ABSTRACT
Worldwide Human Immunodeficiency Virus/Acquired Immune Deficiency syndromes (HIV/AIDS) have created an enormous challenge on the survival of infected patients. Identifying baseline factors that predict morbidity could allow their possible modification in order to improve pediatric HIV care. Retrospective cohort study was conducted in 228 HIV infected children starting antiretroviral treatment at Wolaita zone selected health facilities, Ethiopia. WHO reference population was used to calculate Z- scores for height-for-age, weight-for-height, and weight-for-age. Data were analyzed by bivariate and multivariate analysis using Cox regression proportional hazard model. Survival were calculated and compared with the Kaplan Meier and log rank test. Males account 121(53.1%), mean age was 6.29 years. Mean survival time using Kaplan Meier analysis was 89.3 months (95% CI 85.71-92.97). Incidence of mortality rate 21.02 per 1000 person years of observation (95% CI 12.8-34.3). Overall nutritional status was, 62.5% stunted, 43.0% underweight and 44.7% wasted at baseline. As a result, rural residence AHR 4.30 (95% CI, 1.25-14.8), fair/poor of first three-month ART adherence AHR 8.95(95% CI 2.624-33.72), severely wasted children at baseline AHR 7.040 (95% CI, 1.27-39.13) and age of children were predictors of mortality. Mortality among HIV-infected children was high and strongly associated with malnutrition, residence in rural area, low adherence to ART, and beginning of ART at an advanced age; highlighting the urgent need for targeted interventions including promotion of early initiation and adherence to ART.
Key words: Children, malnutrition, mortality, HIV/AIDS.
Worldwide human immunodeficiency virus/acquired immune deficiency syndrome (HIV /AIDS) have created an enormous challenge on the survival of infected patients. Globally, an estimated 35.3 (32.2–38.8) million people were living with HIV in 2012. Around 9.7 million people in low- and middle-income countries received antiretroviral therapy (ART), representing 61% of all who were eligible under 2010 World Health Organization (WHO) HIV treatment guidelines. From 1996 to 2012, ART averted 6.3 million AIDS-related deaths worldwide, including 5.2 million deaths in low- and middle-income countries (United Nations Program on HIV/AIDS (UNAIDS), 2013).
HIV develops very rapidly among infants and children. Pooled analysis from Africa showed that mortality in infected children was about nine-fold greater than that of uninfected children. They estimated that by 12 months of age, 35.2% of infected children would have died, compared with an estimated 4•9% of uninfected children. At 2 years of age, an estimated 52•5% of` infected and 7•6% of uninfected children would have died (Newell et al., 2004).
Despite children on ART, study in South Africa showed mortality rate of 4.7 deaths per 100 child years on ART (Zanoni et al., 2011). Another study in Asia-pacific showed that during a median follow up of 3.1 years after ART, 6.6% deaths occurred, giving a crude mortality rate of 1.9 per 100 child-years (95% CI, 1.6-2.4) (Lumbiganon et al., 2011).
In Ethiopia, also death rate was calculated to be 4.0 per 100 child-years of observation (Koye et al., 2012). In Addis Ababa, also 8.8% died during a median study follow up of 12 months (Taye et al., 2010).
A number of risk factors contributes to the mortality of these children after starting ART. Some of them are malnutrition status at initiation of ART, lower hemoglobin, age of children,
CD4% at initiation of ART, chronic diarrhea, gender, not receiving cotrimoxazole preventive therapy at baseline and severe immunodeficiency (Zanoni et al., 2011; Lumbiganon et al., 2011; Koye et al., 2012; O'brien et al., 2007; Fenner et al., 2010).
Malnutrition is a common condition in HIV-infected children and one of the predictors of mortality among HIV infected children after initiation of ART except study done in Bahir Dar in which malnutrition has no association with mortality ( Zanoni et al., 2011; Lumbiganon et al., 2011; Taye et al., 2010; O'brien et al., 2007). Study in Addis Ababa, Ethiopia, showed that malnutrition has an impact on survival of HIV infected children after initiation of ART. This study also showed malnutrition prevalence is higher in HIV infected children but this study is done in Addis Ababa which has minimum prevalence of malnutrition in Ethiopia (Fenner et al., 2010; Ethiopian Central Stastical Authority (CSA), 2011).
