ABSTRACT
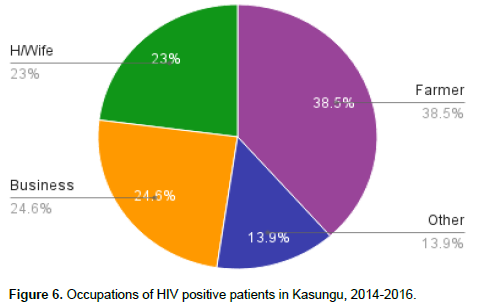
More than 70 million people have been infected worldwide with the HIV virus from the start of the epidemic, and since then, nearly 35 million people have died of HIV. Sub-Saharan Africa remains the most severely affected area, accounting for nearly 70% of the people living with HIV worldwide. Approximately 8.8% of women and men age 15 to 49 in Malawi are HIV positive. Socio-demographic factors affecting the HIV/AIDS epidemic in Kasungu district in Malawi are currently unknown. This study aimed to determine the main socio-demographic factors affecting HIV/AIDS propagation and its treatment in Kasungu district in central Malawi. A descriptive cross sectional study involving 1260 adult participants (aged 18+) living with HIV at both the Kasungu District Hospital and St. Andrew's Hospital was conducted. HIV was common among non-pregnant females (40.9%) compared to pregnant females, (19.3%). HIV was also more common among non-pregnant females than men (40.9% vs. 39.6%, respectively). In general, HIV was more common among farmers (38.5%) and businessmen (24.5%). The main reason for starting anti retro viral (ARV's) was a low CD4 count, seconded by World Health Organization (WHO) clinical stage 3. Nine out of 11 clients had negative reactions towards their HIV positive serostatus. Seven out of 11 clients had thoughts related to suicide or attempted suicide. About 50% of the surveyed patients revealed that they had experienced discrimination due to their HIV positive status.
Key words: HIV/AIDS, demographic factors, social factors.
Since the beginning of the HIV epidemic, more than 70 million people have been infected with the virus and about 35 million people have died of HIV. Prevention programs such as massive expansion of antiretroviral therapy (ART) have reduced the global number of people dying from HIV-related causes to about 1.1 million in 2015, which is 45% fewer than in 2005, when HIV-related mortality peaked (WHO Progress Report, 2016). The Joint United Nations Programme on HIV/AIDS (UNAIDS)/World Health Organization (WHO) estimates show that more than 18 million people were receiving ART in mid-2016. 2020 Fast-Track targets have been set to accelerate the HIV response towards ending the AIDS epidemic by 2030. These Fast-Track targets apply to everyone: children, adolescents and adults; rich and poor; women and men; and all key populations including sex workers, people who inject drugs, men who have sex with men, transgender people and prisoners. The Fast-Track targets include the 90-90-90 target: 90% of the people living with HIV know their HIV status, 90% of the people who know their HIV-positive status and are accessing treatment, and 90% of the people receiving treatment with suppressed viral loads (WHO, 2016).
Sub-Saharan Africa remains the most severely affected, with nearly 1 in every 25 adults (4.4%) living with HIV and accounting for nearly 70% of the people living with HIV worldwide (WHO, 2016). The 2015-2016 Malawi Demographic and Health Survey found that approximately 8.8% of women and men age 15 to 49 in Malawi are HIV positive. The HIV prevalence is higher among women than men (10.8% versus 6.4%) (Malawi Demographic and Health Survey, 2015-16). HIV/AIDS is more prevalent among sex workers, people who inject drugs, men who have sex with men, transgender people, and prisoners. In Malawi, reactions, misconceptions, and discrimination status of clients who are newly diagnosed to be HIV positive vary from population to population. At present, the socio-demographic factors affecting HIV/AIDS epidemic in Kasungu district are largely unknown and undocumented. Also we were not aware of whether discrimination was an issue of concern in HIV/AIDS management in Kasungu district or not.
