ABSTRACT
Integrated community case management (ICCM) is a program that allowed Health Extension Workers (HEWs) treat the three most common childhood illnesses: pneumonia, diarrhea and malaria through delivering a closer and accessible care. In Ethiopia, this proven strategy was being implemented in selected districts of the regions but there were no sufficient evidences to decision-makers for improvement interventions. Cross-sectional study was conducted by including all functional health posts and HEWs from four randomly selected districts. Pre-tested structured questionnaires and observation checklist were used to collect data. Data was entered into Epi data version.3.1 and transported to SPSS v.21.0 for analysis. Bivariate and multiple binary logistic regression analysis were used to identify the determinants. 60 (60.6%) of the Health post were in good implementation category. 24 (15.3%) had only one HEW each, 26.8% had recommended three HEWs and 16 (16.2%) had no. HEWs mentored quarterly had three times better implementation (AOR) 3.14, 95% CI [1.65-6.52]). The services were less likely implemented in kebelles lacking any CHAs (AOR 0.47, 95% CI [0.19-0.83]). Health posts which were serving community for greater than eight hours per day had five times better implementation (AOR 5.33, 95% CI [2.58-9.33]). The study revealed that there is still a long way to go for better implementation of the program. Improving the program implementation needs a coordinated effort of all stakeholders at different levels. Nationally, preparing a system-wide approach towards resolving multifaceted challenges facing the programs will help attain the sectorial mission of reducing child mortality.
Key words: Integrated community case management, health extension workers, community health agents.
Integrated Community Case Management (ICCM) is a community care strategy which seeks to extend case management of childhood illness beyond health facilities to the community level so that more children have access to lifesaving treatments (Unicef, 2012). It is provided by community health workers at the lowest level health units or in the community during home visits. Delivery of care through community health workers (CHWs) can increase coverage of specific treatments and lead to substantial reductions in child mortality (Unicef, 2012). The ICCM package can differ based on national contexts, but most commonly includes diarrhea, pneumonia and malaria diagnosis and treatment. For these reasons, various NGOs like UNICEF, WHO, USAID and other partners are funding and technically supporting the ICCM strategy to train, supply and supervise front-line workers to treat children for diarrhea, pneumonia and malaria, using Oral Rehydration Salt (ORS) and zinc, oral antibiotics, and artemisin based combination therapy (ACT), respectively. Their target is mainly toward low income and malaria-affected countries (Unicef Ethiopia, 2011). In 2010, 12 countries in sub-Saharan Africa were implementing Community Case Management (CCM) of the three illnesses and only 6 of them implemented in at least 50% of their country's districts (Hamer, 2011). Despite the current admirable accomplishment, progress must be accelerated and sustained to meet the Millennium Development Goal (MDG) 4 deadline in all parts of the world. If the current trends continue, the world will not meet the MDG target until 2026. The 2013 data of WHO shows that sub-Saharan Africa shoulders the world’s highest under-five mortality rates. All 12 countries with under-five mortality rates of 100 or more deaths per 1,000 live births are in sub-Saharan Africa. On average, 1 out of every 11 children born in sub-Saharan Africa dies before age five. This is nearly 15 times the average rate (1 in 159) in high-income countries (Who-Cherg, 2013).
In 2013, about half of global under-five deaths occurred in sub-Saharan Africa and 32% in South Asia. Among the top 26 countries shouldering the burden of 80% of the world’s under-five deaths, 19 are in sub-Saharan Africa (Unicef, 2015). Though annual child deaths from pneumonia decreased by 44% from 2000 to 2013 and from 1.7 million to 940,000; it remained the leading infectious cause of death among children under-five, killing nearly 2,600 children a day (Faijer, 2014). In 2013, it killed about 940,000 children with majority of victims are under two years. Diarrhea next to pneumonia also accounts for 9% of all deaths among children under age 5 worldwide. In 2013, this translated into 1,600 young children dying each day, or about 580,000 children a year, most of them living in South Asia and sub-Saharan Africa (Unicef, 2015). Malaria every day in 2013 killed more than 1,200 children under age 5, a total of over 450,000 children a year. Most of these deaths occurred in sub-Saharan Africa (Unicef, 2015). Ethiopia is one of the 10 countries with the highest numbers of neonatal deaths; it is currently ranked fifth in the world as having the greatest potential to save maternal, perinatal and neonatal lives by 2025. Despite this, global movements like “A Promise Renewed” (APR) has helped galvanize a national response in Ethiopia to address existing challenges and disparities that threaten the lives of children to reach the most vulnerable and marginalized children with vital life-saving interventions, over 205,000 children still do not reach their fifth birthday (APR, WHO, 2014) . Nearly 43% or 88,000 of the 205,000 children under-five are dying each year mostly from preventable or easily treatable diseases in their first 28 days (Bhutta et al., 2009).