Ethiopia is one of the highest malnutrition and HIV prevalent areas in the world. According to the Ethiopian Demographic and Health Surveys (EDHS) HIV prevalence ranges from 0.9% in SNNPR and 1.0% in Oromia region to 5.2% in Addis Ababa and 6.5% in Gambella region (Ethiopian Central Stastical Authority (CSA), 2011). The Government of Ethiopia launched fee-based ART in 2003 and frees ART in 2005. During 2011, a total of 333,434 people had ever started ART. There were 249,174 adults (86% of eligible) for a CD4 (cluster of differentiation 4) cutoff less than 200 and 16,000 children currently on treatment (20% of eligible) by the end of 2011 (Ethiopian Federal HIV/AIDS Prevention And Control Office (FHAPCO), 2012). Almost three fourth (64%) of severely malnourished children were found in Oromia and SNNPR (Southern Nation Nationals and Peoples Region) in 20012/2013. Wolaita zone is one of malnutrition and HIV prevalent areas in SNNPR (Federal Democratic Republic of Ethiopia Ministry of Health, 2012/2013).
To have better survival of children after initiation of ART, knowing predictors of mortality is important. Therefore, the aim of this study was assessing predictors that affect the mortality of HIV positive children after initiation of ART.
Study area and period
Study was conducted in Wolaita zone from February 28, 2014 to March 14, 2014.Wolaita zone is found SNNPR and it has 12 woredas and three town administrations. Wolaita Sodo town is administrative town of the zone and 330 km south of the capital city (Addis Ababa). There are 3 hospitals and 68 health centers and 2 non-governmental health centers that render preventive, curative and rehabilitative service for the catchment area population in zone. From these 12 health centers and all hospitals give ART service in Wolaita zone during the study period. Totally 4208 adult patients and 321 children were ever enrolled in ART during the study period. Patients enrolled on HIV care are followed intensively based on national and WHO recommendation.
Study design
Retrospective cohort study was conducted among HIV infected children who had started ART from February, 2006 to March, 2014.
Source population
All children with HIV/AIDS, aged <15 years and started ART treatment in Wolaita zone health facilities were source population.
HIV positive children aged <15 years and at least age should be more than 6 months at initiation of ART and who were on ART at least one full month from February, 2006 to March, 2014 were included. Children HIV patients with incomplete intake form at least with nutritional data, registers and follow up form were excluded.
Sample size
Sample size was determined using a formula for two population proportions and calculated by OpenEpi version 2.3 statistical software package by considering that P1 is percent of exposed (severely underweight) with outcome 17.68% P2 is percent among the non-exposed with outcome 4.83% is estimated from other study (6). Za/2 is taking CL (Confidence Limit) 95%, Zβ 80% power and r is ratio of non-exposed to exposed 1:1. After calculating, sample size was 109 for each total 218. Accordingly, after adding 10% for contingency, a total sample size was 240.
Sampling procedure
Health facilities were selected based on their number of pediatrics ART user. From all 12 health centers, which have given this service we choose 3 which have maximum user which were Bodity, Soddo and Areka health center. From 3 hospitals, which give ART service we choose Wolaita sodo referral hospital and Dubo Sent Marry hospital based on their number of ART user. At the beginning, profiles of all children on ART who have been managed between February, 2006 and March, 2014 in selected health facilities were evaluated. Finally, all individuals ever started ART at that facility were selected.
Dependent variable is survival status from the initiation of ART to March 2014 and main outcome measure is time to survival from the initiation of ART. Independent variables are socio demographic characteristics, base line clinical, laboratory and ART information, anthropometric data (weight, height/length) and ART treatment.
Data collection instrument
Questionnaire consists of the Socio demographic, clinical, laboratory and Anthropometric, ART treatment related and follow up.
Data collection and quality control
Data collection form was developed from ART entry and follow up form used in the ART clinic. Data was collected by reviewing pre-ART register, laboratory request, monthly cohort form, and follow up form, ART intake form and patients’ card. Most recent laboratory result prior to initiation of ART was used as a base line value. In case, there is no pre-treatment laboratory test, results obtained within one month of ART initiation was used. If two results are obtained within a month time the mean was used.