Main objective
To determine socio-demographic factors affecting HIV/AIDS and its treatment in Kasungu district.
Specific objectives
1. To evaluate socio-demographic factors that affect HIV/AIDS in Kasungu district.
2. To investigate the socio-demographic factors affecting the quality of care and life of HIV/AIDS clients in Kasungu district.
Study setting, population, eligibility criteria and data analysis
This was a descriptive cross section study which was conducted at Kasungu district and St. Andrew's Hospitals in 2016. It involved a total of 1,260 adult participants (aged 18+) living with HIV; 981 participants were from Kasungu hospital, and 279 participants were from St. Andrew’s Hospital. Kasungu District Hospital has a bed capacity of 217 beds and offers both primary and secondary care services. Its catchment population is approximately 150,000 people. St Andrews Hospital has a catchment population of approximately 40,000 people and offers both primary and secondary care services. HIV prevalence in Kasungu District is 4.6% which is lower than the country’s prevalence of about 10%. To achieve the objectives, HIV/AIDS Registry data from Anti-retroviral therapy (ART) and HIV Testing and Counselling (HTC) clinics were extracted manually. The registers were made available to the data collectors by the leadership from both institutions. The 2014 to 2016 registry was used to extract the data from 1st January, 2014 to 31st December, 2016. From the ART register, number of males and females on ART for the period under review was extracted. Reasons for starting ART for each individual on ART were extracted as well. Socio-economic status of each individual on ART was also extracted. Microsoft Excel was used to enter and analyse the data. Tables, bar charts and pie charts were created to present the results.
HIV was common among non-pregnant females (40.9%) compared to pregnant females, (19.3%). HIV was more common among non-pregnant females than men (40.9 vs. 39.6%, respectively). Overall, HIV was common among females compared to males, Figures 1 and 2, and the younger demographic was mainly affected by HIV; such that HIV was most common within the ages of 20 to 50 years, Figure 3. Overall, the main reason for starting ARV was a low CD4 count, seconded by symptoms from WHO clinical stage 3 (Figures 4 and 5). Among females, the main reason for starting ART was a low CD4 count seconded by HIV in pregnancy. HIV was more common among farmers (38.5%) and Business people (24.5%).
This study revealed that HIV in Kasungu district was more common among females than males, 40.9% vs. 39.6%, respectively. This finding is consistent with MDHS 2015-16 findings whereby the HIV prevalence was also higher among women than men (10.8% versus 6.4%). Compared to men, women are often powerless to negotiate safe sex properly - this is a common phenomenon in several African countries, especially amongst poorer rural populations (Ung et al., 2014). The results indicated that the main reason for patients starting ARV was a low CD4 count f ollowed by WHO clinical stage 3 symptoms. This finding is due to the fact that this survey was conducted before UNAIDs rolled out the “Test All Treat All” campaign in 2016, whereby everyone who tests positive for HIV starts treatment immediately regardless of CD4 count (WHO Progress Report, 2016). The main reason for starting ART for females in particular was a low CD4 count seconded by HIV in pregnancy, Figure 4. More women started ART because of pregnancy as part of prevention of mother to child transmission of HIV (PMTCT) option B+, since it is much more likely for African mothers to experience MTCT (Drake et al., 2014).
HIV was common among farmers and business owners (38.5 and 24.5%, respectively), Figure 6. This finding was expected, as most of the population of Kasungu district is made up of commercial farmers and business people who engage in promiscuous sexual behaviours that lead to higher HIV prevalence. Stigma has been described as a dynamic process of devaluation that signiï¬cantly discredits an individual in the eyes of others. HIV-related stigma is multi-layered building upon and reinforcing negative connotations through the association of HIV and AIDS with already marginalized behaviours, such as sex work, drug use, and homosexuality and being transgender. Discrimination consists of actions or omissions that are derived from stigma and directed towards those individuals who are stigmatized. Both stigma and discrimination often have negative consequences on the lives of those living with HIV, and can promote risky behaviours due to fear of judgement (Valdiserri et al., 2002; Dos Santos et al., 2014, Reimers et al., 2016). Our survey results indicate that internalized stigma and discrimination related to HIV-status is still prevalent in Kasungu, despite the fact that many people receive information about HIV/AIDS before they get tested, via the hospital staff.
