Full Length Research Paper
ABSTRACT
Orthodontic treatment makes necessary to use a longtime fixed-band appliance, it offers suitable conditions for fungal growth, dentures also allow fungal contamination on their surfaces. The aim of our study is the identification of the fungal species colonizing surfaces of dental appliances, the cross-sectional study was carried out on 60 patients wearing dental appliances, during 5 months, and sterile swabs were used and inoculated into Sabouraud’s dextrose agar tubes. Yeast identification has been based on germ tube test, chlamydoconidia production and biochimical tests (Auxacolor, Api 20 C). The overall prevalence of fungal contamination of dental orthodontic appliance was 35%. The prevalence rate was 40% among patients who had dental appliances for 1 to 2 months, and 45,5% fort patients brushing their teeth at least twice daily, but no statistical relation with mycosis was found. Pain, burning and discomfort were correlated to fungal carriage p=0,038; OR=4,867 IC 95% (1.09-21.74). The fungal species most recovered were Candida parapsilosis 21.47%, Candida Zeylanoides 21.47%, Candida albicans 17.38%, and Cryptococcus terreus 13.04%. Mycological monitoring of dental prosthesis is crucial to prevent possible fungal’s adverse health effects.
Key words: Orthodontic appliances, dentures, fungal contamination, Candida sp, Cryptococcus terreus.
INTRODUCTION
In recent years dental infections and biosecurity attracted greater interest of health professionals due to the spread of infectious diseases such as AIDS and Hepatitis B (Moreira et al., 2016). Oral appliances are divided in prosthodontics and othodontics, ranging from braces and retainers to dental crowns, fillings and dentures.
Denture stomatitis, is a common inflammatory lesion, the erythema is localized to the fitting surface of the denture bearing areas of maxillary removable dental prosthesis (Neville et al., 2009). At one time oral fungal infections were a relatively uncommon event, but with advances in health care and an increasingly aging population, oral fungal infections are becoming more common. Stomatitis appears to be multiparametric; old age and concomitant decline of the immune defences, systemic diseases, smoking, ill-fitting denture and poor oral hygiene resulting in the accumulation of plaque on the dentures have all been proposed as predisposing factors (Barbeau et al., 2003; Grimound et al., 2005; Figueiral et al., 2007). The use of oral appliances is usually asymptomatic; however, it may cause mild soreness or burning sensation.
Fixed orthodontic treatment can lead to alteration in the oral environnement. A study revealed that orthodontic treatment is correlated to an increase in the count of microorganisms, an increased accumulation of plaque, and a decrease in the level of pH, which leads to a major risk of caries and periodontal diseases (Gujar et al., 2020). Orthodontic treatment leads to significant changes in both supragingival and subgingival microbial flora showed that there was an increase in the level of subgingival pathogens after the placement of orthodontic appliances (Gujar et al., 2020).
Numerous fungi are potentially pathogenic microorganisms, Candida albicans is the principal species associated with human infections ranging from the more common oral thrush to fatal systemic superinfections in patients who are afflicted with other diseases (Krishnan, 2012). Besides Candida sp, other fungi can cause oral diseases in humans: Aspergillus, Cryptococcus, Histoplasma capsulatum, Blastomyces dermatitidis, Zygomycetes class, Coccidioides immitis, Paracoccidioides brasiliensis, Penicillium marneffei, Sporothrix schenckii, and Geotrichum candidum (Neville et al., 2009; Samaranayake and MacFarlane, 1990). This study aimed identifying species’s colonizing dental appliances surfaces.
MATERIALS AND METHODS
This cross-sectional study was conducted among patients wearing dental appliances, 60 patients were submitted to a detailed clinical interview and oral clinical examination, and were instructed to keep their dentures. After obtaining informed consent and before collecting samples, a questionnaire was performed among dental wearers. From literature various factors may contribute to increase or decrease in fungal growth these may include oral hygiene of patient, immune status of patient and the medication patient is taking. So, all these factors were considered in this study. Sixty patients wearing dental appliances were selected according to following criteria: Patient included were clinically healthy; they had good oral hygiene and clinically normal oral mucosa, and had no any kind of medication, the study received approval from the ethical committee.
After obtaining informed consent and before collecting samples, a questionnaire was performed among oral appliances wearers; it included (presence of carries, pain, or odour, teeth brushing per day, toothbrushing duration, prior treatment, type of appliance). Swabs were taken according to a standard protocol. Samples were taken of each appliancee surface by means of sterile swabs (that is, each was left in place for 30 s), samples were obtained by swabbing a region (1 × 5 cm line) of the anterior flange of the appliance. Orthodontic appliances were assessed using sterile swabs on the metallic braces (Figure 1).
