ABSTRACT
The focus of the study is to gather data on the current effects of COVID-19 on healthcare practice, medical and pre-medical educational experiences, and permanent implications. This was completed by analyzing data from novel COVID-19 and related studies. The results of the study can show the lasting impact of COVID-19 on medical education and the healthcare field. To reduce exposure and possible disease transmission, many physicians have turned to telemedicine as a way to provide for patients without direct contact. Whether this is a permanent or temporary method of consulting with patients is yet to be determined. Medical and pre-medical educational experiences have also been deeply affected by the pandemic. The pandemic caused medical schools to start limiting students’ patient contact hours and postponed their spring exams, possibly delaying student graduation or residency placement. Pre-medical students are currently unable to participate in many of the activities that are strongly suggested by medical schools as key components to a successful application. Currently, shadowing and other clinical experiences are prohibited in most of the United States, and volunteering opportunities have been extremely limited. Permanent implications of COVID-19 on hospital systems, medical education, and pre-medical experiences are still to be determined. It will take multiple application cycles and cohorts of studies to determine the permanent implications of COVID-19 on the healthcare system, and medical and pre-medical experiences.
Key words: COVID-19, ETHAN, hospitals, medical education, pre-medical education, telemedicine.
COVID-19 is having a great effect on healthcare and medical education starting from the beginning of 2020, leaving providers and students alike lost in its wake. Named for the crown-like spikes on its surface (Yang et al., 2020).COVID-19 is a member of the beta-coronavirus family of viral diseases along with MERS, SARS, and SARS-CoV (Wu et al., 2020). Collectively, these are enveloped, positive-sense, single-stranded RNA viruses that have rapid mutation and recombination rates (Chan et al., 2020). The COVID-19 virus is said to have
originated from a wet market in Wuhan, China, and is transmitted via aerosol and close personal contact (Chan et al., 2020; Yang et al., 2020). Since the outbreak, many have been concerned about the virus mutating in order to gain other susceptible forms of transmission, though none are documented to date.
COVID-19 at the moment is known to attack the upper respiratory tract, with less abrupt onset of symptoms than previous coronaviruses (Heymann and Shindo, 2020). It has also known that individuals can pass on the virus to others without presenting any symptoms (Chan et al., 2020). So far, COVID-19 has presented differently in patients and there have not been any common trends between patients of similar demographic backgrounds (Chan et al., 2020). Generally, symptoms begin to appear after an incubation period of around five days (Rio and Malani, 2020; Rothan and Byrareddy, 2020). The most common symptoms are fever, fatigue, and a dry cough (Yang et al., 2020). Those at the highest risk are of older age, have compromised immune systems or other comorbidities, or live in close-quartered facilities (Heymann and Shindo, 2020; Yang et al., 2020; Zhou et al., 2020).
The high rate of spread of COVID-19 has prompted researchers to work towards developing rapid test kits and presently working on a possible vaccine. Rapid diagnostic tests are using nucleic acid detection with fluorescent PCR, and nucleic acid sequencing to detect if the positive-sense RNA strands of the virus are present, for a positive diagnosis (Yang et al., 2020). Hydroxychloroquine and azithromycin have also been two big names in recent media coverage of COVID-19. In a study to determine the efficacy of the two drugs, a combination treatment of hydroxychloroquine and azithromycin cured all patients of COVID-19 nasopharyngeal carriage only 6 days after the start of treatment, compared to 57.1% of hydroxychloroquine-only treated patients and 12.5% of control patients (Gautret et al., 2020). Researchers have targeted hydroxychloroquine to pair with azithromycin because of its increased potency and safety, compared to other chloroquine derivatives (Yao et al., 2020). However, a clinical observational study designed to test the efficacy of hydroxychloroquine reported a negative effect as a first line of COVID-19 treatment (Mehra et al., 2020). There were also potentially high levels of cardiotoxicity reported in patients being treated with hydroxychloroquine. The study found a correlation between patients treated with hydroxychloroquine and an increased frequency of ventricular arrythmias in these patients (Mehra et al., 2020) leading the World Health Organization to stop hydroxychloroquine testing and issue a health warning. Current clinical trials are looking to target the S protein on the surface to interfere with binding, which will lead to neutralization of the virus (Amanat and Krammer, 2020). A list of ongoing clinical trials for COVID-19 vaccinations can be found in the United States National Library of Medicine (https://clinicaltrials.gov/ct2/results?cond=covid-19&cntry=US&Search=Apply&age_v=&gndr=&type=&rslt=).
