Worldwide, 780 million people do not have access to improved drinking water supplies and 88% of deaths from diarrheal diseases are attributable to unsafe water, inadequate sanitation, and insufficient hygiene. Access to safe water and practice of low cost home based treatments are generally at lower level in people living with human immunodeficiency virus (HIV) in Ethiopia. The aim of this study was to assess the water handling and treatment practice of peoples living with HIV in Southern Ethiopia. A cross sectional descriptive study was carried out among 414 study participants in February 2016 at Arba Minch town, Southern Ethiopia. The study participants were selected randomly from all the associations found in Arba Minch town who have HIV/acquired immunodeficiency syndromes (AIDS) infected people with proportional allocation to sample size. Data was collected using structured questionnaire and prepared checklists by trained data collectors. After checking for the completeness and consistency, the data were entered into Epi Info Version 7 software. Finally, descriptive analysis was done using SPSS Version 21 software, and the results were presented and discussed. The majority of clients 403 (97.6%) reported their drinking water source is tap water. Most households 382 (92.5%) had covered their stored water. Most of the respondents practiced pouring method to withdraw water from the stored container. The water status served for the clients showed that 84.5% (349) of households have improved water status. Majority (83.9%) of the households had access to water within a distance of up to 200 m or less. The majority (82.4%) of households had access to water within a time of 30 min or less. About 56% of the households treated drinking water at home. The water handling practice of the participants is not as recommended, and much effort is needed to alleviate this problem.
Worldwide, 780 million people do not have access to improved drinking water supplies and an estimated 2.5 billion people, half of the developing world, lack access to adequate sanitation. Every year, diarrheal diseases kill 801,000 young children, more children than acquired immunodeficiency syndrome (AIDS), malaria, and measles combined, making diarrheal disease the second leading cause of death among children under five. Eighty-eight percent of deaths from diarrheal diseases are attributable to unsafe water, inadequate sanitation, and insufficient hygiene (Center for Disease Control (CDC), 2013).
Africa is one of the two major regions with the least improvement in accomplishing the Millennium Development Goals on sanitation by 2015. Sub-Saharan Africa has a startling 30% coverage with only a 4% increase from 1990. This is a serious concern because of the associated massive health burden as many people who lack basic sanitation engage in unsanitary activities like open defecation, solid waste disposal and wastewater disposal. Africa as a whole, especially sub-Saharan Africa despite efforts and approaches to extend and sustain water, sanitation and hygiene (WASH) systems and services has led to different health complications leading to death within the region. 115 people in Africa die every hour from diseases linked to poor sanitation, poor hygiene and contaminated water (United Nations Department of Economic and Social Affairs (UNDESA), 2014).
Water should be stored in clean, covered containers and kept in a cool dark place. Wide-necked containers such as a bucket fitted with a tight fitting lid are the best as they are easy to clean between uses. Contamination can also occur as the water is taken out of the storage container. Hands and utensils may come into contact with the water so it is important to encourage users to wash their hands with soap before handling drinking water; and to fit a tap to the storage container so that water can be poured directly into a cup or bowl (World Health Organization (WHO), 2016).
Good access to safe water and sanitation is indispensable for people living with human immunodeficiency virus (HIV)/AIDS and for the provision of home-based care to AIDS patients. Water is needed for bathing patients and washing soiled clothing and linen. Safe drinking water is necessary for taking medicines. Nearby latrines are necessary for weak patients. Finally, water is needed to keep the house environment and latrine clean in order to reduce the risk of opportunistic infections. Water and sanitation provision increases the sense of dignity of both patients and caregivers. In addition, safe drinking water is needed for taking medicines and to make food easier to eat for the patients suffering from mouth ulcers or thrush and for excellent hygiene to prevent opportunistic infections. Despite these changing needs, however, access to water, sanitation and hygiene may in fact become more difficult for households caring for Peoples Living with HIV (PLHIV) due to declining physical health, worsening economic status and/or stigma (USAID, 2007).
