ethical consideration
Ethical clearance was obtained from Aksum University, College of Medicine and Health Science Institutional Ethical Review Committee. Official letter of support was also written to Tigray Region Health Bureau then letter of co-operation was obtained from the bureau to respected hospital and woreda health offices.
Verbal informed consent was obtained from each participant after by explaining the purpose of the study and reading out the consent form before the interview. All information provided will be kept confidential and there was no link to their identity as no names appeared on any form to assure the confidentiality of the participants.
A total of 361 HIV positive adults were interviewed and the response rate was 99.7%. More than half (57%) of the respondents were females. A majority of the respondents were Orthodox Christian 316 (87.5%) and great majority 352 (97.5%) of them were Tigrian in Ethnicity. The age of respondents ranged from 19 – 67 years with mean (SD) age of 36 (± 8.97) years. Three hundred twenty eight (90.9%) were residences of urban area and 177(49%) of them were married. (Table 1)
HIV positive status disclosure
Among the 361 participants, 289 (80.1%) of them disclosed their HIV positive status to somebody; while 151(41.8%) disclosed to their sexual partner and 127 (35.2%) disclosed to their parents. Among HIV positive adults who have a sexual partner, 169 (90.8%) disclosed their HIV positive status to their sexual partner (Figure 1).
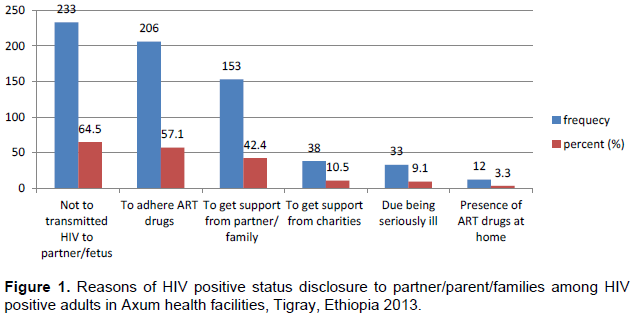
Out of 289 respondents who disclosed their HIV positive status; 202 (67%) disclosed within one month, 39 (13.4%) disclosed between 1 and 6 months and 48 (16.6%) disclosed after 6 months of being notified their HIV positive result. The common reasons to disclose their HIV positive status was not to transmit HIV to partners (233), to make adherence of ART therapy (206) and to get psychological and financial support from partner or families (153).
This result was supported by qualitative interviewed respondents developed into two themes. The in-depth interview was conducted among 12 HIV positive individuals who were disclosed. The identified themes were developed under which others are included:
Medical illness related
The qualitative interviews shed light on these experiences: Most respondents were shy and anxious after the diagnosis of their illness. Several said they were constantly depressed that people would find out and in some instances this led to self-imposed isolation.
A 32 years old male who disclosed his status claimed: ‘’ I was diagnosed first with HIV in the ward but was treated for Tuberculosis. I was shy and feared my wife would blame and leave me alone. But she gave me support and care and lastly was willing to be tested. The result was similar. We are now living together… ‘’
Another 35 years old male expressed: “I have had cough and fever; I lost my energy and weight. My mother took me to hospital and the nurse asked me to do HIV test and then the result was positive. After getting treatment I then told to my partner that I am HIV positive and she also tested and found that she is HIV positive. She decided to stay away and left without making any divorce process…’
Pregnancy condition
Some women found out they were HIV positive during ante natal programme.
A 34 years old female stated “I was pregnant and came to the hospital for ANC follow up. The nurse asked me to do HIV test; the result was positive. I did not reveal my result to my husband because he might get annoyed and beat me. He can divorce me while I am pregnant, leaving all the responsibilities for me.”
Reasons for not disclosing their HIV positive status
Reasons for non-disclosure among those respondents who did not disclose their HIV positive results to their partner/parents/family (n = 72) were "fear of stigma and discrimination (94.4%), fear of breaching confidentiality (61.1%), being shy of families (45.8%) (Figure 2).
This finding was supported by qualitative findings on the reasons that make them not to disclose their HIV positive status, which included fear of partner’s negative reaction and other consequences.
A 26 year young female says, ‘’ I was not expecting positive result and confused when the nurse told me. The first thing that came to my mind was anxiety and humiliation, what will be my husband reaction if I disclose my result? So I prefer to conceal my result for long time…….’’
Similarly a 20 years lady claimed, “I did not disclose my
HIV status to my husband and families because I’m afraid he will beat and divorce me, even my families will discriminate and reject me .I am economically dependent on my husband. So if I disclose my HIV positive result my life will be complicated. … ‘’
Outcomes of HIV positive status disclosure
Following disclosure of HIV positive result, partner,family, or parent reaction was positive for 270/361 (74.7%) where as it was negative reaction for 19 (5.3%). Of 459 individuals who anticipated supportive outcomes, 96.3% (442/ 459) received support and reassurance from their partner after disclosure. However there was paradox response between anticipated and actual outcomes of disclosure. Of 127 respondents who anticipated a negative reaction from their partners, only 17 (13.4%) faced negative reaction of disclosure but the rest (86.6%) received positive reaction such as support and understanding from their partner (Table 2).