The information presented in this study shows the urgent need for governing bodies of the medical field to come together to enact focused plans that will preserve our healthcare system and medical education. Presently, medical education has been moved online until further notice, which can have permanent implication as some institutions may see it fit to keep their students’ pre-clinical educational years online. Without the need to see patients in-person, faculty at medical institutions can permanently teach their students in a virtual format. If executed, it can affect how institutions declare student residency for tuition, if they allow students to reside in other states or countries, and the possibility of increased collaboration between institutions’ students as well. Moreover, pre-medical students now have the opportunity to fulfill their healthcare experiences virtually, which opens the door to more development in virtual healthcare exposure.
CURRENT IMPLICATIONS OF COVID-19
Healthcare
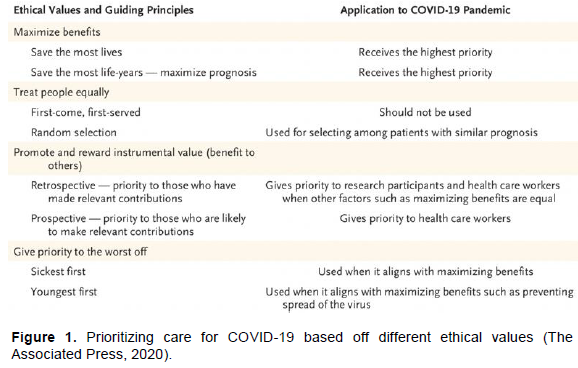
In the United States and around the world, the COVID-19 pandemic has caused an alarmingly large number of patients to exceed the capacity of our hospitals, especially intensive care units (ICUs) (https://www.usnews.com/news/best-states/alabama/articles/2020-04-26/doctors-struggle-to-pay-bills-telemedicine-isnt-helping). Because of CDC recommendations and quarantine laws established by different governments, personal protective equipment (PPE) and ventilators have also been hard to access and to mass-produce safely. Hospital systems and physicians are being faced with extremely difficult decisions regarding who deserves priority care in the midst of limited resources. Figure 1 shows the different justifications healthcare providers might use when it comes to prioritizing their treatment (https://www.usnews.com/news/best-states/alabama/articles/2020-04-26/doctors-struggle-to-pay-bills-telemedicine-isnt-helping). Those who were fortunate to be admitted to hospitals are not able to have family members visit for risk of further transmission. Italy’s chronic shortage of healthcare workings has led to overwhelmingly long hours on their physicians (Paterlini, 2020), a representation of what has also happened in “hot spots” of the United States. For many hospital systems, non-urgent care and elective surgeries started being postponed indefinitely in March (Brindle and Gawande, 2020; Spinelli and Pellino, 2020).
There has been an increased use of telemedicine in the United States. The University of California, San Francisco, has mandated that for palliative and ambulatory care they will strictly use telemedicine to treat (Calton et al., 2020). To allow for physicians to treat as many patients as they can during this crisis, regulations on normal physician-patient contact have relaxed to fit the needs of telemedicine: patients can now receive care across state lines, Medicaid programs allow for telemedicine reimbursement without federal permission, certain HIPAA regulations will not be enforced until the pandemic as subsided, and physicians can waive cost-sharing for virtual appointments without penalty (Amanat and Krammer, 2020; Calton et al., 2020). The age of telemedicine has also led to forward triaging, a way to sort patients before they enter the emergency department. Forward triaging allows for efficient, self-isolated triaging before patients expose healthcare workers and other patients to their conditions (Hollander and Carr, 2020; https://clinicaltrials.gov/ct2/results?cond=covid-19&cntry=US&Search=Apply&age_v=&gndr=&type=&rslt=). This also enables centralized coordination between large healthcare systems and their outpatient and testing centers (Hollander and Carr, 2020; https://clinicaltrials.gov/ct2/results?cond=covid-19&cntry=US&Search=Apply&age_v=&gndr=&type=&rslt=). There are current United States healthcare systems already using forward triaging, and it could be something for more to look to as a method of reducing contact. Telemedicine also provides rapid access to specialist consultations (Hollander and Carr, 2020).
