ABSTRACT
Blood transfusion is an important therapeutic intervention in sickle cell anaemia (SCA). Persons with SCA requiring repeated blood transfusions are at risk of contracting transfusion transmissible infections (TTIs) such as human immunodeficiency virus (HIV). Blood meant for transfusion is usually screened for TTIs to ascertain its safety before transfusion. The study investigated the role of blood transfusion in the spread of HIV among patients with sickle cell anaemia and effectiveness of the screening methods used to prevent HIV acquisition through blood transfusion in Jos. Consenting consecutive patients with sickle cell anaemia attending the Haematology clinic of Jos University Teaching Hospital between November, 2013 and July, 2014 had their blood samples screened for human immunodeficiency virus (HIV) after completing a questionnaire. One hundred and eleven (111) SCA patients aged between 17 and 52 years participated. Seventy six (68.5%) had history of blood transfusion while thirty five (31.5%) had no previous blood transfusion. Nine (8.1%) of them were positive for HIV, which comprised of 3 (8.6%) of the non-transfused and 6 (7.9%) of the transfused (p = 0.911). Blood transfusion though an important risk factor for acquisition of HIV infection, did not play a significant role in this study. Current pre transfusion HIV screening techniques were effective but further improvement in the safety of blood supply can be assured through the use of highly sensitive HIV screening methods and newer technologies.
Key words: Sickle cell anaemia, HIV, blood transfusion.
Sickle cell anaemia, an inherited lifelong haemolytic anaemia is associated with repeated blood transfusion as an integral part of therapeutic intervention for many complications in sufferers (Chou, 2013; Steinberg, 2012). This exposes these patients to the risk of contracting transfusion transmissible infections (TTIs) of which human immunodeficiency virus (HIV) is one (Zia and Taha, 2014). Others include hepatitis B virus (HBV), hepatitis C virus (HCV), and syphilis among others. Blood and blood products transfusion though lifesaving in emergency situations, remains the most efficient way of transmitting life threatening TTIs. The risk of acquisition of these blood borne infectious agents is almost 100% from transfusion of infected blood obtained from infected donors (Roberts et al., 1994).
Laboratory testing to identify HIV infection has been used throughout the world for over 20 years, and continues to be a major intervention in protecting recipients of blood and tissues (Constantine et al., 2005). Serological screening of donor blood for HIV antibodies remains a critical component in identifying and eliminating HIV infected blood donations (Nkengasong et al., 1999) but, this test rarely detect HIV antigen positive blood donors who are in the window period.
Detection of this early viraemic stage continues to be a challenge in transfusion medicine worldwide because of the possibility of transmitting HIV infection (Polywka et al., 2005). Many countries employ stringent blood donor selection criteria to defer potentially infectious donors with high risk of HIV infection and employ highly sensitive screening methods like Nucleic Acid Amplification Testing (NAAT) in a nationally coordinated Blood Transfusion Service. Following this approach, developed countries like the United States of America (USA), United Kingdom (UK) and France have successfully reduced infections through their blood supplies and the window period from an average of 22 days based on antibody ELISA to 11days using NAAT (Busch et al., 2003). In Africa where about 5 to 10% of cases of HIV are reported to have been acquired through blood transfusion (WHO, 2002), the use of sensitive testing assays has persistently posed a daunting challenge for most nations.
In Nigeria, the national prevalence of HIV among blood donors was reported to be 4.4% (PEPFAR, 2006) though, different researchers (Irene, 2002; Durosinmi et al., 2003; Imoru et al., 2003; Ejele et al., 2005) have reported varying prevalence from different parts of Nigeria depending on the setting, nature of blood donation, population prevalence, donor selection criteria and methods of assays employed in testing. Pre-transfusion screening of blood is aimed at reducing to the barest minimum the acquisition of transfusion transmissible infections like HIV through donated blood. Facilities for early detection of infection with newer technologies in asymptomatic carriers thereby narrowing the window period are not available in the study setting. Screening of blood donors rely on available antibody-based detection method for HIV infection. Local data from this centre on the percentage of post transfusion acquired HIV infection are lacking as far as the authors are aware.
