Full Length Research Paper
ABSTRACT
COVID-19 is a major public health emergency that has recently shaken the world. Pregnant women have not been spared from this pandemic. Although there is no clinical difference between them and the general population, pregnant women are at increased risk of developing severe forms and pregnancy-related complications. The objective of this study was to investigate the presence of anti-SARS-CoV-2 antibodies and to identify associated factors in pregnant women followed at the Regional Hospital Center (CHR) of Saint-Louis, Senegal. A cross-sectional, prospective and descriptive study was conducted among 400 pregnant women followed at the Saint-Louis Regional Hospital (Senegal) over a five-month period from March to July, 2021. None of the patients had received an anti-COVID-19 vaccine. Determination of anti-SARS-CoV-2 antibodies was performed by the Healgen IgG/IgM SARS-CoV-2 qualitative rapid test. 400 pregnant women were included in the study. The mean age was 27.8 years (±6.3). The most representative age group was between 25 and 29 years with 29%. The majority of patients (76.8%) were housewives. Only 41 patients (10.3%) had travelled outside Saint-Louis (Senegal) in the previous 6 months. None of the patients had received anti-COVID-19 vaccine. Anti-SARS-CoV-2 antibody testing was positive in 232 cases (58%). IgG anti-SARS-CoV-2 antibodies were present in all the 232 women (100%) and IgM was in 6 cases (2.6%). The study showed a high seroprevalence of anti-SARS-CoV-2 in pregnant women followed at the Saint-Louis Regional Hospital (Senegal) showing a large underestimation of the pandemic in that population. Further evaluation on the role of SRAS-CoV-2 antibodies in the protection against the virus or outcome of pregnancy women need to be investigated on a larger size of pregnant women.
Key words: Seroprevalence, SARS-CoV-2, pregnant women, Saint-Louis, Senegal.
INTRODUCTION
SARS-CoV-2 infection is a global health emergency. First appearing in China's Hubei province in late 2019, it has spread rapidly around the world. As of November 2022, the World Health Organization (WHO) has recorded 636 million infected people worldwide with 6.6 million deaths (Statistics of Coronavirus in the World, 2022). On the same time, Senegal recorded 88859 infected people including 86858 recovery persons and 1968 deaths (Pandémie COVID-19/Sénégal: Communiqué994, 2022). SARS-CoV-2 infection is responsible for variable clinical pictures that can range from simple forms associating fever, cough, myalgia, headache and possibly digestive disorders as well as severe forms responsible for an acute respiratory distress syndrome that can lead to death (Peyronnet et al., 2020). Several risk factors for the development of acute respiratory distress syndrome, such as advanced age, male gender, presence of comorbidities, oxygen desaturation, and abnormal biological parameters (elevated LDH, elevated procalcitonin, low CD4 count, hypoalbuminemia) have been identified in the literature (Chen et al., 2020a). However, data on COVID-19 in pregnant women remain limited (Flannery et al., 2020).
Early study in China series did not appear to show any difference in COVID-19 positive in pregnant women compared to the general population clinically. However, it appears that SARS-C-oV-2 positive pregnant women are at increased risk of developing severe forms and pregnancy-related complications (Moore and Suthar, 2021; Peyronnet et al., 2020). Intrauterine maternal-fetal transmission has not been reported but cases of early infected neonates suggest probable vertical transmission per-partum or neonatally (Peyronnet et al., 2020).
The objective of this study was to investigate the presence of anti-SARS-CoV-2 antibodies and to identify COVID-19 associated factors in pregnant women followed at the Regional Hospital Center of Saint-Louis (Senegal).
METHODOLOGY
The study population is selected with ancillary study of the seroepidemiological survey of hepatitis E conducted among pregnant women in Senegal. The enrollment of participants was carried out from March to July 2021 at the regional hospital of Saint-Louis (Senegal). Socio-demographic characteristics and inclusion criteria of the participants were fully described (Viruses 2022, 14, 1742. https://doi.org/10.3390/v14081742) (Diouara et al., 2022). The free and informed consent of the pregnant women was obtained verbally, individually. The management of the information was done in strict compliance with medical secret.
Ethical and administrative authorization was obtained from the National Health Research Ethics Committee of Senegal (N°000130/MSA/CNRES/Sec).
For sample collection and processing, 400 pregnant women were recruited in this study. Determination of anti-SARS-CoV-2 antibodies (in the residual plasma samples collected as part of the hepatitis E seroepidemiological study) was performed by the Healgen IgG/IgM SARS-CoV-2 rapid qualitative test according to the manufacturer’s instructions. This assay uses lateral flow technology for the qualitative and differential detection of anti-SARS-CoV-2 IgM and IgG antibodies. All plasma samples were biobanking in -80 until their use. From the data collected, the following parameters were investigated:
1. Socio-demographic aspects: Age, marital status and regime, profession, level of education, socio-economic level, travel outside Saint-Louis (Senegal) in the last 6 months, gestational age, anti-COVID-19 vaccination.