All samples were inoculated on Sabouraud dextrose agar (SDA) medium and incubated at 30°C for 7 to 14 days, to allow filamentous fungi and yeasts to grow. Identification of species was performed by phenotypical tests (germ tube formation, chlamidoconidia production), and with the aid of commercially available systems like biochemical carbohydrate fermentation and assimilation using Api 20c and Auxacolor. Data were managed and analyzed using statistical software 17.0 (SPSS, Inc., Chicago, IL).

RESULTS
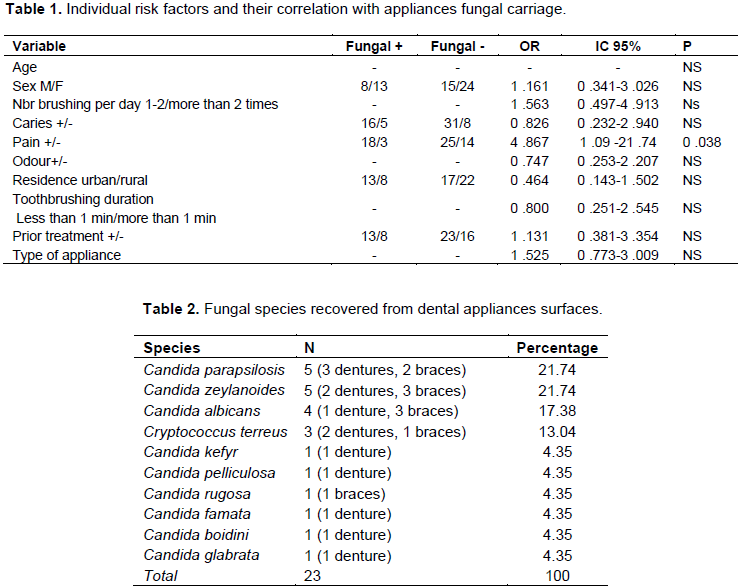
The 60 patients using dental appliance enrolled in this study had a mean age of 48 ± 2.62 years, the age range of the participants was between 10 and 79. The 60 dental appliances were composed of 34 prosthodontics (dentures) and 26 orthodontics appliances (braces). The overall prevalence of fungal contamination of dental appliances was 35% (21/60). The specific prevalence of fungal contamination of denture was 38% (13/34), and the fungal contamination of braces was 31% (8/26). Dentures were the most contaminated appliances. Pain, burning and discomfort were correlated to fungal carriage p=0.038; OR=4.867 IC 95% (1.09-21.74) (Table 1).
Yeasts of Candida genus were present in 20 (86.96%) of positives appliances. Candida parapsilosis and Candida zeylanoides were the species most recovered in this study (21.74% respectively). The various species are outlined in Table 2. Two samples were polymicrobials with the concomitant presence of C. parapsilosis and C. zeylonoides.
DISCUSSION
Denture-induced stomatitis is an inflammatory reaction of the denture-bearing mucosa that affects approximately 65% of complete upper denture wearers (Webb et al., 1998), in our study fungal contamination was more important among dentures.
Fungi and protozoa may find favorable conditions to thrive in dental units. Literature papers have reported microorganism counts ranging from 100 to 400.000 CFU/ml in dental units (Kim et al., 2000; Ozcan et al., 2003). It is usually asymptomatic; however, may cause mild soreness or burning sensation in some (Krishnan, 2012), we found a strong correlation between fungal presence and soreness or burning sensation (p=0.038); OR=4.867 IC 95% (1.09-21.74). Poor hygiene of dentures is also associated with fungal stomatitis (Grimound et al., 2005; Budtz-Jörgensen, 1978). Disinfection of dentures and dental appliances plays a key role in eradicating this form of candida infections (Muzyka, 2005), but number of brushing per day and duration of brushing teethes was not linked to presence of fungi in our study.
In a previous study, the duration of denture use was ranging from 3 weeks to more than 40 years, was generally unrelated to degree of contamination (Glass et al., 2001), in concordance with our results. On the other hand, Gujar et al. (2020) found that the microbial contamination in metallic brackets was higher than that of aligners, when used for a month. The porosity of the acrylic allows fungal and bacterial contamination throughout the entire denture (Glass et al., 2001). Moreover, the relatively acidic and anaerobic microclimate underneath the denture provides an ideal environment for yeast growth, and the denture shields the mucosa from the saliva and its local immunity-enhancing properties. Thus, the denture or any acrylic-containing dental appliance can serve as a source of inoculation for bacteria and fungi (Muzyka, 2005).