The exact source of this stigma and discrimination are still unknown, but due to the confidential nature of HIV-status in Kasungu, patients may have experienced discrimination from family members, friends, or hospital staff. It is not uncommon for discrimination towards HIV-positive patients to manifest in the form of unprofessional treatment and care (Valdiserri et al., 2002). This is consistent with the findings of Peter Aggleton et al in April 2005, which revealed that people living with HIV and their caregivers reported receiving differential and discriminatory treatment from health-care workers. Discrimination lead to isolation in wards, early discharge from hospital, delays in surgery, and serious breaches of conï¬dentiality—all effectively limiting access to proper care (Aggleton et al., 2005).A little more than half of the surveyed patients had misconceptions about HIV before they were tested. This indicates that the general population of Kasungu is not very well educated about the details of HIV/AIDS, although information is available publicly through radio broadcasts and posters.
In Kasungu district, HIV is more common among females than males and HIV is common among young female population compared to young males. Between 2014 and 2016, many HIV positive clients in Kasungu started ART due to low CD4 count and WHO clinical stage 3. More farmers and business people in Kasungu district continue to suffer HIV disease than other occupations. Hence, interventions to prevent new infections should be implemented among most of the female population, farmers and business community in Kasungu district.
The authors have not declared any conflict of interests.
The authors appreciate the STEM Research Institute and Youth with Talents for sponsoring this medical project. The cooperation of the authorities of Kasungu District Hospital is gratefully acknowledged.
REFERENCES
|
Aggleton P, Wood K, Malcolm A, Parker R (2005). HIV-related stigma discrimination and human rights violations: case studies of successful programmes. Available at:
View
|
|
|
|
Dos Santos MM, Kruger P, Mellors SE, Wolvaardt G, Van Der Ryst E (2014). An exploratory survey measuring stigma and discrimination experienced by people living with HIV/AIDS in South Africa: the People Living with HIV Stigma Index. BMC Public Health 14(1):80.
Crossref
|
|
|
|
|
Drake AL, Wagner A, Richardson B, John-Stewart G (2014). Incident HIV during pregnancy and postpartum and risk of mother-to-child HIV transmission: a systematic review and meta-analysis. PLoS Med. 11(2):e1001608.
Crossref
|
|
|
|
|
Malawi Demographic and Health Survey; 2015-16 report. Available at:
View
|
|
|
|
|
Reimers P, Israel-Ballard K, Spies L, Tanser F, Thior I, Scott Gordon W, Coutsoudis A (2016). A Protocol for a Cluster Randomized Trial on the Effect of a "feeding buddy" Program on adherence to the Prevention of Mother-To-Child-Transmission Guidelines in a Rural Area of KwaZulu-Natal, South Africa. J. Acquir. Immune Defic. Syndromes 72(Suppl 2):S130-S136.
Crossref
|
|
|
|
|
Ung M, Boateng GO, Armah FA, Amoyaw JA, Luginaah I, Kuuire V (2014). Negotiation for safer sex among married women in Cambodia: the role of women's autonomy. J. Biosoc. Sci. 46:90-106.
|
|
|
|
|
Valdiserri RO (2002). HIV/AIDS Stigma: An Impediment to Public Health. Am. J. Public Health 92(3):341-342.
Crossref
|
|
|
|
|
WHO Progress Report (2016). Prevent HIV, Test and Treat All. WHO Support for Country Impact.
|
|
|
|
|
World Health Organization (WHO) (2016). Global health sector strategy on HIV/AIDS 2016–2021
|
|