This study therefore investigated the role of blood transfusion in the spread of HIV among persons with sickle cell anaemia in an environment with high HIV prevalence and, assessed the effectiveness of the pre-transfusion HIV screening methods presently in use in this study setting where highly sensitive HIV screening methods are lacking.
Ethical consideration
Ethical approval was obtained from the Human Research and Ethics committee of Jos University Teaching Hospital. Informed written consent was obtained from all the participants prior to procedure and confidentiality maintained by removing personal identifiers.
The study conducted a descriptive, cross-sectional prospective study in patients with sickle cell anaemia (SCA) attending Haematology outpatient clinic of Jos University Teaching Hospital (JUTH) in Jos, North Central Nigeria. JUTH is a 600 bed tertiary health facility located in Shere hills bordering the Jos East local government area in Jos, the Plateau State Capital. It serves as a referral Centre for the surrounding states of Benue, Nasarawa, Bauchi, Gombe, Taraba, and Southern Kaduna in Kaduna State as well as other local government areas of Plateau State. Most patients with SCA on the Plateau and environ access care in JUTH, the reason for its choice as the study area.
Consenting consecutive patients with sickle cell anaemia attending the Haematology clinic of Jos University Teaching Hospital between November, 2013 and July, 2014 were enrolled for this study. Other forms of anaemia, haematological disorders and non-consenting patients were excluded. Participants had their blood samples collected and screened for human immunodeficiency virus (HIV) antigen and antibody by ELISA method using fourth generation ELISA kits (GENSCREEENTM Bio-Rad, Marnes-la-Coquette, France). Haemoglobin electrophoresis was carried out using cellulose acetate haemoglobin electrophoresis method at alkaline pH of 8.9 for all participants to confirm their sickle cell status.
Personal data such as age, sex, marital status, history of blood transfusion, where transfused and units of blood received were obtained through structured questionnaires.
Analysis of data
Data obtained from the study was analyzed using Epi info version 7.1.3.0 (CDC Atlanta Georgia, USA). Statistical comparison between the transfused and non-transfused patients’ HIV prevalence was carried out using student t-test. Results with p-values ≤ 0.05 were considered statistically significant. Results were presented in tables.
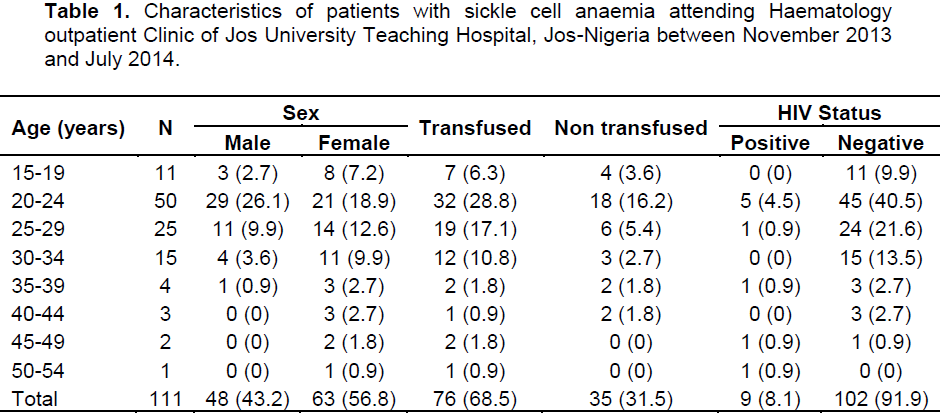
A total of one hundred and eleven (111) patients with SCA were studied. 43.2% were males while 56.8% were females; giving a male: female ratio of 1:1.3. This showed a more female participation in uptake of follow up clinic attendance than males. They were aged between 17 and 52 years. Majorities (81.0%) of the patients studied were between the ages of 20 to 34 years (Table 1) and unmarried (Table 2). This means majority of these patients with SCA were of the youthful and active age group. 68.5% of these patients had history of blood transfusion while 31.5% according to their knowledge had not received blood transfusion previously (Table 2). More females received blood transfusion than their male counterparts, giving a ratio of 1:1.6. Those that received blood transfusion had units ranging from one to more than twenty units. Majority (80%) of those that were transfused received blood at the Jos University Teaching Hospital.