In resource-limited settings, household-based water treatment and storage methods are recommended for PLHIV and their households. Contaminated water, lack of sanitation, and poor hygienic practices in homes of PLHIV increase the risk of diarrhea, which can result in increased viral load, decreased CD4 counts, and reduced absorption of nutrients and Anti-Retrovirals (ARVs). Ninety percent of people living with HIV are affected by diarrhea, the major cause of morbidity and mortality especially sub-Saharan Africa, where access to safe water and adequate sanitation is most limited (Boschi-Pinto et al., 2008; Lule et al., 2005; Thom and Forrest, 2006; World Health Organization (WHO), 2008).
Current WHO guidelines for drinking-water quality support efforts to ensure safe collection, treatment and storage of drinking water. These safe water interventions should be implemented not only where supplies are absent but also where community supplies are known to be contaminated or are causing waterborne diseases. Point-of-use water, personal hygiene, and sanitation interventions have been found to be cost beneficial (Hutton and Haller, 2004; Obimbo et al., 2004; WHO, 2004, 2008). Household water treatment (treatment that happens at the point of water collection or use, rather than at a large, centralized location) improves water quality and reduces diarrheal disease in developing countries (Center for Disease Control (CDC), 2013).
In Ethiopia up to 60% of the disease burden is attributable to poor sanitation where 15% of total deaths are from diarrhea, mainly among the large population of children under five. In each year, about 250,000 children die accordingly (Federal Democratic Republic of Ethiopia Ministry Of Health, 2005).
A study conducted among rural communities of Dire Dawa Ethiopia revealed that majority of the respondents were found to collect water from springs and wells each accounting for 140 (36.5%), while 104 (27%) will collect water from tap. Fifty seven percent of participants fetch water for more than 60 min. In addition to this, 90 (70.3%) of the households were not aware of the need to protect the water sources before use and 38 (29.7%) of the respondents protected the water sources before use (Amenu et al., 2013).
Not much attention is given to water safety, handling and treatment practices of peoples living with HIV especially in developing countries like Ethiopia. Therefore, this study aimed to assess the water handling and home based treatment practices of PLHIV.
Study area and study period
The study was conducted in Arba Minch town. Arba Minch is the capital city of Gamo Gofa Zone, located in approximately 505 km to the South of Addis Ababa and 275 km away from the Regional capital, Awassa. In Arba Minch town, there are two associations for HIV infected people with different numbers of members. The study was conducted in February 2016 at Arba Minch town, Southern Ethiopia.
Study design
A descriptive community based, cross-sectional study design was implemented.
Population
The source population for the study were all HIV infected people who are member of the associations in Arba Minch town. Those HIV infected people who were randomly selected were the study population. All HIV infected people who are member of the associations and permanent residents were included in the study, and participants who were mentally incompetent, critical ill, and less than 15 years of age during data collection period were excluded.
Sample size
A sample size of 414 was calculated using single proportion population formula of Epi Info Version 7 to assess the water handling practice of PLHIV. The assumptions were considering 95% confidence level (Z=1.96), 5% margin of error, 42.9% proportion of water, sanitation and hygiene (WASH) practice (
14), and to minimize errors arising from the likelihood of non-compliance 10% of the sample size was added.
Sampling procedures
All associations found in Arba Minch town who have HIV/AIDS infected people members were taken. Then samples were allocated proportional to size from each association in the town. Simple random sampling technique was employed using random table to select the study subjects.
Data collection methods
A structured questionnaire and observational checklist was developed to collect information on the households’ socio-economic, environmental conditions and behavioral aspects. The questionnaires were first prepared in English and then translated to Amharic (local language) and again back to English to ensure its consistency.
The trained data collectors interviewed the selected study participants. Moreover, an observational checklist was filled by direct observation to collect complementary information on the characteristics of the home water handling practices. During data collection, if the participant was not available at the time of the first visit, the data collectors had made another visit to that household, the next day.
Six diploma environmental health professionals were recruited as data collectors who have a long experience in data collection was involved in the data collection process. Four days training was given to the data collectors and supervisors prior to the start of the data collection process by the principal investigator(s).