One problem with virtual consultations, as with telemedicine in general, is physician compensation. The compensatory system used in the United States does not cover virtual appointments in all cases, and this can create a void in physician payment. Compensation for a virtual appointment is a fraction of what it is for an in-person appointment, too. A rheumatologist in Alabama received $12 from Medicare for a 40-min phone appointment, which is the same coverage he would receive for a 10-min office appointment (The Associated Press, 2020). At the rate physicians are being compensated for virtual appointments many small practices will be out of business, adding to the already overwhelming shortage of physicians in the United States. Most small practices are in rural and underprivileged areas, meaning there will be a decrease in the availability of physicians for these communities which further deepens their medical deficiencies. There is also the problem of whether or not physicians will want to use telemedicine as a main source of consulting with patients. Patients may struggle to feel as though their voice is heard over virtual appointments, and physician-patient relationships will suffer (Brindle and Gawande, 2020).
Medical education
The years spent in medical school are formative for young, upcoming physicians. It is supposed to be their time to explore different specialties and research interests. Due to COVID-19, students can no longer meet for class or in group settings (Rose, 2020). Many hospitals in the United Kingdom and United States have suspended clinical rotations and electives because they fear students will transmit the virus across hospitals (Rose, 2020; https://takecasper.com/about-casper/). Furthermore, the Association of American Medical Colleges (AAMC) supported medical schools postponing clinical rotations through at least the second half of March, with rotations being voluntary thereafter (Gautret et al., 2020). For the last two months, patient contact has been strictly voluntary for all medical students in the United States, per the AAMC’s April 14th recommendation (https://students-residents.aamc.org/applying-medical-school/article/covid-19-changes-mcat-exam-administrations-may-29-/). This loss of clinical exposure and classroom learning experience may potentially lead to difficulties in future residency application and selection. By not having network opportunities or proper exam preparation through clinical rotations, medical students’ professional development is heavily constricted (Ferrel and Ryan, 2020).
Pre-medical education
For many pre-medical students, undergraduate education is a time of discovery and development. Students look to volunteering and shadowing as two primary means of building a base for their medical school applications, and COVID-19 has stopped almost all opportunities. It will be very difficult for younger undergraduate students to gain an appreciation for what the medical field entails, and why they want to go into medicine. Just as important, in-person student organization events have come to a halt as all universities are online through the spring and summer terms. These were how pre-medical students gained invaluable leadership development and it is now a second area future medical school applicants may be lacking proficiency. With spring MCAT exams postponed through May, changes brought to the MCAT exam have forced students to adjust their applications and study schedules as well. For the rest of the 2020 cycle, the AAMC has adjusted the testing format for the MCAT exam so that each test day can include three testing periods; one starting at 6:30 am, one at 12:15 pm, and one at 6:00 pm (https://students-residents.aamc.org/applying-medical-school/article/covid-19-changes-mcat-exam-administrations-may-29-/). By shortening the exam from 7 h and 30 min, to 5 h and 45 min with a shortened mid-exam break (https://students-residents.aamc.org/applying-medical-school/article/covid-19-changes-mcat-exam-administrations-may-29-/) students must adjust the way they prepare for the examto accommodate for differing time limits and questions per section. Many who counted on having a score by applications will now have to consider the options of submitting their application without a score or holding their application until they test and receive a score. There is also the consideration of what COVID-19 has done to the current medical school application pool: are undergraduates still seeing medicine as glamorously as they once have, now with COVID-19 causing extreme hours and risk? Many have pondered on whether or not there will be reduced application numbers over the next few cycles because of the pandemic, and how this will affect the already large shortage of physicians in the United States.
PERMANENT IMPLICATIONS OF COVID-19
Healthcare
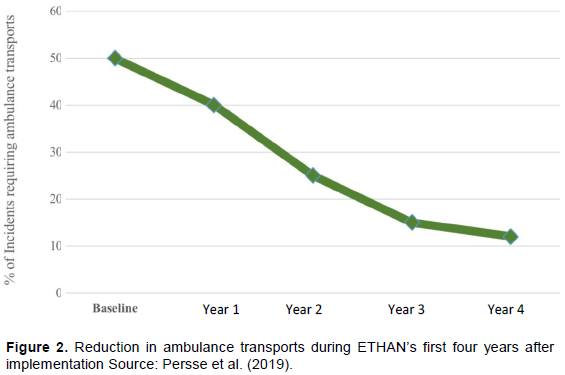
COVID-19 has brought the world of virtual patient care to the forefront of medicine. However, the city of Houston has used an electronic triage system since 2014 in order to reduce ambulatory transports to their emergency departments. The system, called Emergency Telehealth and Navigation (ETHAN) utilizes virtual triaging by emergency room physicians through tablets that emergency medical services carry with them (Langabeer et al., 2016). Physicians are then able to access patient records at the scene and determine if the patient is at a high-enough risk to be transported to the emergency department. If not, emergency services will help the patient setup a follow-up appointment with a primary care physician (Langabeer et al., 2016). This model may be the future of emergency services, specifically in high-density cities like Houston. The ETHAN initiative has reduced emergency department loading for physicians while saving patients the trip to an emergency room, which can run up to $2,500 in the city of Houston (Mantas, 2017). It would allow for physicians to evaluate and prepare for patients prior to arrival, and limit compromised patient exposure to contagious diseases like COVID-19 (Hollander and Carr, 2020). Since its implementation in 2014, there have been drastically fewer emergency visits via ambulance, as well as increased patient savings. A 2019 study shows how, compared to nearly 50% at ETHAN’s implementation, just over 10% of patient incidents required ambulance transport to the emergency department (Figure 2). The ETHAN system can also save patients an average of $223 by taking into account ambulance cost, telehealth cost, physician labor, and EMT labor (Persse et al., 2019). few complications have arisen with ETHAN: compensation for non-emergencies, technological issues, and triage reliability are all areas of concern for healthcare systems before making the switch to a similar model of virtual healthcare (Mantas, 2017). It would not be a surprise to see more permanent attempts at a virtual treatment system, especially for emergency departments in larger cities, to help decrease the exposure of patients and healthcare workers alike to transmissible diseases.