Candida species may be recovered from up to one-third of the mouths of normal individuals and are considered inhabitants of the normal flora of oral and gastrointestinal tract (Krishnan, 2012). However, the involvement of Candida as the main causative agent in denture-induced stomatitis (Pinto et al., 2008) was first described by Cahn in 1936, Candida albicans remains the most frequently isolated fungal in the oral cavity but other species have also been isolated and involved in disease (Garg et al., 2012), C. albicans occurred in the third place. The most commonly occurring dental fungal infection is caused by Candida species with C. albicans most often encountered (Muzyka, 2005), this is in accordance with our results.
Filamentous fungi can also be considered as biofilm-forming organisms because they are well adapted to grow on both biotic and abiotic surfaces. The formation of biofilms (Damasceno et al., 2017), but we did not recorded any filamentous fungi in this study.
In vitro adherence studies illustrate that C. albicans attaches readily to various resins, glass, and metal surfaces. The ability of C. albicans to adhere to polymeric surfaces has been correlated with attractive hydrophobic and repulsive electrostatic forces (Garg et al., 2012).
In denture wearers, Candidiasis is aggravated by the adhesion of C. albicans to the tissue surface of the maxillary denture base, which serves as an effective reservoir of microorganisms (Garg et al., 2012).
Of the organisms recovered in this study, C. parapsilosis, C. famata, C. rugosa and C. glabrata are most frequently involved in human infections. Species that were once considered to be saprophytic are becoming more commonly associated as opportunists causing human disease.
In another study, Candida species isolated from complete upper denture wearers were C. albicans, C. glabrata, C. parapsilosis, C. guillermondii, C. krusei, C. lusitaniae, C. tropicalis (Pinto et al., 2008), Candida kefyr and Cryptococcus were involved in oral fungal infections (Krishnan, 2012).
Basically, the present analysis has pointed to a high prevalence of fungal organisms in oral appliances, in another study samples obtained at both peri-implantitis (31.6%) and healthy (40%) implant sites were dominated by Candida sp (Schwarz et al., 2015), which is in accordance with our results.
C. albicans, C. boidinii, and Rhodotorula sp have already been identify by Polymerase chain reaction (PCR) in oral peri-implantis sites (Schwarz et al., 2015), C. glabrata was also found in denture appliance (Glass et al., 2001).
C. boidinii is widespread and it has been isolated from diverse substrate related to human activity (wine fermentation, olive manufacturing, tepache), and natural environments (soil, seawater, sap fluxes of many sugar rich tree species (Camiolo et al., 2017).
Cryptococcosis also infects the central nervous system, skin and the oral mucous membrane (Glick et al., 1987), it can produce a variety of cutaneous and oral mucosal manifestations such as superficial ulcers, nodules, granulomas or carcinoma-like lesions (Myrvik and Weiser, 1988). Intraoral sites commonly affected are gingiva, palate and tooth socket after extraction. Violaceous nodules of granulation tissue, swellings and ulcers are the various forms of oral lesions reported (Samaranayake and MacFarlane, 1990). The numerous opportunistic and pathogenic microorganisms found in this study were unexpected and are known to produce not only substantial oral infections, but also systemic diseases as mentioned in previous studies (Pinto et al., 2008). Furthermore, the present analysis failed to identify any significant correlation of either fungal organisms or disease severity with risk factors, such as caries and teeth brushing.
CONCLUSION
Candida species are assumed to cause disease by direct tissue invasion, either by inducing a hypersensitive state or by producing potent Candida toxins. The use of oral appliances is known to increase the carriage of Candida in healthy patients, and the proliferation of Candida sp strains can be associated with denture-induced stomatitis. Being aware of these fungal risks, disinfection of dental appliances must be reinforced, and it is desirable to institute procedures to minimize the number of potentially fungal pathogenic agents.
CONFLICT OF INTERESTS
The authors have not declared any conflict of interests.
ACKNOWLEDGEMENT
The authors appreciate the staff of the department of dentistry.