A training manual was also prepared to facilitate the training process. The training was mainly focused on interviewing techniques, and emphasis was also given for questions that need careful attention and observation. Classroom lectures, mock interviews and field practice were included in the training.
Two trained masters of public health professional supervised the survey. The supervisors were responsible for supervising the data collectors; check for the completed questionnaire; and correct any mistake or problem encountered. The principal investigators coordinated the overall data collection process.
Data quality
To ensure reliable information, the questionnaire, check lists and interview guides were developed after reviewing relevant literatures of the subject to include all the possible variables that will address the objective of the study. All tools were first prepare in English and then translated to Amharic and back translated to English to maintain the consistency of the contents of the instrument.
A pretest was done in 5% of the total sample size. Vague terms, phrases and questions identified during the pretest were modified and changed. Missing responses like "No response" and "Others" were added, and skipping patterns were also corrected.
The completed data collection tools were checked every day during data collection for completeness, clarity and consistency by the supervisors/principal investigator. Any mistake detected was corrected the next day. Five percent of the respondents were re-interviewed by the supervisors/principal investigators to check for the consistency of data collection and corrections were made at the spot.
Data management and analysis
Data was coded, stored in a proper area, and kept confidential. Then it was entered into a prepared Epi info template. The data was exported to SPSS version 21 for cleaning and analysis. The data was cleaned by running simple frequency and cross tabulation to check for completeness and consistency, and sorting to identify outliers.
Descriptive measurements (Frequencies, proportions and measures of central tendency) were done to assess the socio-demographic characteristics and the water handling practices of the study participants.
Ethical considerations
Ethical clearance was obtained from the Institutional Review Board of Arba Minch University. Permission was asked from the organizations and Arba Minch city administration office. The questions from the questionnaire were approved and deemed not to affect the morale and personality of study subjects. Informed written consent was obtained from each study subject after explanation and any involvement was done after his or her complete consent. Confidentiality was ensured from all data collectors and principal investigator’s side via the use of code numbers t and keeping questionnaires in a safe secure location. Data collectors interviewed people privately; separately from others to keep the privacy of the clients.
Socio demographic characteristics
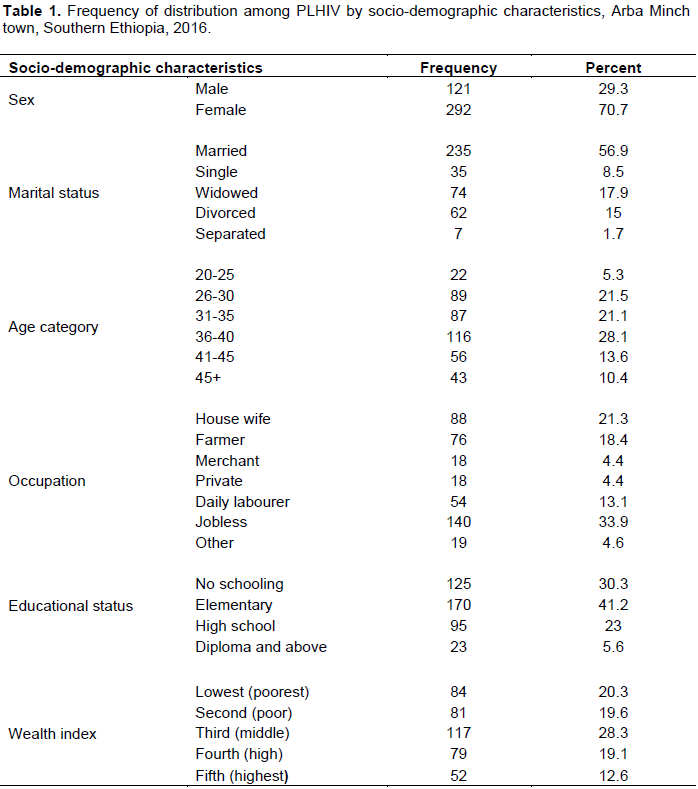
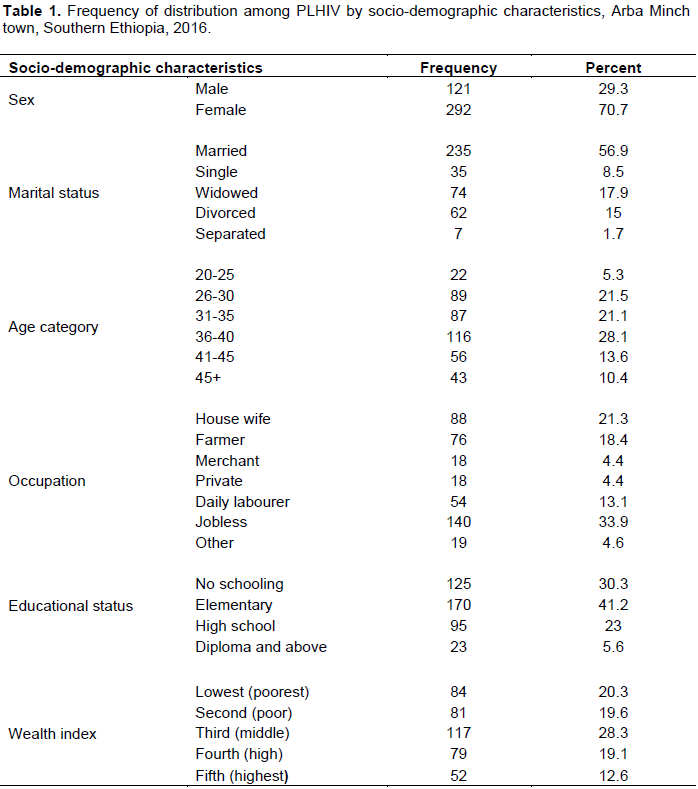
This study was conducted among 413 study participants yielding a response rate of 97.6%. The mean (±standard deviation [SD]) age of respondents was 37.14 ±7.74 years. About 71% of the participants were females. Of the total 413 participants, 116 (28.1%) were in the age group of 36 to 40 years (Table 1).
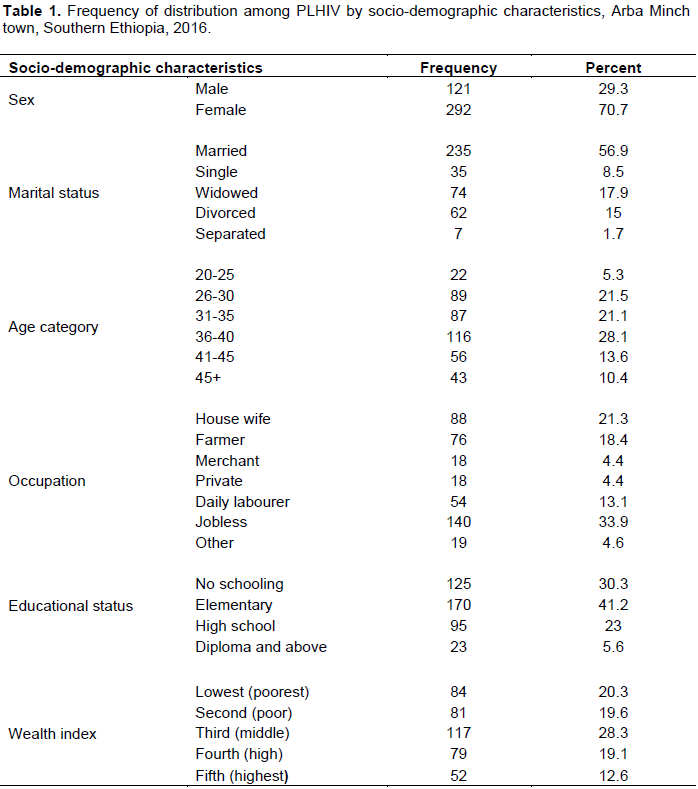
Regarding the marital status of the study participants, 235 (56.9%) respondents were married. The majority of the respondents 237 (57.4%) belong to the Gamo ethnic group followed by Welayta (13.8%), Amhara (12.1%) and others (Gofa, Oromo, Tigre, Konso and Kembata).