Data was collected by trained ART health officers and nurses at Hospital and health center. Two days long training was given for 1supervisor and 5 data collectors. Overall activity was controlled by principal investigator of study. Data quality was assured through designing a proper data collection material and through continuous supervision. All completed data collection form was examined for completeness and consistency during data management, storage and analysis. Data was entered and cleaned by principal investigator respectively before analysis.
Operational definitions
Drop out: If a patient discontinued ART for at least three month as recorded by ART physician.
Fair adherence: If percentage of missed dose is between 85 and 94%(3-5 doses of 30 doses or 3-9 dose of 60 dose) as documented by ART physician.
Good adherence: If percentage of missed dose is between >95% (<2 doses of 30 doses or <3 dose of 60 dose) as documented by ART physician.
Lost: If a patient discontinued ART for at one to three month as recorded by ART physician.
Poor adherence: If percentage of missed dose is between <85% (> 6 doses of 30 doses or >9 dose of 60 dose) as documented by ART physician
CD4 count normal threshold defined as if CD4 cell count >500 cells/mm3 when the child age is greater than 5 years.
CD4 percentage normal threshold were defined as if CD4 percentage is >35% for <12-month-old child, >30% for children 12-35 months of age, and >25% for 36-59-month child.
Survival: Lack of experience of death
Data entry, analysis and processing
Data were entered, cleaned and edited in Epi-Info 3.5.3 for windows and analyzed using SPSS version 21 for windows to see frequency and predictors. Nutritional status was defined by ENA for SMART software for generating Z score. Cox proportional hazard assumption was checked using STATA 11 by schoenfeld residuals test which P>0.1 assumes fulfill the criteria.
Patient’s cohort characteristics were described in terms of central tendency and dispersion value for and frequency distribution for categorical data. Death was confirmed by reviewing death certificates, medical registration in the hospital, or registration by ART adherence supporter through calling using the registered phone number. Individuals alive on ART, lost follow up and transfer out at the end of the study period was censored. Finally, the outcome of each subject was dichotomized into censored or death.
Univariate analysis was used to describe patient’s baseline characteristics. Actuarial table was used to estimate survival after initiation of ART, and log rank test was used to compare survival curves. Cox proportional-hazard regression was used to calculate the bivariate and adjusted hazard ratio and then determine independent predictors of time to death.
In multivariate cox regression analysis, only those variables that were significantly associated with survival on a crude analysis were entered to the final model.
Ethical consideration
This research was approved by the Research and Ethics Committee (REC) of the School of Public Health, College of Health Sciences of Addis Ababa University (AAU) Ethiopia. Official letter of co-operation was written to the concerned bodies by the School of Public Health AAU. As the study was conducted through review of medical records, the individual patients were not subjected to any harm as far as the confidentiality is kept. No personal identifiers were collected and analyzed. Patient’s record/information were anonymized and de-identified prior to analysis.
Cohort baseline characteristics
Of the 260 children’s records reviewed, 228 were included in the final analysis the rest were not fulfil the inclusion criteria. Above half were males 121(53.1%), rest 107 (46.9%) were females. Median age 6 years ((Inter Quartile Range) IQR = 3-9), and mean age was 6.29 years. From the cohort 158 (69.3%) were urban in residence. Children parent status were 104 (45.6%) both alive, 45(19.7%) were both dead at baseline (Table 1).
Baseline clinical and laboratory baseline characteristics
Majority (91.2%) of the HIV positive children were had at least one history of past opportunistic illness at the initiation of ART. Leading opportunistic illness were Pneumonia 62(29.8%), unexplained persistent diarrhea (>=14 day) 59(28.3%) and unexplained persistent fever (>=30days) 51(24.52%). Functional status of children at baseline 202(88.6%) were working or ambulatory. Above half of 163(71.5%), children developmental status was appropriate for their age. At baseline majority 90(39.5%) were WHO classified as clinical stage II. Fifty-nine percent (135) of children CD4 count or percentage were below normal threshold at baseline. Majority 151 (66.2%) had hemoglobin level of >10 gm/dl at baseline the rest were ≤ 10 gm/dl at baseline.