In Ethiopia, of the 34,000 female health extension workers trained and deployed to the community, two were assigned to one kebelle of 5000 residents. In 2010, after the national health policy adopted ICCM, its implementation started in selected areas of four regions (Oromia, Amhara, SNNPR and Tigray) and is currently on the stage of preparation for expansion to other areas. According to 2012 Unicef and National Report (FMOH, 2012; Unicef Report, 2012), 11,754 HEWs were trained in ICCM and deployed to 66 of 254 districts. The program allowed HEWs not only to manage pneumonia, diarrhea, malaria, malnutrition, measles, ear infection, and anemia but also provided 6-day training on strengthened supervision, improved supply chain management for essential commodities, and enhanced monitoring and evaluation (FMOH, 2012; Unicef, 2012, 2015). Though Ethiopia has reached MDG target of 68 CMR per 1000 live births in 2012, it should sustain the achievements and shift to global future child mortality reduction target of bringing it down to 20 per 1000 live births. With this, strengthening current tools that fueled the achievements like ICCM through scientific investigation of the constraints and sharing best experiences during scale up helps the country deliver accessible, affordable, and quality service. As Ethiopia, there is no research done on factors hindering the implementation of the program at community or health post level by health extension workers that could help identify major challenges and propose for possible obstacles for further expansion in other parts of the country. Therefore, the objective of the current study was to assess factors affecting the implementation of ICCM at community level in relation to access to service, monitoring and evaluation, reliable supply of ICCM commodities and HEWs related factors. The other possible influencers could be addressed in further studies.
Study area and period
The study was conducted in South West Shoa Zone of Ethiopia, located at 116 km at south west of the capital Addis Ababa from 16/03/2015 to 30/03/2015. It comprises 12 rural districts with a total population of 1,110,011 residing in 268 villages (National Census, 2010). There were two functional hospitals (One non-governmental and one governmental, excluding three under construction) and a total of 54 health centers coordinating 253 health posts under them.
Study design
A cross sectional study design that used a quantitative data collection method was employed.
Source and study population
All ICCM-trained HEWs (157) working, in the four selected districts of the zone were included. The response rate was 96% excluding five (two ill and three on maternity leave) during the study.
Sampling technique
The survey was conducted in four randomly (lottery method) selected districts that had 99 functional health posts and total of 163 health extension workers. All functional health posts and all trained health extension workers (157) were included in the study. Five HEWs were excluded because two were ill and three were on maternity leave during the time of study. The survey instruments were adapted from the WHO Health Facility Survey tool, a survey of Health Surveillance Assistants in Malawi (Chandani, 2014; Luis et al., 2013) and CCM Global Indicators (WHO, 2014). This structured questionnaire was translated into a working language ‘Afaan Oromoo’ and Checklist for availability of ICCM supplies.
Data management and analysis
Eight data collectors who were fluent in Afan Oromo collected the data. Observations of health post were conducted for availability of ICCM supplies by checklist. All sampled health post’s supply record, sick baby registration books, annual plan, past one year ICCM reports and supervision feedback were reviewed. Data was edited, coded and entered into Epinfo data version 3.1 and exported to SPSS 21.0 statistical software for analysis. Descriptive statistics such as mean, median, standard deviation (SD) and percent were used to present the result. Implementation status of ICCM was dichotomized as good for coverage greater than or equal to 35% and poor for lower service coverage. Bivariate binary logistic regression analysis using stepwise elimination approach and variable at p value of less than 0.25 became candidate for multivariate binary logistic regression analysis. Presences of multi-co-linearity were investigated using correlation coefficient between each pair of independent variables and correlated variables were excluded. Conclusions were made using P value < 0.05 and AOR with 95% CI to measure independent effect of factors on the implementation status of ICCM services package. The model was found fit with Hosmer Lemeshow value of 0.71. Data collectors were trained for two days. The tool was pretested in four health post of neighboring district (Saden Soddo) and little omission were made. Ethical clearance was first obtained from College of Health Sciences, Jimma University, Ethics Clearance Committee, Regional, Zonal and Woreda Health Offices.