REFERENCES
|
Barbeau J, Séguin J, Goulet JP, de Koninck L, Avon SL, Lalonde B, Rompré P, Deslauriers N (2003). Reassessing the presence of Candida albicans in denture-relatedstomatitis. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 95(1):51-59. |
|
|
Budtz-Jörgensen E (1978). Clinical aspects of Candida infection in denture wearers. Journal of the American Dental Association 96(3):474-479. |
|
|
Camiolo S, Porru C, Benitez-Cabello A, Rodriguez-Gomez F (2017). Genome overview of eight Candida boidinii strains isolated from human activities and wild environments. Standards in Genomic Sciences 12:70. |
|
|
Damasceno JL, dos Santos RA, Barbosa AH, Casemiro LA, Pires RH, Gomes Martins CH (2017). Risk of Fungal Infection to Dental Patients. Hindawi ID 2982478, 8 p. |
|
|
Figueiral MH, Azul A, Pinto E, Fonseca PA, Branco FM, Scully C (2007). Denture-related stomatitis: Identification of aetiological and predisposing factors - A large cohort. Journal of Oral Rehabilitation 34(6):448-455. |
|
|
Garg SK, Singh VA, Garg SK, Mittal S, Chahal GK (2012). Effect of denture wearing on occurrence of fungalisolates in the oral cavity: A pilot study. Clinical and Experimental Dentistry 4(2):86-90. |
|
|
Glass RT, Bullard JW, Hadley CS, Mix EW, Conrad RS (2001). Partial spectrum of micro-organisms found in dentures and possible disease implications. Journal of the American Osteopathic Association 101(2):92-94. |
|
|
Glick M, Cohen SG, Cheney RT, Crooks GW, Greenberg MS (1987). Oral manifestations of disseminated Cryptococcus neoformans in a patient with acquired immune deficiency syndrome. Oral Surgery, Oral Medicine, Oral Pathology 64(4):454-459. |
|
|
Grimound A, Lodter J, Marty N, Andrieu S, Bocquet H, Linas M, Rumeau M, Cazard JC (2005). Improved oral hygiene and Candida species colonization level in geriatric patients. Oral Diseases 11(3):163-169. |
|
|
Gujar AN, Al-Hazmi A, Raj AT, Patil S (2020). Microbial profile in different orthodontic appliances by checkerboard DNA-DNA hybridization: An in-vivo study. American Journal of Orthodontics and Dentofacial Orthopedics 157(1):49-58. |
|
|
Kim PJ, Cederberg RA, Puttaiah R (2000). A pilot study of 2 methods for control of dental unit biofilms. Quintessence International 31(1):41-48. |
|
|
Krishnan AP (2012). Fungal infections of the oral mucosa. Indian Journal of Dental Research 23(5). |
|
|
Moreira LVG, Macedo AGO, Cunha AF, Olga Maranhão OBV, Macêdo-Costa MR, de Lima KC, Caldas SGFR, Pereira HSG (2016). Microbial contamination of orthodontic appliances made of acrylic resin. African Journal of Microbiology Research 10(27):1051-1055. |
|
|
Muzyka BC (2005). Oral fungal infections. Dental Clinics of North America 49(1):49-65. |
|
|
Myrvik QN, Weiser RS (1988). Fundamentals of medicalbacteriology and mycology. 2nd ed. Philadelphia: Lea and Febiger. |
|
|
Neville BW, Damm DD, Allen CM, Bouquot JE (2009). Fungal and protozoal diseases. In: Neville, Damm, Allen, Bouquot Oral and maxilla facialpathology. 3rd ed. Philadelphia: WB Saunder pp. 224-237. |
|
|
Ozcan MY, Kulak Y, Kazazoglu E (2003). The effect of disinfectant agents in eliminating the contamination of dental unit water. Journal of Oral Rehabilitation 30(3):290-294. |
|
|
Pinto TMS, Neves ACC, Leão MVP, Jorge AOC (2008). Vinegar as an antimicrobial agent for control of candida spp. incomplete denture wearers. Journal of Applied Oral Science 16(6):385-389. |
|
|
Samaranayake LP, MacFarlane TW (1990). Oral candidosis. London: Wright. |
|
|
Schwarz F, Becker K, Rahn S, Hegewal A, Pfeffer K, Henrich B (2015). Real-time PCR analysis of fungal organisms and bacterial species at peri-implantitis sites. Schwarz et al. International Journal of Implant Dentistry 1:9. |
|
|
Webb BC, Thomas CJ, Willcox MD, Harty DW, Knox KW (1998). Candida associated denture stomatitis. A etiology and management: a review. Part 2. Oral diseases caused by Candida species. Australian Dental Journal 43(3):160-166. |
|
Copyright © 2024 Author(s) retain the copyright of this article.
This article is published under the terms of the Creative Commons Attribution License 4.0