From 150(65.8%) screened for pulmonary TB (Tuberculosis) based on tuberculin skin test 44(29.33%) were positive and 45(30%) of them were took TB treatment. Eighty percent were taking Cotrimoxazole prophylaxis before initiation of ART and 31(13.6%) were taken INH (Isonaizide) prophylaxis. Majority 90(39.5%) were eligible for ART based onCD4 count or percentage cutoff points. For 86.0% of children first Three-month ART adherence was good. From all 12% of children experience at least minor type of drug side effect like 59.25% was nausea, 25.92% were diarrhea and others (Table 2).
From all 24% of children were change their regimen during follow up due to new TB 29.09%, drug out stock 29.09% and drug side effect or toxicity 21.8%. The commonest regimen were 4a = d4t-3TC-NVP which is 59.2% (Table 2).
Baseline nutritional characteristics
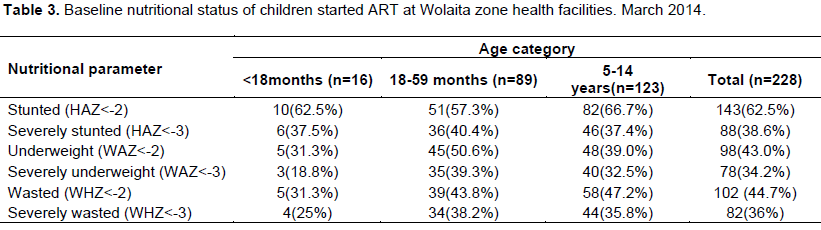
Based on weight for height Z score, nutritional status of this historical cohort at base line was 83(41.9%,95% CI, 35.3 - 48.9) had global malnutrition of these 50.5% were males and 31.9% were females respectively. Prevalence of moderate malnutrition based on weight for height Z score was 13.1% (95% CI 9.1-18.5), with sex distribution of 18.7% (95% CI 12.4-27.1%), and 6.6% (95% CI 3.1-13.6%) for males and females respectively. Prevalence of severe malnutrition was 36% with 43 % in males, 28% in females. Overall nutritional status, 143(62.5%) stunted, 98(43.0%) underweight and 102(44.7%) were wasted at baseline (Table 3).
Survival time
Mean follow up duration was 40.05 months; minimum and maximum follow up time was 1 and 97 months respectively. Mean survival time using Kaplan Meier analysis was 89.3 months (95% CI 85.7-92.9). No median was found (Figure 1). Further analysis of mean survival time was done using socio demographic, nutritional and clinical and laboratory characteristics. Mean survival time had significant difference between urban and rural with log rank test X2 = 9.07 df = 1 p<0.003. Mean survival time had difference across age of children. Mean survival time did not show a difference
across sex of children with log rank test X2 = 1.083 df = 1 p = 0.298. Mean survival time has also difference across severely wasted children stratified by age of the children. Mean survival time among severely wasted HIV infected aged <18 months children on ART was 16 (95% CI, 1-39) compared to non-severely wasted children with mean 80(95% CI 70-89.3 months).
Predictors of mortality
Cumulative incidence of mortality rate 21.02 per 1000 PYO (Person Year of Observation) (95% CI 12.8-34.3 per 1000 PYO). Estimated mortality was 2, 3, 6, 8 and 16% at 6, 12, 24, 60 and 96 months of follow up respectively. Incidences of mortality rate for severely wasted children 3.79 (95% CI 1.3-10.9) times higher than non-severely wasted children.
Relationship between main variable and risk of death was analyzed using Cox proportional model. Result has shown children age, residence, WHO clinical stage III and IV, functional status, developmental status at base line, first three-month ART adherence, hemoglobin value (< = 10 gm/dl), severely underweight, wasted and severely wasted children has significant association on Hazard rate of death (HZ). The rest has no significant association with mortality status.