Variables
The outcome variables of measurement were implementation status of ICCM of childhood illness services (annual percentage coverage). The independent variables were availability and accessibility of services (power and water source, hours of open health posts, number of CHAs per Kebelle, sessions of community sensitization), monitoring and supervision related variables (HEWs mentored onsite, reporting documentation), supply related variables (availability of ICCM drugs and supplies), health extension workers related factors (socio demography of HEWs, place of residence of HEWs, perceived benefit of ICCM, session of meetings HEWs participate per week, irregular working hours).
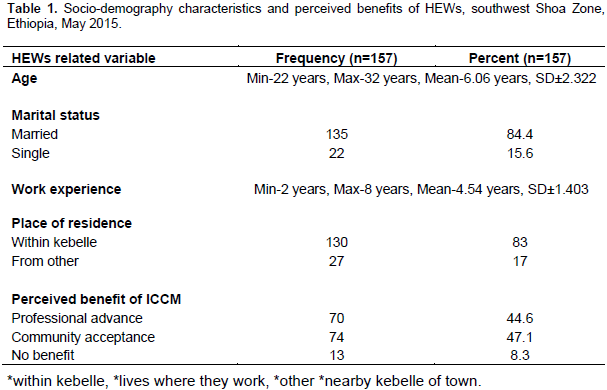
Socio-demographic characteristics of the study participants
A total of 157 health extension workers deployed in 99 health posts from four districts were included in the study. Five HEWs were excluded from 163; because two were ill and three were on maternity leave during the time of study. Total of 99 health posts were visited and assessed for supply and record checklist during an interview. The ages of the respondents ranged from 22 to 32, with a mean age of 26.1 years and SD 2.32. 135 (84.4%) of them were married. The work experience of health extension workers ranged from 2 to 8 years with mean and SD of 4.5 and 1.40 years, respectively. More than 83% of HEWs reside in their respective villages. 44.6% stated that the initiation of the ICCM had increased their acceptance from the community (Table 1). All health extension workers were asked for any motivation or promotions provided to them from either of community and government. For 16 (16.16%) of health posts, the community constructed shelter to live in the kebelle, for 20 (20.2%) the government in collaboration with Woreda health office built the house for them; but 63 (63.6%) had no residential support with some transport from other kebelles. Since recent time (two years), there was 11 (7%) health extension workers turnover from the health posts under study. In regard with educational opportunity, 11 HEWs meaning 7% have got educational opportunity by government from the surveyed health posts.
Service access barriers
In 83 (83.8%) of the total health posts, there were two or more HEWs in each, whereas in 16 (16.2%), there was only a single health extension in each. In addition, only 27 (27.3%) of the health posts had recommended community health army (CHA) of greater than or equal to three persons per kebelles with 26 (26.3%) lacking any assigned CHAs. Concerning infrastructure coverage, 96 (97%) get their water source from protected source (hand pipe 75 (75.8%), pulling wheel 21 (21.2%), and 3 (3%) fetch lake water). Additionally, 17.2% of the total health posts have access to electric power for night time services, while the 82.8% are in use of kerosene or fuel.
Monitoring of ICCM services
The record review result revealed that 66 (66.7%) of health posts had copy of all ICCM reports for the past one year. But amazingly, in all of the available reports, there was no LQAS done. The study reported that 39 (39.4%) of the health posts received supportive supervision on ICCM that included review of registration and observation of case management, while the remaining 60 (60.6%) were not reached by either of the Woreda and Health center ICCM focal persons. Few health extension workers (2.6%) had gone to their catchment health center for professional advices and practical attachment to build their service capacity, while others had no hint for it. All of the health extension workers have participated in review meeting at district level at least twice per the last one year. However, written or documented feedback from their district or health center was found in only 63 (63.6%) of the health posts.