Medical education
For the past few months, medical students have been forced to transition their intensive learning environments to an online format. With ever-increasing desires to have consistent patient contact early, and many medical universities already recording lectures, COVID-19 may be the tipping point that drives future medical school lecture-style learning online. Medical school learning is known as “drinking water from a firehose.” The vast amount of information presented during lectures might make an online format more advantageous: whatever is missed in a lecture can be re-watched to ensure proficient understanding of the material. Moving lecture-style courses online allows more time for students to meet in groups to learn together, take part in research or volunteering interests, and gain valuable hands-on patient care experience as well. This is not to say there are problems with online learning, though, as they have also been witnessed during the pandemic. Moving lectures to a permanent online format would force students to seek help from professors via virtual appointments or during times that are not already blocked off, like in-person lectures. Medical school is also a time to start professional networks and mentorship, and to decrease interpersonal communication may negatively impact students’ development. There are many considerations to take into account as medical schools announce decisions about returning to their respective campuses, or continuing virtual education, for the fall term.
Pre-medical education
As noted earlier, COVID-19 has halted almost all pre-medical student opportunities to shadow, volunteer, and gain other experiences prior to medical school. With increased vigilance in nursing homes and hospitals, pre-medical students may need to go through more intense clearance processes after quarantine to ensure they will not transmit anything to patients. It is possible that undergraduate students will find it difficult to initiate volunteering or shadowing as well. Those in charge of these experiences may be hesitant to open their doors to people that are exposed to a large volume of others, like college students. The pandemic has raised a lot of questions for pre-medical students on how they should be gaining experience in the medical field if they cannot shadow, work, or volunteer. Although students are coming up with creative ways to do so, most will be left with a gap in their experiences because of the virus. We may start to see different approaches by medical schools on how to evaluate the quality and quantity of students’ pre-medical experiences. Some schools are starting to use Situational Judgement Tests (SJTs), such as CASPer, to see if applicants match what the respective schools are looking for. SJTs are psychological tests that present realistic scenarios to test-takers and score responses based on what the individual would do (https://takecasper.com/about-casper/). These types of tests may fill the gaps left by underwhelming experiences during future application cycles. It is difficult to say how the pre-medical experience will look after the pandemic. Will students be allowed to shadow or volunteer in hospitals as they did before COVID-19? Is there the chance that shadowing is moved permanently online, through live feeds in patient rooms or “physician cams,” to remove liability of transmitting diseases to and from students? These are questions pre-medical students are asking themselves to determine what they need to do to gain valuable experience before medical school applications.
It is too early to determine what the permanent implications of COVID-19 are on medical and pre-medical educational experiences, especially because many institutions are unsure of their fall plans. Virtual learning platforms have been established during the spring semester and may continue until further notice. This can establish a norm of pre-clinical education being presented online in the future. Clinical rotations are deemed essential to medical education and will resume under safe conditions. As for pre-medical experiences, many medical schools are now accepting virtual experiences as substantial. Whether or not this will remain as the virus is contained, we do not know. Many hospital systems are adapting telehealth measures to continue treating patients. Once ETHAN’s minor complications have been resolved, this appears to be the pre-hospital system of the future by decreasing physician load and patient costs. Other telehealth measures, such as virtual appointments with primary care physicians and specialty consultations, seem to be less effective than they were before the pandemic. More studies need to be published focusing on how the pandemic has affected diagnostic and consultant accuracy before definitive statements can be made.