In multivariate Cox regression analysis, only those variables significantly associated with survival on bi-variate were entered to the final model. After adjusted, independent significant predictor of mortality in children living with HIV/AIDS after initiation of ART remain residence of children, age of children, first three-month ART adherence and severely wasted. Residence of children is predictor of mortality of children on ART living in rural AHR 4.302 (95% CI, 1.25-14.8) than urban children. Children aged < 18 months were less likely to survive than aged 18 to 59 month, 5 to 14 years of age with AHR 0.047(95% CI, 0.006-0.368), 0.145(95% CI 0.032-0.663) respectively. Fair/poor of first three-month ART adherence of children was not surviving as good adherence with AHR 8.95(95% CI 2.624-33.72). Severely wasted at baseline was important predictor of mortality in HIV/AIDS infected children after initiation of ART with AHR 7.040 (95 % CI, 1.267-39.13) (Table 4).
Overall nutritional status, 62.5% were stunted, 38.6% were severely stunted, 43.0% were underweight, 34.2% were severely underweight and 44.7% were wasted and 36% were severely malnutrition at baseline. There was high prevalence of severely wasted, underweight and stunted which was in line with finding of study done in Zewditu memorial hospital that indicated with 61.1% underweight children, 55.6% stunting of children, 27.3% wasting of children at base line were (5,6,). The finding of this study also has similar result with finding in Tanzania (Sunguya et al., 2011). This could be due to substantial impact of HIV infection on the nutritional status of infected people due to poor food intake as a result of poor appetite and difficulty eating, intestinal mal-absorption because of chronic diarrhea and HIV caused intestinal cell damages, metabolic changes and increased nutrient requirements related to opportunistic infections (OIs).
In our study the cumulative incidence of mortality rate, cumulative proportion of survival and mean survival time for this cohort using Kaplan Meier analysis was lower in our study compared with study done in 2006 by Medicines Sans Frontie`res HIV/AIDS programs in 14 countries, the overall probability of survival (O'brien et al., 2007). Our finding also had lower mortality rate compared study done in Ethiopia in AA zewditu and Bahir Dar (Koye et al., 2012; Taye et al., 2010; Atnafu and Wencheko, 2012). This could be explained in two ways. Firstly, the difference in the study period as there were changes in the treatment and care of children on ART through time. Secondly our study includes health centers which give ART service so health centers have most of simple cases as severe cases were refer to hospital.
After adjusted by multivariate Cox proportional regression, the independent significant predictor of reduced surviving in children living with HIV/AIDS after initiation of ART remain residence of the children, age of the children, first three-month ART adherence and severely wasted.
Residence of children is one of the predictor of reducing survival of children on ART living in rural four times higher than urban children. This is similar with EDHS 2011 shows Mortality rates in urban areas are consistently lower than in rural areas in child mortality. This could be due to hygiene and sanitation, malnutrition is prevalent in rural, poor knowledge of on care of HIV and others (Federal Democratic Republic of Ethiopia Ministry of Health, 2012/2013).
In our study the only socio demographic predictor for survival was children age as < 18 months were more not surviving than age 18 month-5 year, 5 to 14 years of age. This is in line with study done in South Africa shows age of <3 years 2.6 times higher to die than the others (Zanoni et al., 2011). Our study also in line with study done in south Africa from this study age comparing ≥120 months with <18 months were risk factor for death (Fenner et al., 2010). Study done in Malawi also in line with our result Children <18 months old were 2.15 times more likely to die as children aged at least 18 months (Fetzer et al., 2009). Our study also support WHO new 2013 guideline which says ART should be initiated in all children infected with HIV below five years of age, regardless of WHO clinical stage or CD4 cell count (World Health Organization (WHO), 2013).
But our result is not congruent with result from Ethiopia done in Bahir Dar Felege Hiwot referral hospital and AA zewditu memorial Hospital. These studies end that age is not the predictor in the multivariate cox regression. This could be due WHO guideline change for ART initiation that uses age as starting for ART.
However, sex and other socio demographic characteristic were not predictors of mortality in in our study and another study from Ethiopia (Koye et al., 2012; Taye et al., 2010).
