ABSTRACT
Human immunodeficiency virus/acquired immune deficiency syndromes (HIV/AIDS)-related stigmatization and discrimination have been acknowledged as an impediment to mitigating the HIV epidemic and little is known about its contributory factors in Nigeria. Therefore, this study investigated factors associated with HIV/AIDS perceived stigmatization and discrimination among women of reproductive age in Nigeria. This was a retrospective analysis of data on 15,639 women of reproductive age (15 to 49 years) collected during the National HIV/AIDS and Reproductive Health Survey (NARHS Plus II) conducted in 2012. Perceived stigma was measured using specific questions and scored as follows: less or equal to 3 points (low stigma), 4 to 6 points (moderate stigma) and greater than or equal to 7 points (high stigma). Data were summarized using descriptive statistics while chi square test was used to assess significance of association of qualitative variables and level of stigma. A multinomial logistic regression model was fitted to determine variables associated with stigma at 5% level of significance. The mean age of women was 29 ± 9.54 years. About 44, 21 and 35% reported low, moderate and high stigma, respectively. Level of education and HIV knowledge were significantly associated with perceived stigmatization (p<0.001). Respondents with poor HIV knowledge were three times more likely to report high level of stigma (odd ratio (OR) = 3.38, 95% confidence interval (CI) = 2.54 - 4.49, p< 0.001). In addition, respondents with primary education were 4 times more likely to report high stigma when compared with those that have higher education (OR = 3.80, 95% CI = 2.36-6.13, p <0.001). Perceived HIV/AIDS-related stigmatization was common among women of reproductive age in Nigeria. Low education level, condom and antiretroviral drug awareness were significantly related to perceived stigmatization among women of reproductive age in Nigeria.
Key words: Perceived stigmatization and discrimination, human immunodeficiency virus/acquired immune deficiency syndromes (HIV/AIDS), women of reproductive age.
Various studies demonstrated human immunodeficiency virus (HIV)-related stigma as common worldwide phenomenon which occurs in a variety of contexts including family, community, workplace, markets and healthcare settings (Mahendra et al., 2007).
The mental well-being, social and economic effect on people living with the virus, has a devastating impact on their families and the community (Mutalewa et al., 2008). Fear, stigma and discrimination have continued to accompany the HIV pandemic. People who are infected, or even suspected of having HIV, have experienced emotional, physical, and structural abuse (Dlamini et al., 2007), and the fear of experiencing such stigma discourages people living with HIV/AIDS (PLWHA) from seeking medical care (Pulerwitz et al., 2010). HIV/AIDS-related stigma and discrimination has negative effect to willingness to test for HIV or to disclose positive outcome to partners. Stigma is often associated with discrimination and human rights which has several undermining effects.
Studies have shown that PLWHA, were often time rejected, restricted from sharing toilets, canteens and sports facilities. Some lost their jobs, some were threatened with dismissal, job duties were changed, some lost prospects for promotion and were excluded from insurance schemes (Chinwe, 2005, 2007).
According to Stangl et al. (2013), stigma and discrimination are broadly significant in diverse ways. Some people are avoided by family, peers and the wider communities, while others face maltreatment in healthcare and educational settings, erosion of their human rights, and psychological damage resulting to a limiting access to HIV testing, treatment and other HIV services. A study by Dlamini et al. (2009) also reveals that stigmatization undermines prevention, voluntary counseling and testing, care and support as well as increases the impact of the infection on individuals, families, communities and nations.
Nigeria is the second largest HIV epidemic in the world (National Agency for the Control of Aids [NACA], 2015). Although HIV prevalence among adults is remarkably small (3.1%) compared to other sub-Saharan African countries such as South Africa (19.2%) and Zambia (12.9%) (UNAIDS, 2016).
In Nigeria, as in most cases, HIV/AIDS is perceived to be a disease of other people living on the margins of society, whose lifestyles are considered perverted and sinful (Nduonofit et al., 2012). Stigmatization and discrimination attached to being diagnosed with HIV/AIDS is far greater and significantly different than that linked to being diagnosed with other illnesses such as cancer and psychiatric disorders (Nduonofit et al., 2012).
HIV-related stigmatization and discrimination has been acknowledged as an impediment to mitigating the HIV epidemic since its early days, yet programming and activities to reduce stigma and discrimination have received much less attention than other aspects of the disease. Recently, there has been an increase in the literature on HIV-stigma, as the issue has gained visibility and greater conceptual clarity (Nyblade et al., 2013; Stein and Li 2008; Akanbi et al., 2010). A significant challenge to the success of achieving universal access to HIV prevention, treatment, care and support by 2010 is HIV-AIDS stigma and discrimination (Emmanuel et al., 2009).
Prior studies that examined stigmatization in HIV-positive women have focused predominantly on either socio-demographic (Ogilvie et al., 2007; Oladapo et al., 2005) or psychological correlates (Rao et al., 2007; Wingood et al., 2007) and HIV-Stigma structural equation (Rao et al., 2012). A previous study by Olalekan (2012) also examined the relationship between psycho demographic factors and perceived stigmatization among people living with HIV/AIDS in Ibadan, Nigeria which revealed a significant relationship between perceived stigmatization and both HIV cognition and HIV disclosure. This study showed that females are more stigmatized than males and younger females with poor HIV cognition had the highest HIV disclosure and stigmatization (Olelakan, 2012). Although, none of these studies focused on the stigmatizing effect among women of reproductive age who are HIV positive. This study was conducted to fill this gap by identifying the socio demographic and psycho-demographic factors influencing HIV stigmatization among women.
Nonetheless, a study by Kinsler et al. (2007) looked at some of the issues surrounding HIV stigma amongst women in a low-income setting. The study reveals that lack of access or delayed access to care influences the quality of life of its patients, health opportunities and psychological well-being of HIV positive women. Globally, HIV is the leading cause of death among women of childbearing age (UNAIDS, 2014). Women accounted for more than half of the people infected with HIV and represent a growing proportion of people living with HIV/AIDS (Kola et al., 2005). Also, women have greater likelihood than men of being infected in heterosexual encounters (WHO, 2006). HIV affects all aspects of women’s reproductive health such as pregnancy, childbirth, breastfeeding, abortion, use of contraception, exposure, diagnosis and treatment of sexually transmitted infections (STIs) and their exposure to sexual violence. It also affects their sexual health and well-being.
Young women may be unable to negotiate condom use and are more likely than men to experience coerced sex (Krug et al., 2006). In many Africa countries, women are disproportionately affected, not only by HIV/AIDS disease, but also by the related stigma and discrimination (Chinwe, 2005). Leclerc-Madlala (2002) opined that the attachment of gender discrimination to HIV stigma has led to women being blamed for spreading the epidemic.