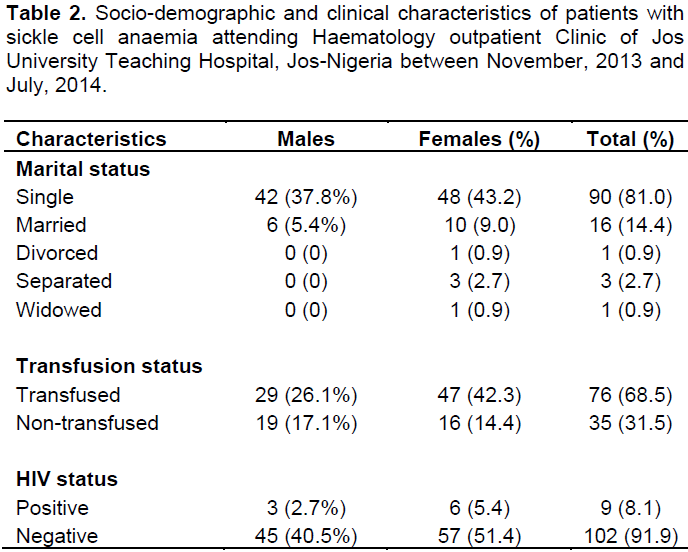
Nine (8.1%) of these patients were positive for HIV. Of those who were positive for HIV, 7.9% had history of previous blood transfusion while 8.6% had no history of previous blood transfusion (Table 3). 66.7% of the transfused patients who were HIV positive were female, 50% of them were married and had received greater than 10 units of blood. 66.7% of the non-transfused HIV positive patients were unmarried males, aged between 21 and 23 years. There was no significant difference between the HIV seropositivity in transfused and non-transfused patients with sickle cell anaemia (Table, 3) (p= 0.911).
This study showed a HIV seroprevalence of 8.1% among the study adult patients with SCA from this Centre. The HIV seroprevalence in this study was higher than the 2012 Nigerian estimated National prevalence of 3.2% Central Intelligence Agency (CIA, 2012) and the reported National HIV prevalence of 3.4% in adults in the 2012 survey (NARHS, 2012). The high prevalence of HIV in patients with SCA in this study may be due to additional risk factors such as exposure to blood and blood products used as therapeutic intervention in their condition. The prevalence of HIV in patients with SCA in this study irrespective of their transfusion status was however lower than that reported from an earlier study in intended blood donors from this Centre which was 9.1% (Egesie et al., 2011). The difference is however not statistically significant (p = 0.749).
The seroprevalence of HIV in patients with SCA who had blood transfusion in this study was observed to be 7.9%. This lower HIV prevalence in transfused patients with SCA when compared with that of previous seroprevalence in intended blood donors from this centre, may be as a result of pre-donation screening for TTIs routinely carried out on all intended blood donors before collection. The difference is however not statistically significant. This measure may have protected this vulnerable group of individuals to some extent from acquiring HIV from infected blood donors. However, blood donors who may be in the window period may have been missed and passed as healthy individuals fit to donate their blood, using the present screening methods employed in pre-transfusion screening of donor blood. This calls for use of newer technologies and highly sensitive screening methods like Nucleic Acid Amplification Testing (NAAT) for detection of early infection so as to narrow the window period.
The seroprevalence of HIV in the transfused patients with SCA in this study was higher than that reported from a study carried out in Yaoundé Central Hospital, Cameroon. In that study, a seroprevalence of 5.6% was observed in transfused SCA patients (Ngo et al., 2013). The high prevalence of HIV in this group of patients was linked to increasing incidence of HIV infection in the general adult population and consequently in the blood donors; a situation that is not far from what is obtainable in the adult population in the study setting. This calls for stringent blood donor selection criteria with deferral of high risk donors.
The seroprevalence of HIV in transfused patients with SCA found in this study was higher than that reported from a study in Enugu, South-Eastern Nigeria (Ubesie et al., 2012). In their study, Ubesie et al. (2012) reported a HIV seroprevalence of 2.9% among transfused patients with SCA. The difference in prevalence may be as a result of the differences in study population and geographical location. The Enugu study was carried out in children with SCA while this study involves adult patients with SCA. Additional risk factors of sexual exposure and transmission of HIV through sexual contact as well as repeated blood transfusion may have contributed to the higher seroprevalence in this study population.