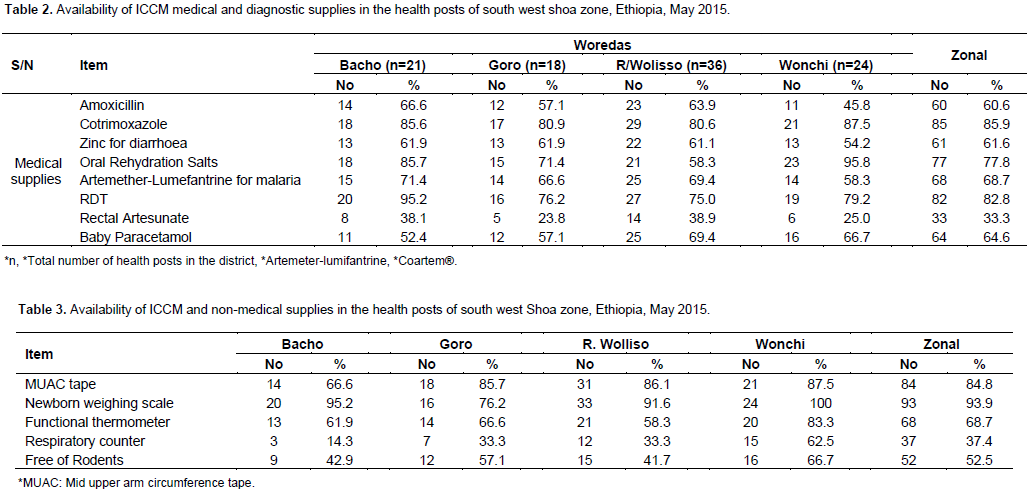
Supply related factors
The supply related factors affecting the implementation of ICCM were identified in three categories as medical and diagnostic supplies, non-medical supplies and storage areas (Table 2). From the overall 99 health posts observed, 87.93% had medical and diagnostic supplies, 52.5% of them had rodent free store house, 60.6% had adequate space of storage and 61.4% had non-medical supplies including stationary, registration books and forms (Table 3). All variables showing significant value to affect implementation status of ICCM service delivery up on bivariate binary logistic regression analysis become candidate for multiple binary logistic regression analysis. Thus, number of community health agents per kebelle, average hours the HEWs work per day, documentation of reports and other files, onsite mentoring of HEWs, and community mobilization meetings were statistically significant upon both bivariate and multiple bivariate logistic regression analysis. Summary of the multivariate binary logistic regression analysis is discussed below (Table 4). Implementation of ICCM services were twice more likely implemented (adjusted odd ratio (AOR) 2.21, 95% CI [1.27-5.41]) in kebelles where communities were mobilized or had meeting for at least once per month than those who had not mobilized. The ICCM service coverage was 48% less likely implemented in kebelles possessing less than the standard three CHAs than those possessing greater than or equal to three CHAs (AOR 0.624, 95% CI [0.114-0.8777]). Kebelles lacking any assigned CHAs 53% less likely implemented the program than those possessing the recommended three per kebelle (AOR 0.47, 95% CI [0.19-0.83]). Health posts which were serving community for greater than 8 h per day had five times implementation of ICCM services than those that only open for customary 8 h per day (AOR 5.33, 95% CI [2.58-9.33]). Health extension workers who were mentored onsite quarterly in the past one year (including register reviews and case observations) three times more likely implemented the services three fold than those who were not mentored in the previous one year (AOR 3.14, 95% CI[1.65-6.52]). Health posts with improper documentation of reports and documents less likely implemented the program (AOR 0.041, 95% CI [0.008-0.216]).