The authors have not declared any conflict of interests.
REFERENCES
|
About CASPer. Retrieved May 27, 2020, from
View
|
|
|
|
Amanat F, Krammer F (2020). SARS-CoV-2 Vaccines: Status Report. Immunity 52(4):583-589.
Crossref
|
|
|
|
|
Brindle ME, Gawande A (2020). Managing COVID-19 in Surgical Systems. Annals of Surgery, 1.
Crossref
|
|
|
|
|
Calton B, Abedini N, Fratkin M (2020). Telemedicine in the Time of Coronavirus. Journal of Pain and Symptom Management.
Crossref
|
|
|
|
|
Chan JFW, Yuan S, Kok KH, To KKW, Chu H, Yang J, Yuen KY (2020). A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. The Lancet 395(10223):514-523.
Crossref
|
|
|
|
|
COVID-19 Changes to MCAT Exam Administrations: May 29 - September 28, 2020. (2020, April 24). Retrieved May 27, 2020, from
View
|
|
|
|
|
COVID-19: LCME. Retrieved May 19, 2020, from
View
|
|
|
|
|
The Associated Press (2020). Doctors Struggle to Pay Bills, Telemedicine Isn't Helping. (2020, April 26). Retrieved May 27, 2020, from
View
|
|
|
|
|
Ferrel MN, Ryan JJ (2020). The Impact of COVID-19 on Medical Education. Cureus.
Crossref
|
|
|
|
|
Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, Raoult D (2020). Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. International Journal of Antimicrobial Agents 105949. Available from
Crossref
|
|
|
|
|
Heymann DL, Shindo N (2020). COVID-19: What is next for public health? The Lancet 395(10224):542-545.
Crossref
|
|
|
|
|
Hollander JE, Carr BG (2020). Virtually Perfect? Telemedicine for Covid-19. New England Journal of Medicine 382:1679-1681.
Crossref
|
|
|
|
|
Langabeer J, Gonzalez M, Alqusairi D, Champagne-Langabeer T, Jackson A, Mikhail J, Persse D (2016).Telehealth-Enabled Emergency Medical Services Program Reduces Ambulance Transport to Urban Emergency Departments. Western Journal of Emergency Medicine 17(6):713-720.
Crossref
|
|
|
|
|
Mantas J (2017). Informatics empowers healthcare transformation. Amsterdam: IOS Press.
|
|
|
|
|
Mehra MR, Desai SS, Ruschitzka F, Patel AN (2020). Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis. The Lancet.
Crossref
|
|
|
|
|
Paterlini M (2020). On the front lines of coronavirus: the Italian response to covid-19. BMJ 368:m1065.
Crossref
|
|
|
|
|
Persse DE, Gonzalez M, Langabeer J, Champagne-Langabeer T, Gleisberg GR (2019, September 6). Tele-EMS Improves Productivity and Reduces Overall Costs. Retrieved June 18, 2020, from
View
|
|
|
|
|
Rio CD, Malani PN (2020). COVID-19-New Insights on a Rapidly Changing Epidemic. Jama 323(14).
Crossref
|
|
|
|
|
Rose S (2020). Medical Student Education in the Time of COVID-19. Jama.
Crossref
|
|
|
|
|
Rothan HA, Byrareddy SN (2020). The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity, 109.
View
Crossref
|
|
|
|
|
Spinelli A, Pellino G (2020). COVID-19 pandemic: Perspectives on an unfolding crisis. British Journal of Surgery.
Crossref
|
|
|
|
|
Wu A, Peng Y, Huang B, Ding X, Wang X, Niu P, Jiang T (2020). Genome Composition and Divergence of the Novel Coronavirus (2019-nCoV) Originating in China. Cell Host and Microbe 27(3):325-328.
Crossref
|
|
|
|
|
Yang Y, Peng F, Wang R, Guan K, Jiang T, Xu G, Chang C (2020). The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. Journal of Autoimmunity 109:102434.
Crossref
|
|
|
|
|
Yao X, Ye F, Zhang M, Cui C, Huang B, Niu P, Liu D (2020). In Vitro Antiviral Activity and Projection of Optimized Dosing Design of Hydroxychloroquine for the Treatment of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Clinical Infectious Diseases.
Crossref
|
|
|
|
|
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Cao B (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. The Lancet 395(10229): 1054-1062.
Crossref
|
|