In our study fair/poor of the first three-month ART adherence of children was not surviving as good adherence with 8 times higher. According to WHO Retaining people receiving ART in care and ensuring good treatment adherence are critical determinants of successful ART outcomes. Our finding is similar with finding from British Non-adherence over time (<95%) was strongly associated with higher risk of mortality (AHR: 3.13; 95% CI: 1.95 to 5.05). This was also in line with study in Uganda which was good adherence reduces the hazard rate adherence to HAART was associated with survival (HR 0.46, 95% CI 0.47 to 0.50) (World Health Organization (WHO), 2013a, b; Abaasa et al., 2008; Lima et al., 2009). Due to fair/poor adherence of the ART leads to virologic, immunologic and clinical failure that is mediated mainly by two potentially reinforcing mechanisms. Fair/poor adherence to ART leads to failure to suppress viral replication, thus increasing the likelihood of developing HIV mutations that could lead to the development of drug-resistant viral strains. Secondly, fair/poor adherence to ART fails to prevent further viral destruction of the cellular immune system with consequent reduction in the level of CD4+ cells and development of opportunistic infections (Maggiolo et al., 2007).
Severely wasted children at baseline were seven times higher to die early than not severely wasted children with which is consistent with study done in AA Zewditu memorial Hospital, but in study done in Bahir Dar nutritional predictors were not associated with survival (Koye et al., 2012; Taye et al., 2010; Atnafu and Wencheko, 2012). Households of HIV-positive children under ART had lower economic status, less education, and greater proportions of unemployed caregivers. Despite the effectiveness of ART in ameliorating disease burdens, persistent socio-economic backwardness may ultimately retard the progress (Fetzer et al., 2009). The mechanism malnutrition might act to decrease survival is uncertain: The hypothesized reason is malnutrition impair immune reconstitution and there by prolong the period at which patient remain at increased risk of opportunistic infection.
However, in contrary to another study presence of OIs, WHO clinical stage, hemoglobin level, absolute CD4 value, Cotrimoxazole preventive therapy at baseline and delayed or regressing developmental history were significant predictors of mortality but not in our study (Koye et al., 2012; Taye et al., 2010). This could be explained by the study there are high missing value for example for hemoglobin and absolute CD4 value were have number of missing value and missing value analysis was done for these variables.
Limitation of the study was using secondary data with incomplete data and excluding these incomplete data might cause selection bias. A second limitation is computing risk of death which may overestimate the predictors due to inability of controlling competing risk of death as well as underestimated mortality that might be lost to follow up patient. Other limitations such as important predictors of mortality, viral load and micronutrient deficiency were not considered.
Children on ART at baseline have high prevalence of malnutrition. Incidence of mortality for children infected with HIV and initiated ART was lower in this cohort. Malnutrition due to severe wastage was an important predictor of reducing survival of children on ART. Other independent predictors of mortality or survival reduction were residence, age of the child, and first three-month ART adherence registered by physician at baseline.
Based on the study finding, the following recommendations to researchers, hospitals and health centers can be forwarded. The first one is careful monitoring and follow up of patients with who came from rural, age less than 18 months are necessary particularly during the first 6 months of ART initiation. The second recommendation is malnutrition as severely wasted children on ART at baseline should be carefully assessed and treated accordingly and seeks special follow up. Last is about Careful follow up for poorly or fairly adhered patients and giving them drug counseling is crucial to improve survival. Further study is recommended on prospective by controlling such as viral load and micronutrient deficiency.
The authors have not declared any conflict of interests.
REFERENCES
|
Abaasa AM, Todd J, Ekoru K, Kalyango JN, Levin J, Odeke E, Karamagi CA (2008). Good adherence to HAART and improved survival in a community HIV/AIDS treatment and care programme: the experience of The AIDS Support Organization (TASO), Kampala, Uganda. BMC Health Serv. Res. 8(1):241.
Crossref
|
|
|
|
Atnafu H, Wencheko E (2012). Factors affecting the survival of HIV-infected children after ART initiation in Bahir-Dar, Ethiopia. Ethiop. J. Health Dev. 26(3):193-199.
|
|
|
|
Ethiopian Central Stastical Autority (CSA) (2011). Ethiopian demographic and health survey(EDHS).
|
|
|
|
Ethiopian Fedral HIV/AIDS prevention and control office (FHAPCO)(2012). Contry progress report on HIV/aids response.
|
|
|
|
Federal Democratic Republic of Ethiopia Ministry of Health (2012/2013). Health sectore development programme IV performance report.
|
|
|
|
Fenner L, Brinkhof MW, Keiser O, Weigel R, Cornell M, Moultrie H, Prozesky H, Technau K, Eley B, Vaz P (2010). Early mortality and loss to follow-up in HIV-infected children starting antiretroviral therapy in Southern Africa. J. Acquir. Immune Defic. Syndr. 54(5):524.