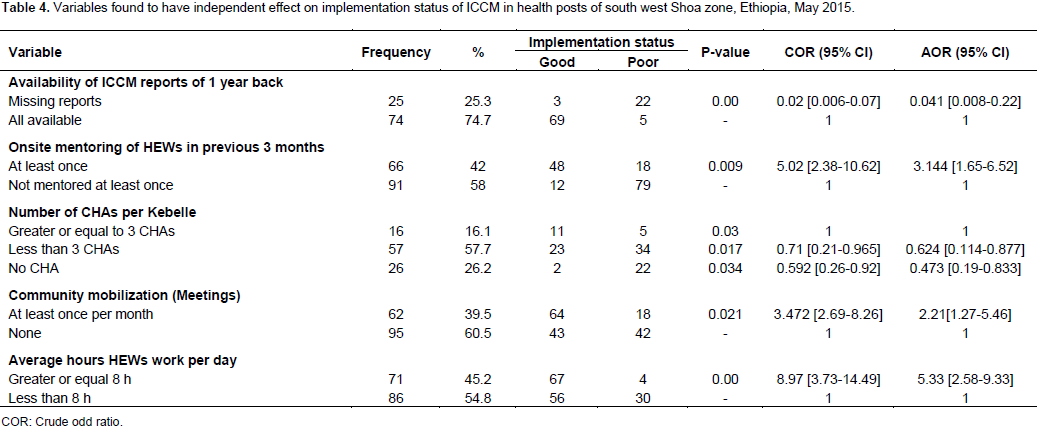
The study brought about two major findings. The first was level of ICCM services implementation in the health posts; where 60.6% (61) of them were above or mean coverage of 35%. It also extracted factors affecting the implementation status of the program in various aspects which were not addressed and never investigated in the study area. The reason is that the survey of the factors affecting implementation of ICCM was not done in any part of the country and consequently the findings were majorly compared with the neighboring countries with similar implementation and service trend findings. Inadequacy of community health agents (CHAs) had a profound effect on implementation status of the program. Currently, minimum of three CHAs are expected per every kebelle as policy guide but only 16.2% of kebelle had three and more CHAs and even 26.3% lacking any CHA in their kebelles. Hence, the lower their number in the community the lesser the community sensitized about the services and lower service coverage. This is consistent with the qualitative study conducted in rural Kenya, which also identified CHWs un-availability in the villages together with low community involvement limited provision of the ICCM services (Simon, 2012). On the other hand, demand generation activities that were measured by session of community mobilization in form of meeting per month had greatly affected the implementation status of the program. Implementation or service coverage were twice more likely higher in kebelles where communities were mobilized for at least once per month. This was also convergent with the study conducted in rural Zambia; which concluded that regular community sensitization was crucial for optimal functioning of ICCM services and health service coverage as a whole (Seidenberg et al., 2012). Additionally, another study conducted in 32 health facilities of Malawi, Mali and Zambia showed that low awareness among the beneficiaries of the service affected the ICCM implementation (Nsona et al., 2012).
This study showed that timely onsite mentoring of health extension workers that included review of registration and observation of case management had greater impact on level of ICCM service coverage. Health posts which received onsite mentoring as per the standard of at least once in a quarter had better implementation of the program which was found significant after multivariate regression analysis (AOR 3.144, 95% CI [1.65-6.52]). The studies done in rural Uganda also found that supervision were less than optimal. Less than 40% of HSAs included in the sample had received an ICCM-specific supervisory visit in the previous 3 months, and only 16% received a visit that included clinical observation of case management (Rutebemberwa et al., 2012). This is almost the same result with this study outcome of 42.04% HEWs mentored, of which only 16.61% were reported as case observation. Health extension workers participated in the study were all trained on the program and working for at least two years. Few health extension workers (2.6%) had gone to their catchment’s health center for professional advices and practical attachment; while others had neither hint for it nor linkage with their health center. Absence of using report quality assessment techniques like lot quality assurance system (LQAS) at health post were also common problem as observed in UNICEF’s 2012 systematic review report of high burden countries including Ethiopia (Unicef, 2012). Consequently, improving quality of reports and feasible program monitoring become complicated. The study showed that majority (87.1%) of the health posts had adequate essential medical supplies though it vary within and among woredas but non-medical supplies was scarce in most of them. In contrast, another study conducted in Malawi reported 47% of CHWs had standard essential ICCM commodities (Health et al., 2014). Storage room was commonly not adequate; there was no separation of commodities and rodents sometimes eat up the supplies. There was limited understanding of forecasting for future demand by HEWs and frequent stock out was common that is linked with untimely requisition of supplies by them and irregular provision of some commodities by health centers and woredas. More than 76% of the health posts receive their supplies from resupply point by their own while others receive through focal persons and commonly assigned professional to the kebelles. The base line study conducted in Rwanda showed that frequent stock out of supplies related with limited capacity of CHWs (Chandani et al., 2011).