The seroprevalence of HIV among the non-transfused patients with SCA was found to be 8.6%. This was seen in three young unmarried patients with SCA aged 21 to 23 years. As youth who have a lot of energy and are more restive, they are likely to engage in risky behaviours that could expose them to HIV infection. Two out of the three were males and unmarried, while the only female among them was divorced. Although the seroprevalence of HIV in the transfused patients with SCA was twice as high as that found in the non-transfused patients with SCA, there was no statistical significant difference between the two groups (p>0.05). This agrees with a Ghanaian study in which there was no significant association found between blood transfusion and HIV infection in sickle cell disease patients (Baah et al., 2014).
In this study, the number of females who were HIV positive was higher than that of males in a ratio of 1:0.8. This may be due to the fact that there was more female participation in the study than their male counterparts confirming an earlier observation in a study in Cape Coast metropolis, Ghana (Baah et al., 2014). This also confirms the fact that more females uptake sickle cell medical care services than their male counterparts. On the other hand, this might have confirmed the fact that females are more at risk of acquiring HIV infection than their male counterparts (Coombs et al., 2003).
It has been observed that gender plays an important role in the acquisition of HIV infection with the females being at a disadvantaged position. This may not be unconnected with the unique anatomy of the female urogenital system as well as their peculiar physiology increasing their susceptibility to HIV infection than their male counterparts (Koofreh et al., 2008; Myer et al., 2003; Coombs et al., 2003). This fact may have contributed in addition to other factors to the higher seroprevalence of HIV infection observed among the female patients with SCA in this study. It was also observed that more female patients with SCA received blood transfusion than their male counterparts. This is not surprising, considering the added burden of menstrual blood losses, demands of pregnancy and childbirth; female patients with SCA are therefore at higher risk of developing severe anaemia necessitating blood transfusion and consequently acquisition of HIV infection through blood transfusion.
Blood transfusion though an important risk factor for acquisition of HIV infection, did not play a significant role in this study. This was clearly demonstrated by the findings in this study and other previous studies. Increasing regional HIV prevalence in the general population and consequently in blood donors threatens the safety of blood supply. It is therefore very important that measures directed at further improving the safety of blood supply through stringent blood donor selection criteria, use of highly sensitive and improved screening tests aimed at reducing the window period and, alternatives to blood transfusion be instituted in the management of patients with SCA. It is hoped that these measures will further reduce the seroprevalence of HIV infection in this group of individuals through blood transfusion.
The authors are grateful to all the patients with SCA who participated in this study, and also they express their profound gratitude to the Zonal Coordinator and staff of National Blood Transfusion Service (NBTS) North-Central Zone, Jos for the valuable assistance they gave, particularly in the use of their facilities for running the HIV screening of the study participants’ blood samples.
The authors hereby declare that they have no conflict of interest.
REFERENCES
|
Baah ATD, Azumah DE, Ampiah C, Boampong J, Nuvor SV (2014). Incidence of human immunodeficiency virus in sickle cell patients in the Cape Coast Metropolis, Ghana. World J. AIDS. 4:338-345.
Crossref
|
|
|
|
Busch MP, Kleinman SH, Nemo GJ (2003). Current and emerging infectious risks of blood transfusion. JAMA 289(8):959-962.
Crossref
|
|
|
|
|
Central Intelligence Agency (CIA) World factbook (2012). HIV/AIDS –adult prevalence rate in Nigeria.
|
|
|
|
|
Chou ST (2013). Transfusion therapy for sickle cell disease: a balancing act. Hematol. Am. Soc. Hematol. Educ. Program pp. 439-446.
Crossref
|
|
|
|
|
Constantine NT, Zink H (2005). HIV testing technologies after two decades of evolution. Indian J. Med. Res. 121(4):519-38.
|
|
|
|
|
Coombs RW, Reichelderfer PS, Landay AL (2003). Recent observations on HIV type-1 infection in the genital tract of men and women. AIDS 17:455.