Concerning the occupational status of the study participants, most 140 (33.9%) were jobless followed by housewives 88 (21.3%), farmers 76 (18.4%) and daily laborers 54 (13.1%). About 170 (41.2%) respondents had attended formal education from elementary, 125 (30.3%) were illiterate. The income distribution of the study participants was assessed using various parameters of the respondents and their households. Then, wealth index was calculated using factor analysis in five categories. Accordingly, the poorest/lowest, second, third/middle, fourth/high and richest/highest quintile accounted for 20.3, 19.6, 28.3, 19.1 and 12.6%, respectively.
Status of water supply
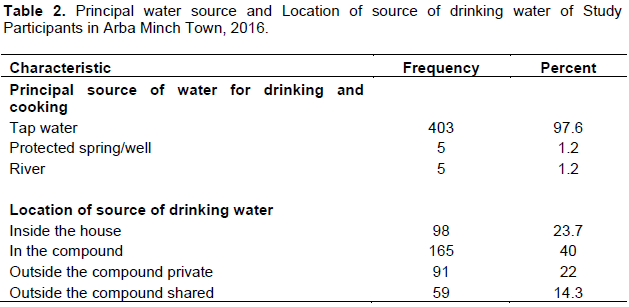
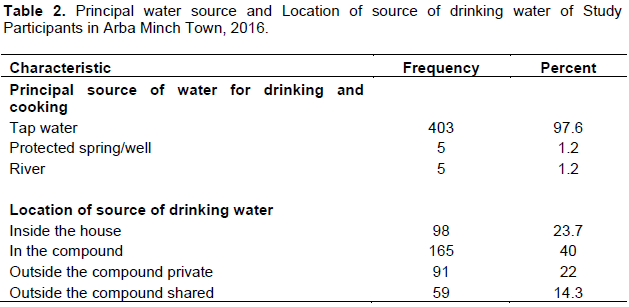
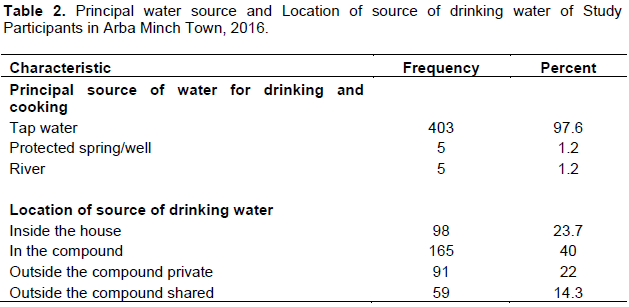
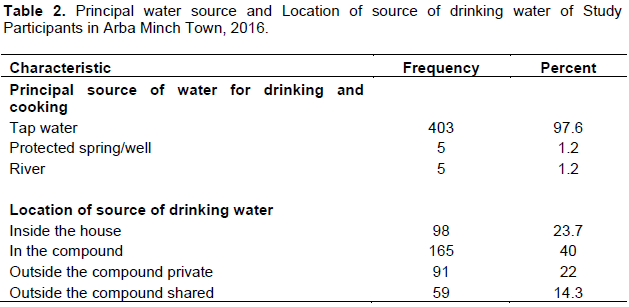
The majority of clients 403 (97.6%) reported their drinking water source is tap water. Only a small number of clients
(1.2%) get their water from a protected well/spring or river. According to this study, 40% of the drinking water source is located within their compound (Table 2).
Water and sanitation to people were affected and living with HIV/AIDS were some of the shortcomings reported in South Africa (Potgieter et al., 2007). In India, economic constraints, lack of individual household toilets, lack of fuel for boiling water, and water scarcity were problems for PLHIV (Seremet et al., 2010). Studies conducted in Zambia and Malawi revealed that PLHIV used different sources and travel long distance to fetch drinking water; only 54 and 53% of clients fetch water from improved sources and walk at least 40 and 25.33 min, respectively (Kangamba et al., 2006; Lockwood et al., 2006). Another study conducted in Botswana on access to safe water for HIV/AIDS patients showed that people use several sources of water and the unreliability leads to use of poor quality water and poor hygiene (Ngwenya and Kgathi, 2006).