2. Serological aspects: Presence or absence of anti-SARS-CoV-2 IgM and/or IgG.
Data entry and analysis were done using Excel and Epi info7 software. Categorical variables were expressed as proportions and numerical variables as median and standard deviation.
RESULTS
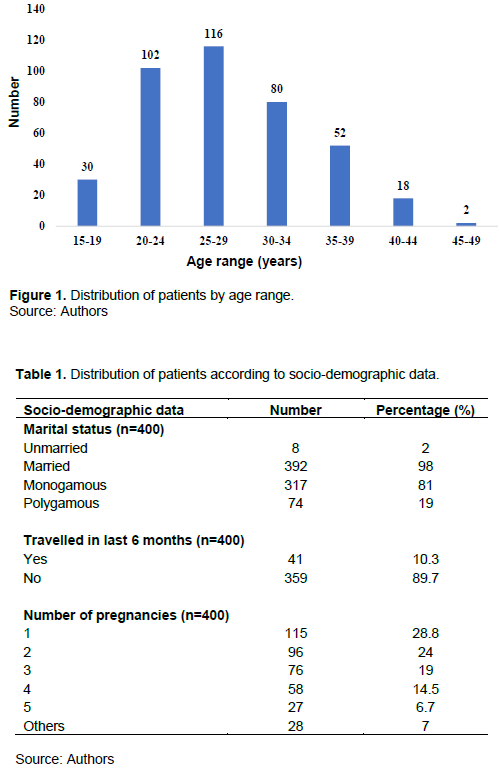
400 pregnant women were included in the study. The mean age was 27.8 years (±6.3). The most representative age group was between 25 and 29 years with 116 cases (29%) (Figure 1). They were married in 392 cases (98%) under monogamous regime with 317 cases (81%). The majority of patients were housewives with 307 cases (76.8%). Only 41 patients (10.3%) had travelled outside Saint-Louis (Senegal) in the last 6 months. No patient had received a COVID-19 vaccine. The median gestation was 2 with extremes of 1 and 11. Primiparous women were in the majority with 115 cases (28.8%) (Table 1).
Concerning seroprevalence of SRAS-CoV-2 in pregnancy women, all patients were tested for the presence of anti-SARS-CoV-2. They were positive in 232 cases (58%) and IgG anti-SARS-CoV-2 antibodies were present in all of those 232 cases (100%). However, 6 (2.6%) of them had simultaneous IgM anti-SARS-CoV-2 antibodies.
DISCUSSION
The COVID-19 pandemic has resulted in a global health crisis that has impacted all areas of life. Its rapid progression and the lack of knowledge of its impact on pregnancy at the beginning of the pandemic led obstetricians to adapt their practice. Current knowledge suggests that there is no risk of maternal-fetal transmission of SARS-CoV-2 (Chen et al., 2020b). However, cases of COVID-19-infected newborns diagnosed from samples taken several hours after birth have been published. Some studies point to the possibility of vertical transmission through the detection of IgM in the serum of newborns of infected mothers (Zeng et al., 2020).
However, samples of the amniotic fluid and cord blood of the newborn show the absence of the virus in the majority of cases of infection that occur during the third trimester of pregnancy. Information on patients exposed in early pregnancy is currently scarce (Dong et al., 2020). Teratogenicity of SARS-CoV-2 appears to be unlikely but may increase the risk of growth retardation and fetal death in utero. Hence the need for strict monitoring of the fetal growth curve, particularly during the third trimester of pregnancy (Schwartz and Graham, 2020). The clinical course of SARS-CoV-2 infection in pregnant women is similar to that of non-pregnant women, although fever appears to be less prevalent than in the general population (Kouas et al., 2020).
During pregnancy, physiological and immunological changes make pregnant women more susceptible to viral respiratory infections and severe pneumonia. Studies done during the SARS-CoV-1 and MERS-CoV epidemics showed that pregnant women were at higher risk of developing severe complications (Juan et al., 2020; Lambelet et al., 2020).
In our series, the mean age of the patients was 27.8 years (±6.3). In Ethiopia, Assefa et al. (2021) found a mean age of 23.9 years. The majority of our patients were housewives (76.8%), as in a Cameroonian study where 44% of pregnant women were unemployed (Moustapha et al., 2022). Precariousness and promiscuity are risk factors for the occurrence of SARS-CoV-2 infection in pregnant women (Ngaba et al., 2021). For diagnosis of SARS-CoV-2 infection, PCR (direct diagnosis) and serological tests (indirect diagnosis) are used (Hantz, 2020). A disadvantage of indirect diagnosis is the limited sensitivity at an early stage, when the host has not yet developed specific antibodies. Indeed, during SARS-CoV-2 infection, data from the literature have shown antibody production beginning after the first week of infection and generally detectable from the second (Van Elslande et al., 2021). IgM type antibodies appear from the 7th day and IgG type antibodies from the 10th day (Hantz, 2020). IgG will persist in circulation for months (Sh. Nur et al., 2022). In this study, the seroprevalence of anti-SARS-CoV-2 was 58%. This seroprevalence was much higher than those found in the literature in Philadelphia and Ethiopia with respectively 6.2 and 5.7% (Assefa et al., 2021; Flannery et al., 2020). In Somalia, seroprevalence of 36.7% was found by Sh Nur and al. (2022). In a Parisian hospital, four months after the beginning of the epidemic, the seroprevalence of IgG was 4.7% among women giving birth (Tsatsaris et al., 2021).