Factors associated with HIV positive status disclosure
On bivariate analysis marital status of respondents, type of sexual partner, ART started, educational status of sexual partner, knowledge of partner’s HIV status, sexual partner’s HIV status, discussion about HIV/AIDS prior test, being membership in Anti- HIV Association and use of condom were significantly associated with HIV positive status disclosure. After adjusting variables in the multivariate logistic regression analysis variables significant at p-value < 0.05 were being married, knowing partner’s HIV status and membership in an HIV Support Group.
Unmarried respondents were 3.7 times more likely to disclose their HIV positive status compared to the married (AOR = 3.70; 95% CI; 1.21 – 11.39). Respondents who knew their sexual partner’s HIV status were 3.4 times more likely to disclose their HIV positive status as compared to those who did not know their partner's HIV status (AOR= 3.43; 95% CI: 1.02– 11.54). Participants who were members in Anti- AIDS association were 4.8 times more likely to disclose their HIV positive result compared to those not in the Anti- AIDS Association (AOR = 4.81; 95% CI, 1.01 - 23.05) (Table 3).
HIV positive result disclosure also prevents HIV infection of the sexual partner with a discordant sero-status. For instance, the sexual partners of 30 (16.1%) of the respondents in this study were HIV negative.
The rate of HIV positive status disclosure to at least one person was 80.1%. The finding is lower than that found in the study done in Hawasa Referral Hospital, Ethiopia, which was 92.2% (Gari et al., 2010); in Jimma University Referral Hospital, Ethiopia, it was 94.5% (Deribe et al.,, 2008) and in Kemissie District, north east Ethiopia, it was 93.1% (Seid et al., 2012). The reason could be the study subjects from Jimma and Hawasa University Hospitals might get adequate HIV related information more easily than those in Axum Health Facilities as they are teaching hospitals which are equipped with skilled man power. Besides, it might be due to socio - demographic difference of the study subjects.
On other hand, the rate of HIV positive status disclosure in this study was higher than that reported in Mettu and Gore towns (69%) (Kassaye et al., 2005). The possible explanation for this could be due to the reason that ART service provision was not fully implemented national wide and the patients were highly stigmatized and discriminated due to the disease. So they prefer to conceal their status. Seventy two (19.9%) of the respondents did not disclose their HIV positive status to anyone. Some of the reasons for non - disclosure based on this study were fear of stigma and rejection, fear of breach of confidentiality, shyness, and fear of divorce. These results were consistent with studies carried out elsewhere in Ethiopia (Erku et al., 2012; Gari et al., 2010; Seid et al., 2012; Erku et al., 2012). These reasons were also similar to studies done in different developing countries like Uganda, South Africa, Tanzania and Djibouti (Antelman et al., 2001; Kadowa and Nuwaha, 2009; Makin et al., 2008; Kajura, 2010).
In this study, it was observed that marital status of the respondents, knowledge of partners HIV status and membership in the Anti- HIV/AIDS Association were independently associated with disclosure of HIV positive Status. This result is consistent with studies done elsewhere (WHO, 2012; Deribe et al.,, 2008; Seid et al., 2012).
Unmarried respondents were more likely to disclose their HIV positive status compared to the married ones. This finding was contrary with other studies done in Hawasa (Gari et al., 2010). This might be due to the fact that unmarried individuals relatively feel free from parental control.
Knowledge of partner’s HIV status was found to be a predictor of HIV positive status disclosure, which is 3.43 times more likely to disclose their HIV status compared to those who did not know their partners’ HIV status. This agrees with what others reported (Gari et al., 2010; Seid et al., 2012). A majority of the respondents (81.6%) had similar HIV positive status with their partner. This might encourage them to have open communication and freedom to disclose. Partner’s communication among themselves concerning their HIV status is beneficial. Health service providers can address sexual partners on the benefits of disclosing their HIV positive status to one another.
Respondents who were members in Anti- HIV/AIDS Association were more likely to disclose their HIV status as compared to non-members. This finding was in line with the study done in Kemissie District (Seid et al., 2012), suggesting that individuals who are members have frequent discussion related to HIV and they are the first to bring behavioral changes. As a result individuals were able to overcome feelings of shame which facilitated disclosure of HIV positive status.
Most of the study participants (74.7%) experienced positive outcomes after disclosure. This shows that helping individuals to disclose will help them get important services to improve their quality of life contrary to its negative outcomes. In this study, 19 (5.3%) of the respondents reported negative outcome after disclosure, which is similar to studies conducted in Jimma (5.2%) (Deribe et al.,, 2008), but lower than studies in Mettu and Gore towns, which reported 24.1% (Kassaye et al., 2005).