Crossref
|
|
|
|
Fetzer BC, Hosseinipour MC, Kamthuzi P, Hyde L, Bramson B, Jobarteh K, Torjesen K, Miller WC, Hoffman I, Kazembe P, Mwansambo C (2009). Predictors for mortality and loss to followâ€up among children receiving antiâ€retroviral therapy in Lilongwe, Malawi. Trop. Med. Int. Health 14(8):862-869.
Crossref
|
|
|
|
Koye DN, Ayele TA, Zeleke BM (2012). Predictors of mortality among children on Antiretroviral Therapy at a referral hospital, Northwest Ethiopia: a retrospective follow up study. BMC Pediatr. 12(1):161.
Crossref
|
|
|
|
Lima VD, Harrigan R, Bangsberg DR, Hogg RS, Gross R, Yip B, Montaner JS (2009). The combined effect of modern highly active antiretroviral therapy regimens and adherence on mortality over time. J. Acquir. Immune Defic. Syndr. 50(5):529.
Crossref
|
|
|
|
Lumbiganon P, Kariminia A, Aurpibul L, Hansudewechakul R, Puthanakit T, Kurniati N, Kumarasamy N, Chokephaibulkit K, Nik Yusoff NK, Vonthanak S, Moy FS, Razali KA, Nallusamy R, Sohn AH (2011). Survival of HIV-infected children: A cohort study from the Asia- Pacific region. J. Acquir. Immune Defic. Syndr. 56(4):365-71.
Crossref
|
|
|
|
Maggiolo F, Airoldi M, Kleinloog HD, Callegaro A, Ravasio V, Arici C, Bombana E, Suter F (2007). Effect of adherence to HAART on virologic outcome and on the selection of resistance-conferring mutations in NNRTI-or PI-treated patients. HIV Clin. Trials 8(5):282-292.
Crossref
|
|
|
|
Newell ML, Coovadia H, Cortina-Borja M, Rollins N, Gaillard P, Dabis F (2004). Mortality of infected and uninfected infants born to HIV-infected mothers in Africa: a pooled analysis. Lancet 364:1236-1243.
Crossref
|
|
|
|
O'brien DP, Sauvageot D, Olson D, Schaeffer M, Humblet P, Pudjades M, Ellman T, Zachariah R, Szumilin E, Arnould L, Read T (2007). Treatment outcomes stratified by baseline immunological status among young children receiving nonnucleoside reverse-transcriptase inhibitor–based antiretroviral therapy in resource-limited settings. Clin. Infect. Dis. 44(9):1245-1248.
Crossref
|
|
|
|
Sunguya BF, Poudel KC, Otsuka K, Yasuoka J, Mlunde LB, Urassa DP, Mkopi NP, Jimba M (2011). Undernutrition among HIV-positive children in Dar es Salaam, Tanzania: antiretroviral therapy alone is not enough. BMC Public Health 11(1):869.
Crossref
|
|
|
|
Taye B, Shiferaw S, Enquselassie F (2010). The impact of malnutrition in survival of HIV infected children after initiation of antiretroviral treatment (ART). Ethiop. Med. J. 48(1):1-10.
|
|
|
|
United Nations Program on HIV/AIDS(UNAIDS)(2013). Glaobal Report on Global AIDS epidemics.
|
|
|
|
World Health Organization (WHO) (2013a). Consolidated guidelines on the use of antiretroviral drugs for treating AND preventing HIV infection recommendations for a public health approach Report.
|
|
|
|
World Health Organization report (WHO) (2013b). United Nations International Children's Emergency Fund (UNICEF), Joint United Nations Programme on HIV and AIDS (UNAIDS) (2013). Global update on hiv treatment 2013: results, impact and opportunities.
|
|
|
|
Zanoni BC, Phungula T, Zanoni HM, France H, Feeney ME (2011). Risk factors associated with increased mortality among HIV infected children initiating antiretroviral therapy (ART) in South Africa. PloS one 6(7):e22706.
Crossref
|