Due to the stigma and discrimination attached to HIV/AIDs, it is particularly important that health service providers protect the reproductive rights of women living with HIV. These rights include having access to sexual and reproductive health services, decision on whether to be sexually active or not, spacing and timing of childbearing and the right to make these decisions free of discrimination, coercion and violence (UNAIDS, 2006). Also, women who experience fear or stigma have less access to health care services, and research has shown that pregnant women who anticipate HIV related stigma are less likely to get tested for HIV (Turan et al., 2008).
As postulated by Jonathan HIV-Stigma is the third phase of the HIV pandemic which poses a serious threat to prevention and treatment (Mann, 1987). Also, Nigeria aimed to achieve her national policy on HIV/AIDS, by controlling the spread of the infection and its impact, as well as the needs to address the issue of stigmatization and discrimination. It is therefore very important to tackle HIV/AIDS and its consequential stigmatization and discrimination among women of reproductive age who are known to be sexually active. The global health community has set some important goals as part of efforts to control and end HIV/AIDS scourge by 2030, a prevailing drive established towards ensuring that 90% declined in deaths of people living with HIV/AIDS by 2020 via early diagnosis, treatment and viral suppression (USAID, 2014). In Nigeria, issues relating to stigmatization and discrimination of people living with HIV/AIDS (PLWHAs) among reproductive women have not been fully explored. Information on the stigmatization of AIDS in Nigeria has focused on workplace discriminations, prevention programs, counseling and health provider’s anxiety among others (Chinwe, 2007; Oku et al., 2013; Vanden et al., 2009). Hence, this study utilized a nationally representative sample to determine the socio and psycho demographic factors affecting perceived stigmatization and discrimination against PLHWA among women of reproductive age in Nigeria.
Study design and population
A retrospective data analysis of the Nigeria Federal Ministry of Health (2013) and National HIV/AIDS and Reproductive Health Survey 2012 (NARHS Plus) was carried out. The 2012 NARHS Plus was a cross sectional study of men and women of reproductive age. A stratified multistage cluster sampling technique was used to select a nationally representative probability sample of women aged 15 to 49 years and men aged 15 to 64 years living in households in rural and urban areas in all the 36 states and the Federal Capital Territory (FCT), Nigeria.
First stage of sampling involved the selection of rural and urban localities from each state and FCT. Second stage involved the selection of Enumeration Areas (EA) within the selected rural and urban localities. The third stage involved the listing and selection of households. Thirty-two households were sampled from each of the 30 sampled EA (clusters) from each state. A total of 32543 (91.6%) out of selected 35520 individuals were selected using structured. questionnaires. However, all analyses in this study are based on responses by 15639 women respondents that are within reproductive age of 15 to 49 years. The data was weighted to reflect differences in population sizes of the states.
Data management
Descriptive statistics were used to summarize the data. Chi-square test was used to investigate association between categorical variables (perceived stigmatization and the explanatory variables) and multinomial logistic regression analysis was used to further investigate association and the contribution of explanatory variables (factors) on perceived stigmatization. Analysis was done using the statistical package for social sciences (SPSS) Version 20.0 (SPSS, Chicago IL, USA). The dependent variable HIV-related perceived stigmatization and discrimination was measured using seven questions about respondents’ discriminatory attitudes against people living with HIV/AIDS. These questions were selected based on previous studies (Ochako et al., 2011; Sophoan, 2013).
Questions used to measure perceived stigmatization and discrimination include:
(1) Would you be willing to eat from the same dish with a person you knew had the virus that causes AIDS (HIV)?
(2) If a male relative of yours became ill with AIDS, would you be willing to care for him in your household?
(3) If a student has the virus that causes AIDS (HIV) but is not sick, should he or she be allowed to continue attending school?
(4) If a female relative of yours became ill with AIDS, would you be willing to care for him in your household?
(5) If a female teacher has the virus that causes AIDS (HIV) but is not sick, should she be allowed to continue teaching in school?
(6) If you knew a shopkeeper or food seller who had the virus that causes AIDS (HIV), would you buy food from him/her?
(7) In your own view, do you think your community cares and support PLWHA.
These seven questions were used to create and compute the dependent variable. Values were assigned to responses and were scored as follows: agree =0, neutral =1, and disagree =2 which was summed up to generate total scores with a minimum and maximum score of 0 and 14, respectively.
The total scores were disaggregated into 3 categories using percentile ranges. The 25, 50 and 75th percentiles were 2, 4 and 7, respectively. Values less than 4 (0-3) were categorized as “low” stigma, values between 4 and 6 represented “moderate” stigma, and values ≥ 7 indicated “high” stigma (Adewuya and Makanjuola, 2008; Bogardus, 1925). Pearson’s chi square test was used to determine the association between perceived stigmatization and each of the independent variables. Multinomial logistic regression analysis was employed to determine the relationship between perceived stigmatization and the explanatory variables. The explanatory variables that were utilized in the multinomial logistic regression analysis were socio (age, education, marital status, occupation and religion) and psycho demographic variables such as alcohol use, sexual history and behavior, STIs, HIV knowledge, prevention, misconceptions, testing and risk perception. Odds Ratio (OR) and their 95% confidence intervals (CI) were determined. P-value < 0.05 was considered statistically significant.
Seven questions were used to measure comprehensive knowledge of HIV/AIDS (UNGASS, 2010; Ochako et al., 2011; Sophoan 2013). One point was awarded for a correct answer and 0 point for an incorrect choice or no response. Total scores for each respondent ranged from 0 to 7. ‘Score 0 to 6’, indicates the persons had poor knowledge about HIV transmission routes and beliefs, and ‘Score 7’ indicates the persons had a good knowledge about HIV transmission routes and beliefs. Correct responses to all the seven questions were categorized as good knowledge while a wrong response to at least one question was rated as poor knowledge (UNGASS, 2010).
A total of 15,639 records were available for analysis. The mean age of the women was 29 years (SD=9.5 years). The respondents’ age, education, marital status, occupation and religion were found to be significantly associated with stigmatization.
About 6039 (44%) respondents reported low stigmatization, 2907 (21%) moderate stigmatization, and 4805 (35%) high stigmatization.