Similarly, study done in Ethiopia indicated that the majority of clients 211 (71.8%) reported their drinking water source location as outside their yards in the neighborhood. Only a small number of clients, that is, 0.7% (2), 1% (30), and 0.7% (2) households get their water from protected well, spring and unprotected spring, respectively (Yallew et al., 2012). In other research conducted in Ethiopia, it was reported that one third of the respondents were discriminated in the water source and forced to go far distance to fetch water for their families (Tibebu et al., 2007).
Water storage practice
A good number of participants responded that they stored their drinking water in containers. The majority 386 (93.5%) had used plastic containers, followed by tin containers (6.5%). The data collectors observed whether the household water container was covered or not. Accordingly, the observation revealed that most households 382 (92.5%) had covered their stored water and the rest 31 (7.5%) had not covered. The major type of primary vessel volumes in the households was 20 L (95%). Other households reported tanker, 5 and 2.5 L as primary vessel containers. The type of neck of the primary vessels were narrow, covered, necked, and opened accounting 40.2, 35.1, 23 and 1.7%, respectively.
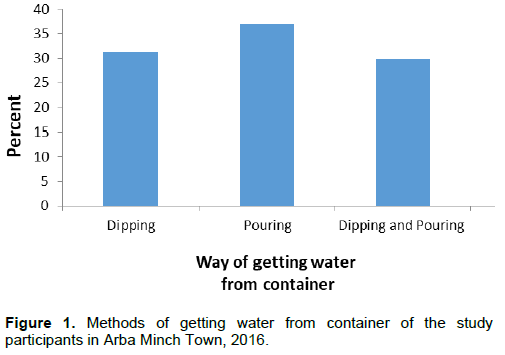
Most of the respondents practiced pouring method to withdraw water from the stored container, while 129 (31.2%) practiced dipping and 123 (29.8%) using both dipping and pouring methods (Figure 1). In general water status served for the clients showed that 84.5% (349) of households have improved and 14.5% (64) of the clients have unimproved water status.
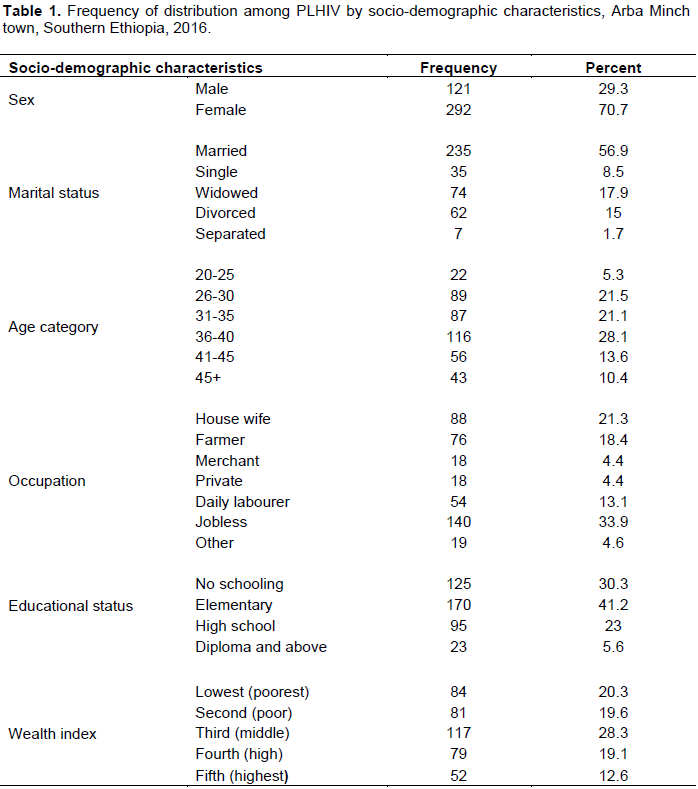
Regarding the marital status of the study participants, 235 (56.9%) respondents were married. The majority of the respondents 237 (57.4%) belong to the Gamo ethnic group followed by Welayta (13.8%), Amhara (12.1%) and others (Gofa, Oromo, Tigre, Konso and Kembata).