Despite the overall coverage, ICCM services in the health posts were above mean of 35%, which reflects there is still long way towards better implementation of the program. Absence of residential house for HEWs in all kebelles minimized the time they spent at health posts to provide services especially to those hard to reach areas. Continuous onsite mentoring of review of registration and observation of case management needs were not accustomed. On the other hand, supervision conducted by health center had no written feedback complicating the follow-up. Inadequacy of standard two HEWs and three CHAs per each kebelle were major obstacle for better functionality of the services and sensitizing community towards the services. Improper documentation of data and absence of monthly assessment of report quality were also tackle of continuous improvement. Unreliable supplies of medical and non-medical supplies were convoluted and forecasting of future demand and safe storage space are underlying cause for service interruption. Improvement of the ICCM services implementation needs utmost intervention and strive of all stakeholders starting from health extension workers to regional and policy makers. Nationally, preparing a system wise approach towards resolving multifaceted challenges facing the health care programs will help attain the sectorial mission.
The authors have not declared any conflict of interests.
The authors would like to thank Jimma University for funding this research. Their gratitude goes to respective district health offices, data collectors, supervisors, and study participants for their cooperation in the study process.
REFERENCES
|
Bhutta AZ, Lassi ZS, Pariyo G, Huicho L (2009). Global Experience of Community Health Workers for Delivery of Health Related Millennium Development Goals.
View
|
|
|
|
Chandani Y, Noel M, Pomeroy A, Andersson S, Pahl MK, Williams T (2012). Factors Affecting Availability of Essential Medicines among Community Health Workers in Ethiopia, Malawi and Rwanda : Solving the Last Mile Puzzle 87(Suppl 5):120-126.
|
|
|
|
Downey S (2011). Community Case Management Overview. UNICEF
|
|
|
|
Hamer DH (2011). Integrated Community Case Management ( iCCM ) in sub-Saharan Africa. (iCCM).
View
|
|
|
|
Health C, Paper W, Division P (2014). Review of Systematic Challenges to the Scale-up of Integrated Community Case Management.(April) UNICEF.
View
|
|
|
|
Nsona H, Mtimuni A, Daelmans B, Callaghan-Koru JA, Gilroy K, Mgalula L, Kachule T (2012). Scaling up integrated community case management of childhood illness: update from Malawi. Am. J. Trop. Med. Hyg. 87(Suppl 5):54-60.
Crossref
|
|
|
|
Rutebemberwa E, Kadobera D, Katureebe S, Kalyango JN, Mworozi E, Pariyo G (2012). Use of Community Health Workers for Management of Malaria and Pneumonia in Urban and Rural Areas in Eastern Uganda. 87(Suppl 5):30-35.
|
|
|
|
United Nations Children Fund (UNICEF) report (2014). Diarrhoea remains a leading killer of young children.
View
|
|
|
|
United Nations Children Fund (UNICEF) (2012). Integrated Community Case Management of Childhood Illness in Ethiopia.
View
|
|
|
|
United Nations Children Fund (UNICEF) (2012). Qualitative study to identify solutions to local barriers to care-seeking and treatment for diarrhoea malaria and pneumonia in select high burden countries Report on findings from Kenya. 5603
View
|
|
|
|
United Nations Children Fund (UNICEF) Report (2015). Committing to Child Survival : A Promise Renewed Progress Report.
View
|
|
|
|
UNICEF Manual I, Guide TU (2011). Integrated Community Case Management ( ICCM ) Costing and Financing Tool Implementation Manual & Tool User Guide, (ICCM).
View
|
|
|
|
United Nations Children Fund (UNICEF) (2014). Trends of death from Malaria in under five children.
View
|
|
|
|
World Health Organization (WHO) (2013). Global Health Estimates Technical Paper WHO/HIS/HSI/GHE/2013.4.
View
|