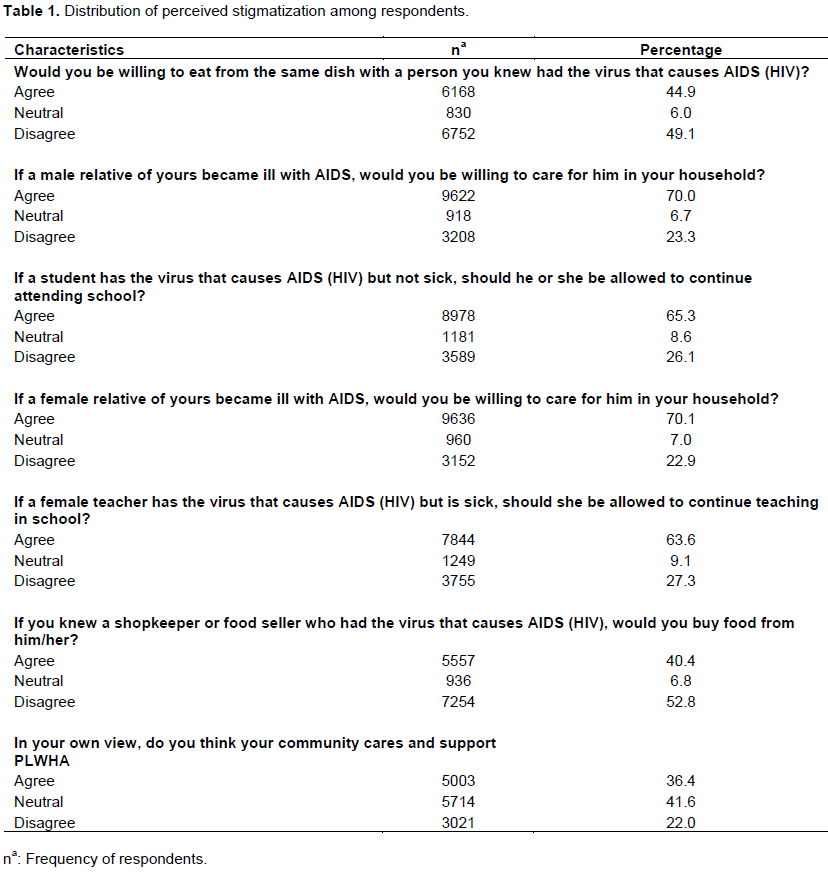
Frequency distribution of items on perceived stigmatization
Slightly less than half (44.9%) agreed to eat from the same dish with person they knew had the virus that causes HIV/AIDS. Majority of the respondents (70.0%) agreed to care for male relatives that are ill with AIDS in their household while 23.3% disagreed. About 64% agreed that a female teacher with the virus that causes AIDS (HIV) should be allowed to continue teaching in school while 27.3% disagreed. Table 1 shows the distribution of the respondents by perceived stigmatization.
Association between socio-demographic factors and perceived stigmatization among women of reproductive age
The proportion with high stigmatization reduced significantly with increasing levels of education (primary: 36.6%, secondary: 31.0%, tertiary: 16.1%) (p<0.001). About 40% of unemployed respondents had high stigmatization compared with 31% who were students and 35% who were self-employed (p<0.001).
A larger proportion (36.4%) reported high stigmatization among the 15 to 24-year-old compared to 33.5% in the 25 to 39 years and 35.5% in the 40 to 49 years. The proportion with high stigmatization was significantly higher among those who were separated/divorced (39.7%), compared to those who were currently married (35.8%), never married (32.1%) and widowed (34.9%) (p=0.001).
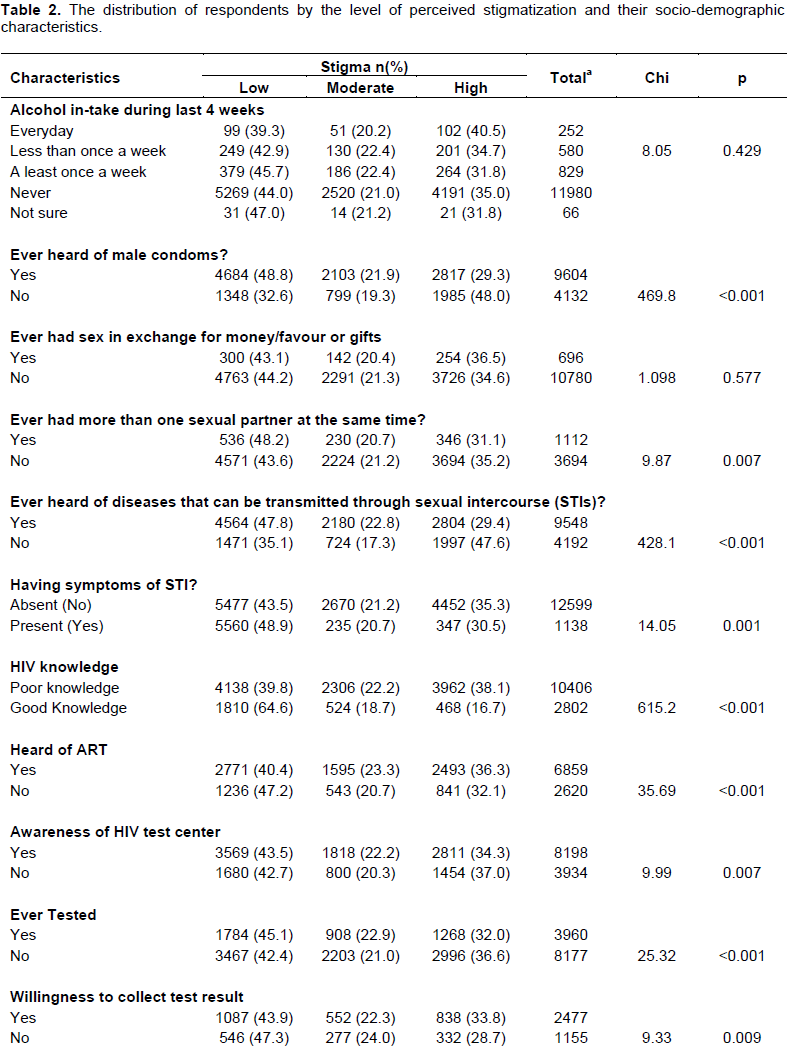
Table 2 shows the distribution of the women of reproductive age by level of perceived stigmatization and socio-demographic characteristics.