The qualitative part of the information revealed that most respondents disclose their HIV status due to serious medical illness that make them to visit health facility for diagnosis and get admitted after being counseled by health workers. Meanwhile pregnancy was also an event to HIV positive status determined and disclosure is facilitated for the fetus’ survival. Some respondents did not disclose their HIV status due to fear of the future consequence such as fear of being beating, divorce, discrimination and rejection.
The extent of HIV positive status disclosure among HIV positive adults has remained low. Moreover factors that predictors of disclosure of HIV positive status were marital status of respondents, knowledge of partner’s HIV status, and membership in an Anti- AIDS Association. Most of the participants experienced positive outcomes of HIV positive status disclosure. Adherence and ART nurse counselors should give due attention to married people. Couples’ counseling should be encouraged for them to disclose without fear and anxiety. Participation of HIV positive individuals in Anti – HIV/AIDS Associations should be strengthened in societies.
The authors have not declared any conflict of interests.
REFERENCES
|
Annual performance report of Ministry of Health (2010/11). Federal democratic republic of Ethiopia. Health sector development programme IV: Version I.
View
|
|
|
|
Antelman G, Smith FC, Kaaya SF, Fawzi WW (2001). Associated factors of HIV-1 status disclosure: A prospective study among HIV-infected pregnant women in Dares Salaam, Tanzania. AIDS15:1865-1874.
|
|
|
|
|
Axum Woreda Health Office (2012). Annual performance report.
|
|
|
|
|
Deribe K, Woldemichael K, Wondafrash M, Haile A, Amberbir A (2008). Disclosure experience and associated factors among HIV positive men and women clinical service users in southwest Ethiopia. BMC Public Health 8(1):81.
Crossref
|
|
|
|
|
Erku TA, Megabiaw B, Wubshet M (2012). Predictors of HIV status disclosure to sexual partners among people living with HIV/AIDS in Ethiopia. Pan Afr. Med. J. 13:87.
|
|
|
|
|
Federal Ministry of Health (FMOH) (2006). National HIV/AIDS prevention and control office. AIDS IN ETHIOPIA: sixth report.
|
|
|
|
|
Gari T, Habte D, Markos E (2010). HIV positive status disclosure to sexual partner among women attending ART clinic at Hawassa University Referral Hospital, SNNPR, Ethiopia. Ethiop. J. Health Dev. 24(1):9-14.
Crossref
|
|
|
|
|
Haileselasie B, Worku A, Melkamu B, Meresa G (2015). HIV positive status disclosure and associated factors among HIV positive adults in Axum health facilities, Tigray, Northern Ethiopia. Sci. J. Public Health. 3(1):61-66.
Crossref
|
|
|
|
|
Kadowa I, Nuwaha F (2009). Factors influencing disclosure of HIV positive status in Mityana district of Uganda. Afr. Health Sci. 9(1):26-33.
|
|
|
|
|
Kajura NN (2010). The perceived and experienced barriers andreported consequences of HIV positive status disclosure by people living with HIV to their partners and family members in Djibouti (Doctoral dissertation, University of the Western Cape).
|
|
|
|
|
Kassaye KD, Lingerh W, Dejene Y (2005). Determinants and outcomes of disclosing HIV-sero positive status to sexual partners among women in Mettu and Gore towns, Illubabor Zone southwest Ethiopia. Ethiop. J. Health Dev. 19(2):126-131.
Crossref
|
|
|
|
|
Legasion M (2010). A study on Factors associated with non-disclosure of HIV positive status to sexual partners by adult patients attending the VCT clinic at Nhlangano health centre, Swaziland (Doctoral dissertation, University of Limpopo, Medunsa Campus).
|
|
|
|
|
Makin JD, Forsyth BW, Visser MJ, Sikkema KJ, Neufeld S, Jeffery B (2008). Factors affecting disclosure in South African HIV-positive pregnant women. AIDS Patient Care STDs 22(11):907-916.
Crossref
|
|
|
|
|
Mbonu NC, Van Den Borne B, De Vries NK (2011). Societal beliefs and reactions about people living with HIV/AIDS. In: Gobopamang L (eds,) Social and psychological aspects of HIV/AIDS and their ramifications.
|
|
|
|
|
Rapid Response Service (2013). Disclosure of HIV-positive status: Towards the development of guidelines, strategies and interventions. Ontario HIV Treatment Network. Available at:
View
|
|
|
|
|
Seid M, Wasie B, Admassu M (2012). Disclosure of HIV positive result to a sexual partner among adult clinical service users in Kemissie district, northeast Ethiopia. Afr. J. Reprod. Health 16(1):97-104.
|
|
|
|
|
World Health Organization (WHO) (2012). Gender Dimensions of HIV status Discourse to sexual partners: Rates, Barriers & outcomes. A Review paper.
|
|
|
|
|
World Health Organization (WHO) Document Summary (2012). HIV Status Disclosure to Sexual Partners: Rates, Barriers and Outcomes for Women, Rates of HIV status disclosure.
|
|