Crossref
|
|
|
|
|
Durosinmi MA, Mabayoje VO, Akinola NO, Adegunloge AB, Alabi AO (2003). A retrospective study of prevalence of antibody to HIV in blood donors at Ile-Ife, Nigeria. Niger. Postgrad. Med. J. 10(4):220-223.
|
|
|
|
|
Egesie OJ, Egesie UG (2011). Seroprevalence of human immunodeficiency virus among blood donors in Jos. In: Eugenia Barros (ed). HIV infection – impact, awareness and social implications of living with HIV/AIDS (ISBN 979-953-307-190-8) by In Tech, Rijeka-Croatia. pp. 233-240. www.intechopen.com
|
|
|
|
|
Ejele OA, Nwauche CA, Erhabor O (2005). Seroprevalence of HIV infection among blood donors in Port Harcount, Nigeria. Niger. J. Med. 14(3):287-289.
|
|
|
|
|
Imoru M, Eke C, Adegoke A (2003). Prevalence of hepatitis B Surface antigen, hepatitis C virus and human immunodeficiency virus among blood donors in Kano State, Nigeria. J. Med. Lab. Sci. 12(1):59-63.
|
|
|
|
|
Irene PA (2002). Prevalence of HIV/AIDS virus among blood donors in Lagos Island. A Nigeria experience. Intl. Conf. AIDS. Abstract no. C10834.
|
|
|
|
|
Koofreh M, Nwauche CA, Ughoma HA (2008). Prevalence of HIV infection among secondary school students in two cities in south-south Nigeria. Port Harcourt Med. J. 2(3):253-256.
Crossref
|
|
|
|
|
Myer L, Kuhn L, Stein ZA, Wright TC Jr, Denny L (2003). Intravaginal practices, bacterial vaginosis, and women's susceptibility to HIV infection: epidemiological evidence and biological mechanisms. Lancet Infect. Dis. 5(12):786-794.
Crossref
|
|
|
|
|
National HIV/AIDS and Reproductive Health Survey (NARHS) (2012). National HIV prevalence rate. www.naca.gov.ng/new/content/hiv-prevalence-rate-states
|
|
|
|
|
Ngo SF, Eboumbou C, Ngouadjeu E, Zouhairatou H, Mbanya D (2013). Prevalence of HIV seropositivity among sickle cell disease patients at Yaounde Central Hospital. Health Sci. Dis. 14(2):1-4.
|
|
|
|
|
Nkengasong JN, Maurice C, Koblavi S, Kalou M, Yavo D, Maran M, Bile C, N'guessan K, Kouadio J, Bony S, Wiktor SZ, Greenberg AE (1999). Evaluation of HIV serial and parallel serologic testing algorithms in Abidjan, Cote d'Ivoire. AIDS 13:109-117.
Crossref
|
|
|
|
|
Polywka S, Duttmann H, Lubben F, Laufs R, Felder JA (2005). New Combined HIV P24 Antigen and Anti-HIV 1/2/0 Screening Assay. J. Virol. Methods 304:229-243.
Crossref
|
|
|
|
|
Roberts CR, Longfield JN, Platte RC, Zielmanski KP, Wages J, Fowler A (1994). Transfusion-associated HIV type 1 from screened antibody-negative blood donor. Arch. Pathol. Lab. Med. 118(12):1188-1192.
|
|
|
|
|
Steinberg MH (2012). Sickle cell disease and other haemoglobinopathies. In Goldman, A Shafer, eds., Goldman's Cecil Medicine, 24th ed., Saunders. Philadelphia. pp. 1066-1075.
|
|
|
|
|
The president's emergency plan for AIDS relief. Report on blood safety and HIV/AIDS (2006). http://www.state.gov/documents/organization/74125.pdf
|
|
|
|
|
Ubesie AC, Emodi IJ, Ikefuna AN, Ilechukwu GC, Ilechukwu GCA (2012). Prevalence of human immunodeficiency virus transmission among transfused children with sickle cell anaemia in Enugu, Nigeria. Ann. Med. Health Sci. Res. 2(2):109-113.
Crossref
|
|
|
|
|
World Health Organization (WHO) (2002). Blood safety unit. Aide-Memoire for national blood programmes. Geneva, Switzerland: World Health Organization. http://www.who.int/bloodsafety/transfusion_services/en/Blood_Safety_Eng.pdf
|
|
|
|
|
Zia M, Taha HM (2014). Transfusion-Transmitted Diseases. Medscape. http://emedicine.medscape.com/article/1389957-overview
|
|