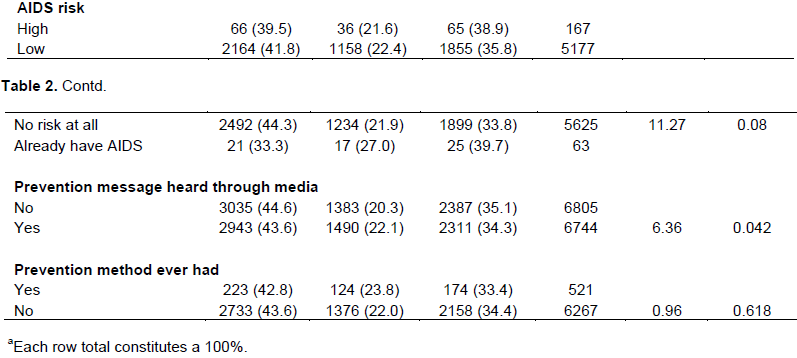
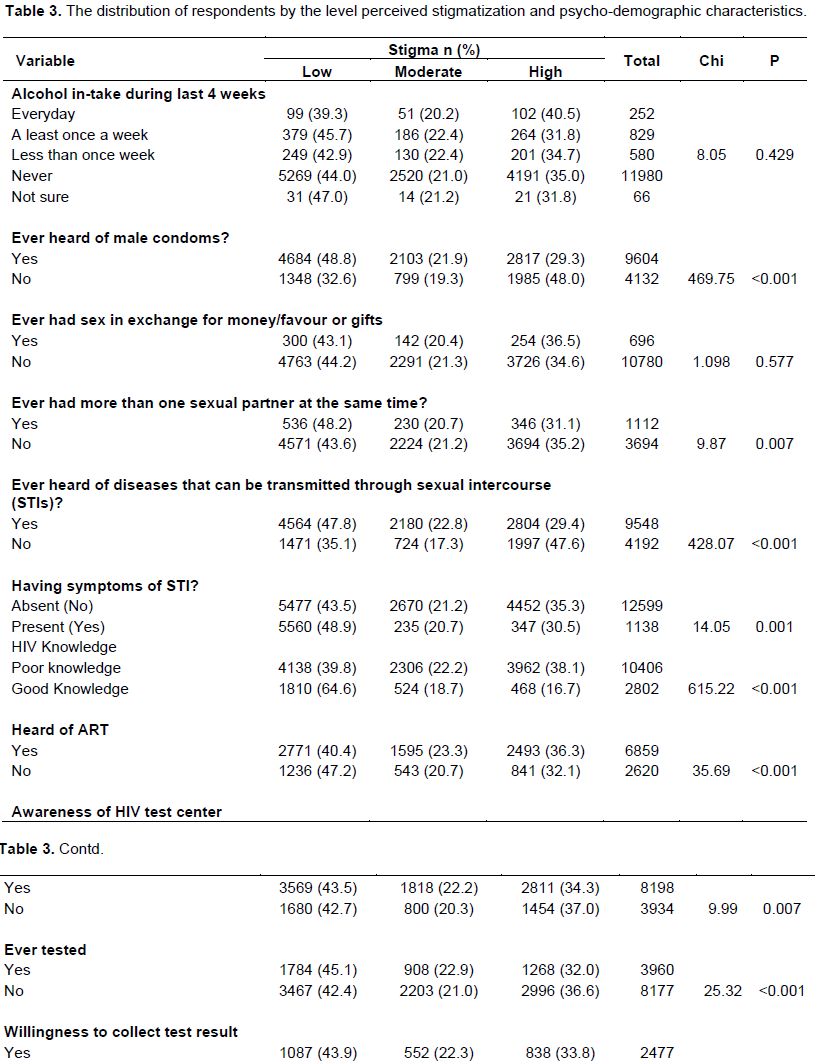
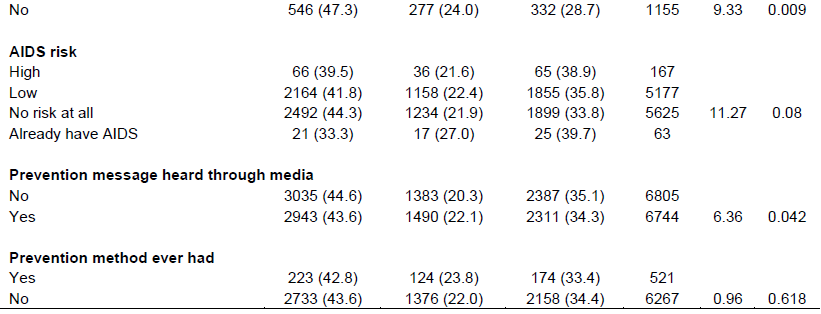
The relationship between psycho-demographic factors and perceived stigmatization among respondents
About half (48.8%) of the respondents that have heard about male condom had low stigmatization compared to
32.6% who were unaware (p< 0.001). Of the 1112 respondents that had more than one sexual partner at the same time, 48.2, 20.7 and 31.1% reported low, moderate and high stigmatization, respectively (p= 0.007).
About 40% with poor HIV knowledge had low stigmatization compared with 64.6% who had good knowledge. Of the 6859 respondents who had heard of antiretroviral drugs, 40.4, 23.3, and 36.3% had low, moderate and high stigmatization, respectively (p<0.001). Of the 3960 respondents that have ever tested for HIV, 45.1, 22.9 and 32.0% reported low, moderate and high stigmatization, respectively (p <0.001).
About 44.5% of the respondents that were willing to test for HIV had low stigmatization compared with 22.8 and 32.7% with moderate and high stigmatization, respectively (p<0.001).
Out of 2477 respondents willing to get HIV test results, 43.9% had low stigmatization, while 22.3 and 33.8% reported moderate and high stigmatization, respectively (p =0.009).
Respondents that have heard about HIV prevention messages through media had low stigmatization (43.6%) and those that have not heard about HIV prevention messages had high stigmatization (34.3%) (p=0.042) (Table 3).