Concerning the occupational status of the study participants, most 140 (33.9%) were jobless followed by housewives 88 (21.3%), farmers 76 (18.4%) and daily laborers 54 (13.1%). About 170 (41.2%) respondents had attended formal education from elementary, 125 (30.3%) were illiterate. The income distribution of the study participants was assessed using various parameters of the respondents and their households. Then, wealth index was calculated using factor analysis in five categories. Accordingly, the poorest/lowest, second, third/middle, fourth/high and richest/highest quintile accounted for 20.3, 19.6, 28.3, 19.1 and 12.6%, respectively.
Status of water supply
The majority of clients 403 (97.6%) reported their drinking water source is tap water. Only a small number of clients (1.2%) get their water from a protected well/spring or river. According to this study, 40% of the drinking water source is located within their compound (Table 2).
Water and sanitation to people were affected and living with HIV/AIDS were some of the shortcomings reported in South Africa (Potgieter et al., 2007). In India, economic constraints, lack of individual household toilets, lack of fuel for boiling water, and water scarcity were problems for PLHIV (Seremet et al., 2010). Studies conducted in Zambia and Malawi revealed that PLHIV used different sources and travel long distance to fetch drinking water; only 54 and 53% of clients fetch water from improved sources and walk at least 40 and 25.33 min, respectively (Kangamba et al., 2006; Lockwood et al., 2006). Another study conducted in Botswana on access to safe water for HIV/AIDS patients showed that people use several sources of water and the unreliability leads to use of poor quality water and poor hygiene (Ngwenya and Kgathi, 2006).
Similarly, study done in Ethiopia indicated that the majority of clients 211 (71.8%) reported their drinking water source location as outside their yards in the neighborhood. Only a small number of clients, that is, 0.7% (2), 1% (30), and 0.7% (2) households get their water from protected well, spring and unprotected spring, respectively (Yallew et al., 2012). In other research conducted in Ethiopia, it was reported that one third of the respondents were discriminated in the water source and forced to go far distance to fetch water for their families (Tibebu et al., 2007).
Water storage practice
A good number of participants responded that they stored their drinking water in containers. The majority 386 (93.5%) had used plastic containers, followed by tin containers (6.5%). The data collectors observed whether the household water container was covered or not. Accordingly, the observation revealed that most households 382 (92.5%) had covered their stored water and the rest 31 (7.5%) had not covered. The major type of primary vessel volumes in the households was 20 L (95%). Other households reported tanker, 5 and 2.5 L as primary vessel containers. The type of neck of the primary vessels were narrow, covered, necked, and opened accounting 40.2, 35.1, 23 and 1.7%, respectively.
Most of the respondents practiced pouring method to withdraw water from the stored container, while 129 (31.2%) practiced dipping and 123 (29.8%) using both dipping and pouring methods (Figure 1). In general water status served for the clients showed that 84.5% (349) of households have improved and 14.5% (64) of the clients have unimproved water status.
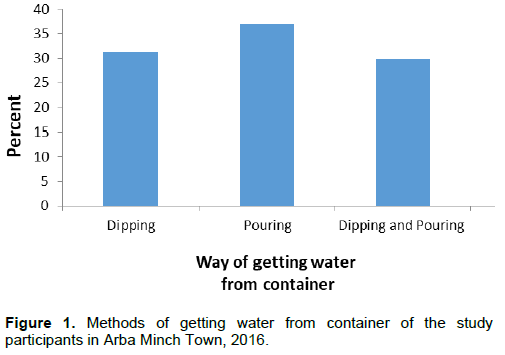
Although storing of water in covered containers and the use of proper procedures to pour water ensures the water is not re-contaminated, different studies in different areas documented malpractices. A study conducted in Zambia reported that only 55% used vessels having a narrow neck for storage and 12% reported dipping from the container (Kangamba et al., 2006). A similar study in Malawi also showed that 26.7% used narrow neck while the majority (83.3%) reported dipping a coup into the storage (Lockwood et al., 2006). But a study done in Ethiopia indicated that majority of the clients (80.3%) practiced pouring method to withdraw water from the stored container while (7.1%) practiced dipping (Yallew et al., 2012).