Multinomial logistic regression analysis of perceived stigmatization and selected socio-demographic and psycho-demographic variables
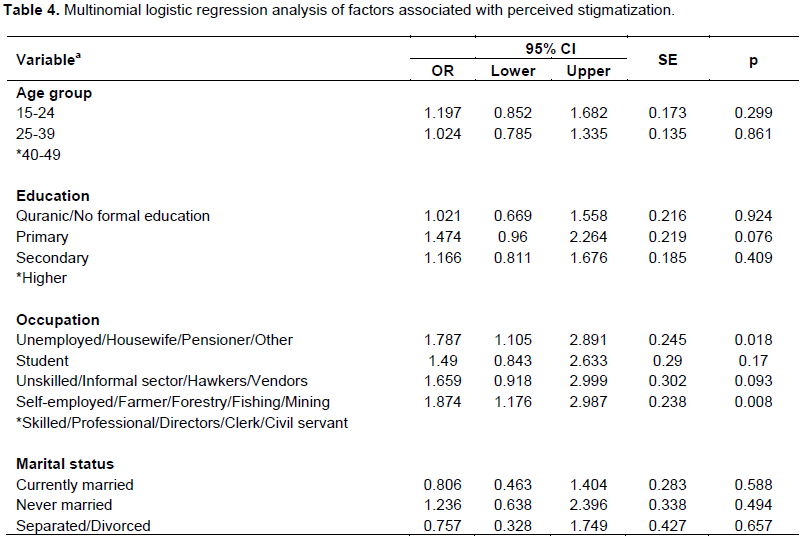
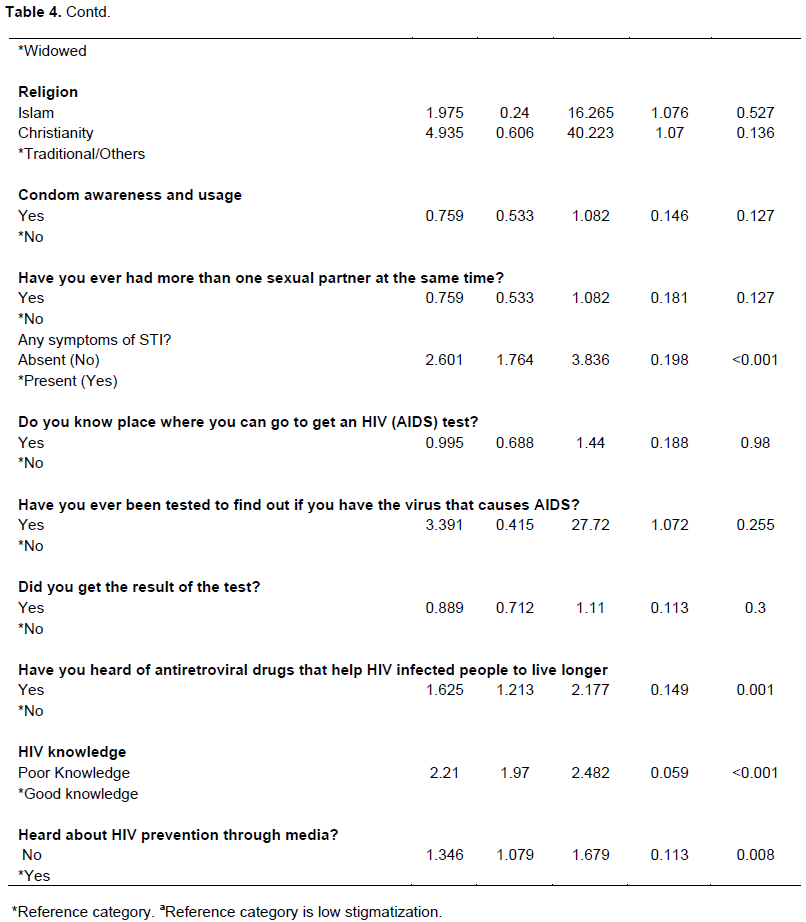
Moderate stigmatization relative to low stigmatization
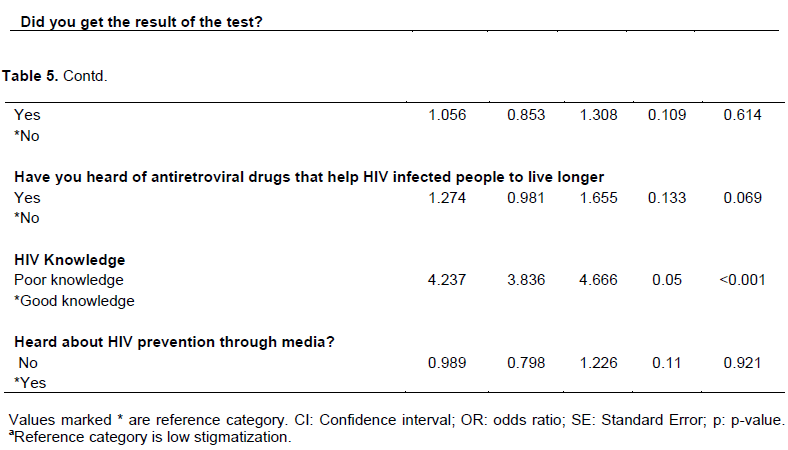
Table 4 shows the results of a multinomial logistic regression model of perceived stigmatization on both socio demographic and psycho-demographic variables.
For moderate stigmatization, relative to low stigmatization the results revealed that among the occupation categories, respondents that were unemployed/not working were about 2 times more likely to exhibit moderate stigma relative to those that were skilled/professional (OR = 1.79, 95% CI = 1.11-2.90, p = 0.02). Respondents that were self-employed were 2 times more likely to report moderate stigma when compared with those that had skilled occupations (OR = 1.87, 95% CI= 1.18-2.99, p=0.008). Respondents who had heard about special antiretroviral drugs were about 2 times more likely to exhibit moderate stigma when compared with respondents that have not heard about antiretroviral drug (OR =1.63, 95% CI=1.21-2.18, p= 0.001). Respondents with poor knowledge about HIV were about 2 times more likely to experience moderate stigma relative to those that have good knowledge about HIV (OR = 1.71, 95% CI =1.33-2.19, p < 0.001). Respondents who have not heard about HIV prevention through media were likely to report moderate stigma when compared with those who have heard about HIV prevention through media (OR = 1.35, 95% CI = 1.08 -1.68, p = 0.008).
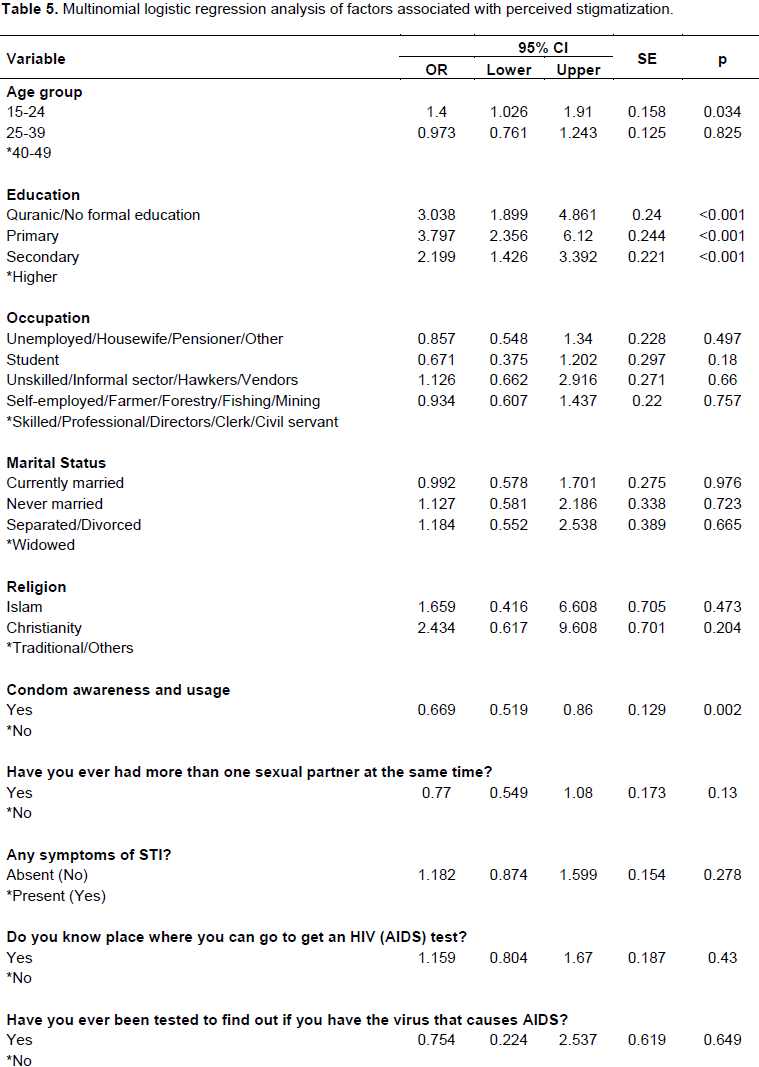
High stigmatization relative to low stigmatization
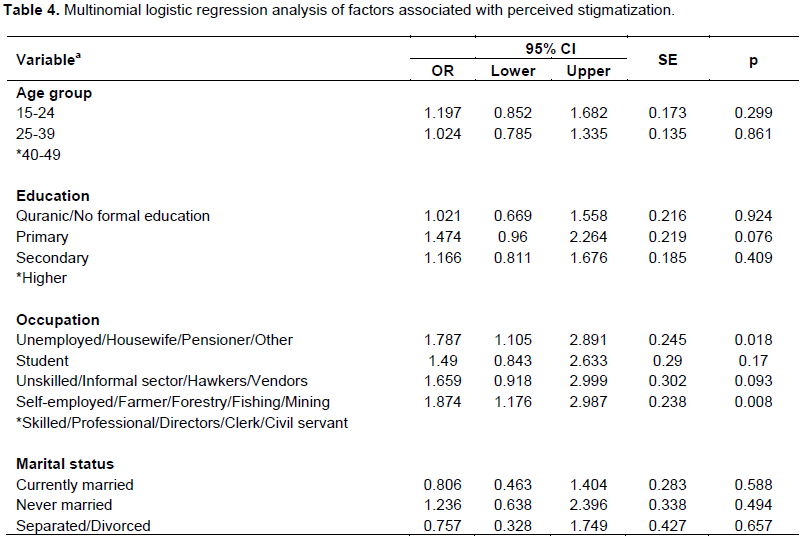
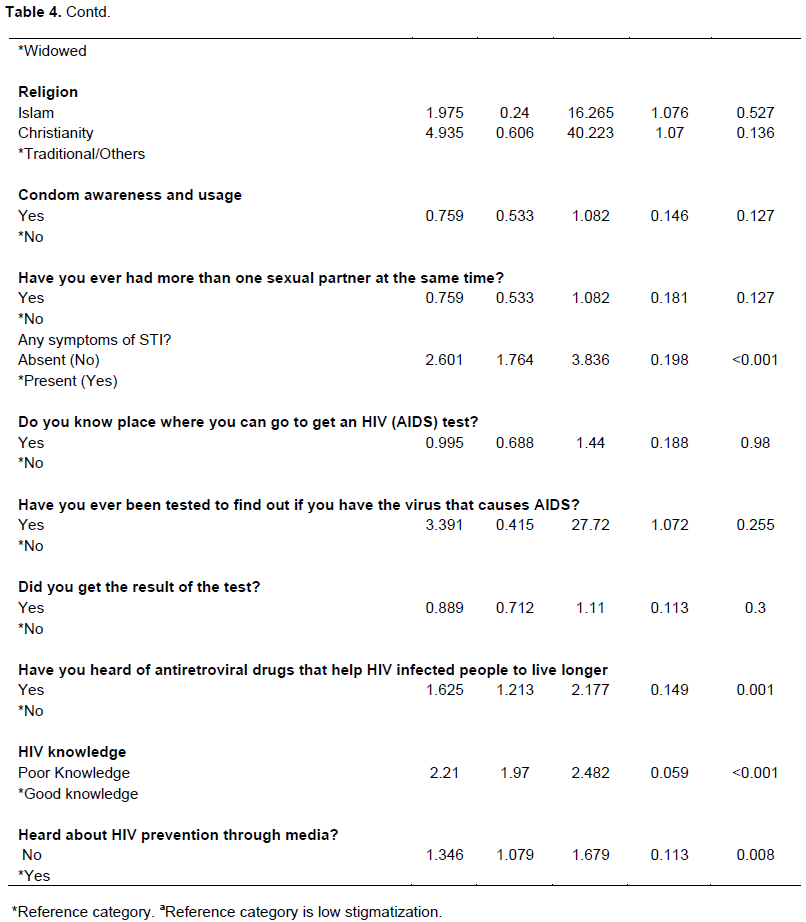
Table 5 shows the results of a multinomial logistic regression model of perceived stigmatization on both socio demographic and psycho-demographic variables.
For high stigmatization, relative to low stigmatization, respondents in age group 15 to 24 years were more likely to exhibit high stigmatization when compared with those in age group 40 to 49 years (OR = 1.40, 95% CI = 1.03 - 1.91, p= 0.034).
Respondents with no formal education were 3 times likely to report high stigmatization when compared with those that have higher education (OR = 3.04, 95% CI = 1.90-4.86, p < 0.001). Furthermore, respondents with primary education were 4 times more likely to exhibit high stigma relative to those that have higher education (OR = 3.80, 95% CI = 2.36-6.13, p <0.001). Respondents with secondary education were 2 times more likely to report high stigma when compared with those that have higher education (OR = 2.20, 95% CI = 1.43 -3.39, p < 0.001). The respondents with knowledge of condom use were 33% less likely to exhibit high stigmatization compared to those that do not have knowledge of condom use (OR = 0.70, 95% CI = 0.52 -0.86, p = 0.002). Respondents who have poor knowledge of HIV were 3 times more likely to report high stigmatization compared with those that have good knowledge of HIV (OR = 3.38, 95% CI = 2.54 - 4.49, p< 0.001).
To our knowledge, this is the first report of a nationally representative study of HIV/AIDs on perceived stigmatization among women of reproductive age in Nigeria. Stigmatization against infected and affected individuals with HIV/AIDS has been identified as a restraint to addressing HIV epidemic in Nigeria. The stigmatization and discrimination attitudes create a situation that facilitates the spread of the disease; and this can be reduced by developing effective strategies.