Water collection and consumption
The containers differ in sizes but range from 20 L buckets to 40 L containers. Mostly, 20 L jerry cans are used for fetching water 391 (94.7%). With respect to distance of water source from dwelling, majority (83.9%) of the households had access to water within a distance of up to 200 m or less. In addition, the majority (82.4%) of households had access to water within a time of 30 minor less. Fifty seven percent of participants fetch water for more than 60 min according to a study done on Eastern Ethiopia (Amenu et al., 2013). The variation might be due to difference in geographical location and time of study. A study carried out in Malawi on assessment of water, sanitation, and hygiene in the context of Home-Based Care for Peoples Living with HIV indicated that long distances to water sources in the rural areas created barriers to accessing water for households affected by HIV (Lockwood et al., 2006).
In the majority of households 328 (79.7%), an adult woman usually collected drinking water from water sources followed by both adults 35 (8.5%), adult men 28 (6.8%) and under 18 years females 21 (5.1%).
Regarding consumption of water, the majority of households (93.7%) had used less than 20 L per capita per day and of which 55.8% households had used less than 15 L per capita per day. This is in contrary to a case study conducted in Botswana, which revealed that home based care HIV/AIDS patients used additionally 20 to 80 L of water for care from the normal water supply, and also the water consumption was increased from 40 l to 100 L (Ngwenya and Kgathi, 2006). This variation could be attributed due to economic problems and/or insufficient amount of water availability in the household (Yallew et al., 2012).
Home based water treatment
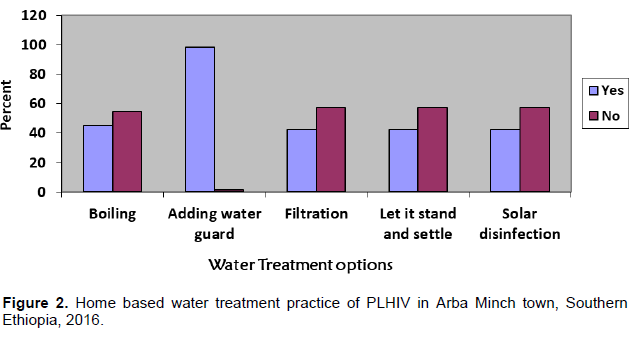
More than one-third (67.6%) of the respondents think that the water they drink is safe directly from its source, however, 104 (25%) participants responded “I do not know”. Only 7.4% (30) of respondents do not think that the water they drink is safe directly from its source. Moreover, 233 (56.4%) households treated drinking water at home, but the rest 176 (42.6%) did not treat water at home. A study from Northern Ethiopia showed that only 12% households treated water at home and 82.7% of them believed that the water they used was always clean and safe (Sharma et al., 2013).
Among the households who treated their drinking water within 24 h at home, about 98.5% mostly used a water guard. Filtration, settlement, solar disinfection and boiling were also the other water treatment methods used by the households at home (Figure 2). Some studies showed that the use of household treatment or at point of use thereby reduces the risk of diarrheal disease by 30 to 40% (Lule et al., 2005; Wanyiri et al., 2013). Sharma et al. (2013) reported only 7.8, 3, and 1.5% households practiced simple sedimentation, boiling and filtration methods, respectively to treat water at home before consuming water (Sharma et al., 2013). Studies done in Zambia and Malawi revealed that respondents used chlorine and boiling to treat their drinking water in the previous 24 h (Kangamba et al., 2006; Lockwood et al., 2006). A study done in Gondar city also showed that people living with HIV practice treating water in home using chlorination, boiling and filtration (Yallew et al., 2012).