The results from this study showed that age, education, occupation, use of ART, HIV knowledge and condom awareness were significant determinants of perceived stigmatization. The finding that perceived stigmatization was significantly higher among younger women (15 to 24 years of age) than older women (those within the 40 to 49 years) is consistent with findings by Chellan (2011) who reported that males below 24 years of age usually have erroneous beliefs about the modes of transmission and prevention practices which leads to stigmatizing attitude. This was further corroborated by Kola et al. (2005) who revealed that younger women within 15 to 24 years were more likely to stigmatize against PLHWA due to misconceptions on the mode of HIV transmission. The belief that PLHWA are promiscuous is stronger among young people which may explain the higher stigmatizing attitudes.
Level of education, HIV knowledge and exposure to media campaigns were significant determinants of stigmatization attitudes among the study population. These findings are consistent with other previous studies (Lau and Tsui, 2005; Ezeiru and Odeyemi, 2013). These studies explored the impact of targeted health education on knowledge of HIV and stigmatization practices among market women in Lagos, Nigeria. There was an increase in the proportion of women showing less stigmatizing attitudes towards PLWHA after receiving the intervention. More than half of the intervention group had secondary education or less. This suggests that women with lower levels of education can benefit from educational programmes designed specifically to improve their knowledge and attitude. Our findings also highlighted the contribution of mass media campaigns in increasing HIV knowledge. This corroborates with the findings by Bekalu et al. (2014); that identified the role of mass media and its association to HIV-related stigma, which revealed that mass media publicity decreases the gaps in HIV knowledge that exists in sub-Saharan Africa.
HIV knowledge around transmission, prevention and exposure to mass media campaigns were strongly associated with perceived stigmatization. Similarly, a study in India showed that persons who had received HIV related information through NGOs and those who were aware of prevention and control services in the area were less likely to discriminate against PLWHA (Challen, 2011).
The association between condom awareness/usage and perceived stigmatization has also been previously reported (Challen, 2011). A possible explanation may be that people who use condoms are very cautious about contracting HIV and realize that the virus may be carried by even healthy-looking people.
Certain characteristics such as religion, marital status, alcohol consumption, willingness to test and having multiple sexual partners did not achieve statistical significance for perceived stigmatization. Christianity and Islam when compared with traditional religions did not show any significant relationship with perception of stigmatization. This may be because religious people are more likely to reach out to the downtrodden, the sick and many faiths based organizations have been major partners in HIV control programmes (James et al., 2009). However, this is contrary to the findings of another study in Hong Kong which revealed that religious people are more likely to make value laden judgments about PLWHA (Lau, 2005). This also corroborated with the report by Asonibare (2009) on religious leaders’ perception about PLWHA in Ilorin, Metropolis, Nigeria. It was discovered that perceptions of religious leaders were different based on religious affiliation, age and educational qualifications.
This study also revealed that knowledge of antiretroviral drugs was associated with stigmatization. People who are aware that antiretroviral drugs for PLWHA make them live longer may tend to report less stigmatizing behavior. This was contrary to Ekama’s (2012) study on the pattern and determinants of antiretroviral adherence among Nigerian pregnant women in Lagos State. It was reported that even though maternal desire to protect their unborn child was the greatest adherence motivator for some, majority of these women missed their drugs nor partake in any other HIV-related services because of stigmatization and discrimination associated to being identified as HIV positive. These women had higher tendencies of self-stigmatization and were less aware that antiretroviral drugs help to increase their quality of life (Ekama, 2012).
Stigmatization rates or levels varied among women of reproductive age with less than half reporting low stigma. Low level of education, younger age (15to 24 years of age), poor HIV knowledge, condom use and awareness, as well as antiretroviral drugs and HIV prevention via exposure to media messages were related to perceived stigmatization among women of reproductive age in Nigeria.
This study therefore suggests that in addition to the existing global and national programmes such as Family Life and HIV Education to curb HIV-related stigma, more efforts should be made on reinforcing the effects of stigmatization.
The authors have not declared any conflict of interests.
REFERENCES
|
Adewuya AO and Makanjuola RO (2008). Social distance towards people with mental illness in southwestern Nigeria. Austr. New Zealand J. Psycol. 42(5):389-95.
Crossref
|
|
|
|
Akanbi MA (2010). Socio-Demographic Factors influencing HIV/AIDS stigmatization and Discrimination amongst Women in Lagos State. Afr. J. Gender Behav. 8(2).
Crossref
|
|
|
|
|
Asonibare JB, Durosato IA., et al., (2009). Prevention of HIV/AIDS as perceived by religious leaders in Ilorin, Metropolis, Nigeria. Nigerian J. Guid. Counsel. 14(1).
Crossref
|
|
|
|
|
Bekalu MA, Eggermont S, Ramanadhan S, Viswanath K (2014). Effect of Media Use on HIV-Related Stigma in Sub-Saharan African: A Cross Sectional Study. PLOS one 9(6):1-9.
Crossref
|
|
|
|
|
Bogardus ES (1925). "Measuring Social Distances." J. Appl. Sociol. 9(1925):299-308
|
|
|
|
|
Chellan R, Rajendran P, Charles B (2011). Perceived stigma and discrimination towards PLHAS among young people in Tamil Nadu, India: Evidence from behavior Surveillance Survey. Int. J. Curr. Res. 3(11):421-429.
|
|
|
|
|
Chinwe RN (2007). HIV-Related Knowledge and Social Discrimination in selected Local Government Areas of Lagos State, Nigeria. Presented as a Poster at 5th African Population Conference, Dec. 10-14, 2007 at Arusha, Tanzania.
|
|
|
|
|
Chinwe RN (2005). Social Consequence of HIV/AIDS; Stigma and discrimination in workplace in Nigeria. Paper being presented at the XXV International Population Conference held at Vinci Convention Centre, Tours, France. 18-23.
|
|
|
|
|
Dlamini PS, Kohi TW, Uys LR (2007). Verbal and physical abuse and neglect as manifestations of HIV/AIDS stigma in five African countries. Publ. Health Nurs. 24(5):389-399.
Crossref
|
|
|
|
|
Ekama SO, Herbertson EC, Addeh CV (2012). Pattern and
Crossref
|
|
|
|
|
Emmanuel M, Andrea S, James E (2009). HIV/AIDS-Related Stigma and Discrimination in Nigeria; Review of Research Studies and future directions for Prevention Strategies. Afr. J. Reprod. Health 13(3):21-35.
|
|
|
|
|
Ezeiru SS, Odeyemi KA (2013). Reducing HIV-related stigma among traders in model markets in Lagos, Nigeria through HIV education. J. Community Med. Primary Health Care 24(1,2):34-43.
|
|
|
|
|
James Z, Yvonne Y, Muze J (2009). Religious and HIV in Tanzania; Influence of Religious beliefs on HIV Stigma, disclosure and treatment attitudes. 9(75):1-12.
|
|
|
|
|
Joint United Nation Programme on HIV/AIDS (UNAIDS) (2006). Report on HIV/AIDS Epidemic. UNAIDS 10th anniversary special edition.
|
|
|
|
|
Joint United Nation Programme on HIV/AIDS (UNAIDS) (2014) 'Prevention Gap Report'.
|
|
|
|
|
Joint United Nation Programme on HIV/AIDS (UNAIDS) (2016) 'Prevention Gap Report'.
|
|
|
|
|
Kinsler JJ, Wong MD, Sayles JN (2007). The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care STDS 21(8):584-592.
Crossref
|
|
|
|
|
Kola AO, Ladipo O, Anyanti J (2005). HIV/AIDS Stigmatization in Nigeria.
|
|
|
|
|
Krug EG, Mercy JA, Dahlberg LL, Zwi AB (2006). World report on violence and health. Geneva, World Health Organization, 2002
|
|
|
|
|
Lau JTF, Tsui HY (2005). Discriminatory attitudes towards people living with HIV/AIDS and associated factors: a population based study in the Chinese general population. Sex Transmitted Infections. 81:113-119.
Crossref
|
|
|
|
|
Leclerc-Madlala S (2002). Youth and the importance of sexual culture and context. Social Dynamics. J. Afr. Stud. 28(1):20-41.
|
|
|
|
|
Mahendra VS, Gilborn L, Bharat SB (2007). Understanding and Measuring AIDS related stigma in health care settings: A developing country perspective. J. Soc. Aspects HIV/AIDS. 4(2):616-625.
|
|
|
|
|
Mann J (1987). "Statement at an Informal briefing on AIDS to the 42nd Session of the UN General Assembly, 20 October.
|
|
|
|
|
Mutalewa P, Kisoka W, Ngigo V (2008). Manifestations and reduction strategies of stigma and discrimination on people living with HIV/AIDS in Tanzania. Tanzan J. Health Res. 10(4):220-225.
|
|
|
|
|
Nduonofit, Larry-love E, Ekpenyong (2012). HIV/AIDS stigma and discrimination: challenges, prevention and care. J. Social Sciences And Policy Review. June; 4.
|
|
|
|
|
Nigeria Federal Ministry of Health (2013) "National HIV & AIDS and Reproductive Health Survey 2012, (NARHS Plus II).
|
|
|
|
|
Nigeria's National Agency for the Control of AIDS (NACA, 2015) 'End of Term Desk Review Report of the 2010-2015 National HIV/AIDS Strategic Plan'.
|
|
|
|
|
Nyblade L, Aparna J, Manal B (2013). A brief, standardized tool for measuring HIV-related stigma among health facility staff: results of field testing in China, Dominica, Egypt, Kenya, Puerto Rico and St. Christopher & Nevis. J. Int. AIDS Soc. 16 (3 Suppl. 2).
Crossref
|
|
|
|
|
Ochako R, Ulwodi D, Njagi P (2011). Trends and determinants of Comprehensive HIV/AIDS knowledge among urban youth women in Kenya. AIDS Res. Ther. 8:11
Crossref
|
|
|
|
|
Ogilvie GS, Palepu A, Remple VP (2007). Fertility intentions of women of reproductive age living with HIV in British Columbia, Canada. AIDS 21(1):S83-S88.
Crossref
|
|
|
|
|
Oku AO, Owoaje ET, Ige OK, Oyo-Ita A (2013). Prevalence and determinants of adherence to HAART amongst PLHIV in a tertiary health facility in south-south Nigeria. BMC Infect. Dis. 13:401
Crossref
|
|
|
|
|
Oladapo OT, Daniel OJ, Odusoga OL, Ayoola-Sotubo O (2005). Fertility desires and intentions of HIV-positive patients at a suburban specialist center. J. Natl. Med. Assoc. 97(12):1672-1681.
|
|
|
|
|
Olalekan TK (2012). Relationship between Psycho-demographic Factors and Perceived Stigmatization among People Living with Hiv/Aids in Ibadan, Nigeria. OSR J. Human. Soc. Sci. 5(5).
|
|
|
|
|
Pulerwitz J, Michaelis A, Weiss E, Brown L, Mahendra V (2010). Reducing HIV-related stigma: Lessons learned from Horizons research and programs. Publ. Health Reports 125(2):272-281.
|
|
|
|
|
Rao D, Feldman BJ, Fredericksen RJ (2012). A structural equation model of HIV-related stigma, depressive symptoms, and medication adherence. AIDS Behav. 16(3):711-716.
Crossref
|
|
|
|
|
Rao D, Kekwaletswe TC, Hosek S (2007). Stigma and social barriers to medication adherence with urban youth living with HIV. Psychol. Socio-med. Aspects AIDS/HIV. 19(1):28-33.
|
|
|
|
|
Sophoan T (2013). "Comparison of HIV-Related Knowledge, Attitudes, and Behavior among People Aged 15-49 Years BetweenLesothoand Senegal." Thesis 256, Georgia State University. SPSS Inc., Version 20.0 (SPSS, Chicago IL, USA).
|
|
|
|
|
Stein JA, Li L (2008). "Measuring HIV-related Stigma among Chinese Service Providers: Confirmatory Factor Analysis of a Multidimensional Scale." AIDS Behav. 12(5):789-795.
Crossref
|
|
|
|
|
Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S (2013). A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come?. J. Int. AIDS Soc. 16(3):1-14.
Crossref
|
|
|
|
|
Turan JM, Miller S, Bukusi EA (2008). HIV/AIDS and maternity care in Kenya: how fears of stigma and discrimination affect uptake and provision of labor and delivery services. AIDS Care 20(8):938-945.
Crossref
|
|
|
|
|
United Nations General Assembly Special Session (UNGASS) (2010). UNGASS country progress report. Malawi HIV and AIDS monitoring and evaluation report. 2008-2009.
|
|
|
|
|
Vanden D, Sabue K, Dufour M (2009). Health workers training to promote HIV services for patients with tuberculosis in the Democratic Republic of Congo. Human Res. Health 13:23.
|
|
|
|
|
Wingood GM, Di-Clemente RJ, McCree DH (2007). HIV discrimination and the health of women living with HIV. Women Health. 46(2):99-112.
Crossref
|
|
|
|
|
World Health Organization (WHO) (2006). AIDS epidemic update.
|
|
|
|
|
World Health Organization (WHO) (2006). World report on violence and health. Programme of Action of the International Conference on Population and Development. 3-16.
|
|