The results provide sufficient evidence that the pregnant women followed at the hospital were largely affected by COVID-19. They had not developed severe forms that could require hospitalization. In Senegal, the same observation was made by Diouf et al. (2020) who did not find any severe forms in their study.
Indeed, in Jering's study, about 5 to 10% of pregnant women had a severe form of the disease, 4% were admitted to intensive care and 3% required mechanical ventilation (Jering et al., 2021). They also had more heart attacks and venous thromboembolic events than pregnant women not infected with SARS-CoV-2 (Jering et al., 2021). Certain comorbidities such as advanced maternal age, high body mass index, pre-existing hypertension and diabetes mellitus are risk factors for the occurrence of severe forms of COVID-19 in pregnant women (Jering et al., 2021). Indeed, the risk of infection and development of other complications is high during pregnancy. Despite the possibility of passive immunization, the best prevention to protect the mother from SARS-CoV-2 infection is vaccination, which will provide the fetus and the newborn with strong and effective protection against infection through passive placental transfer of specific antibodies (Zambrano et al., 2021). Placenta functions as an immunological barrier preventing viral transfer to the fetus, but allows the transfer of immunological components, such us immunoglobulins. In addition, the rate of seroprevalence in the newborns demonstrates an active communication between maternal immune system and fetus (Zambrano et al., 2021).
CONCLUSION
The study showed a high seroprevalence of anti-SARS-CoV-2 antibodies in pregnant women followed in Saint-Louis (Senegal) showing a large underestimation of the pandemic in that population. Cross-tabulations between different parameters reveal no associated factors with such high prevalence. Further evaluation on the role of SRAS-CoV-2 antibodies in the protection against the virus or outcome of pregnancy women need to be investigated on a larger size of pregnant women.
CONFLICT OF INTERESTS
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
This work was supported by Institut de Recherche pour le Développement (IRD) through its program of Young team associated with IRD (JEAI EPIVHE) and IRESSEF. The authors express their thanks to IRD (JEAI EPIVHE) and IRESSEF, CERPAD and CHR-Saint-Louis.
REFERENCES
|
Assefa N, Regassa LD, Teklemariam Z, Oundo J, Madrid L, Dessie Y, Scott J (2021). Seroprevalence of anti-SARS-CoV-2 antibodies in women attending antenatal care in eastern Ethiopia: a facility-based surveillance. British Medical Journal Open 11(11):e055834. |
|
|
Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Li J, Zhao D, Xu D, Gong Q, Liao J, Yang H, Hou W, Zhang Y (2020a). Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet 7;395(10226):809-815. |
|
|
Chen T, Dai Z, Mo P, Li X, Ma Z, Song S, Chen X, Luo M, Liang K, Gao S, Zhang Y, Deng L, Xiong Y (2020b). Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China (2019): a single-centered, retrospective study. The Journals of Gerontology. Series A, Biological Sciences and Medical Science 75:1788-95. |
|
|
Diouara AAM, Lo S, Nguer CM, Senghor A, Diop-Ndiaye H, Manga NM, Danfakha F, Diallo S, Faye-Dieme ME, Thiam O, Biaye B, Manga NMP, Thiam F, Sarr H, Lo G, Ndour M, Manga SP, Diaby N, Dieng M, Diop I, Dieye Y, Toure Kane C, Peeters M, Ayouba A (2022). Hepatitis E Virus Seroprevalence and Associated Risk Factors in Pregnant Women Attending Antenatal Consultations in Senegal. Viruses 14:1742. |
|
|
Diouf AA, Diallo-Mbaye K, Guèye M, Thioub D, Niang N, Dekou CY, Gueye MDN, Diallo M, Mbaye M, Dieme MEF, Diouf A, Seydi M (2020). Clinical characteristics and outcomes of COVID-19 infection in nine pregnant women: a report from a sub-Saharan African country, Senegal. Pan African Medical Journal 35(2):58. |
|
|
Dong L, Tian J, He S, Zhu C, Wang J, Liu C, Yang J (2020). Possible Vertical Transmission of SARS-CoV-2 From an Infected Mother to Her Newborn. Journal of the American Medical Association 12:323(18):1846-1848. |
|
|
Flannery DD, Gouma S, Dhudasia MB, Mukhopadhyay S, Pfeifer MR, Woodford EC, Gerber JS, Arevalo CP, Bolton MJ, Weirick ME, Goodwin EC, Anderson EM, Greenplate AR, Kim J, Han N, Pattekar A, Dougherty J, Kuthuru O, Mathew D, Baxter AE, Vella LA, Weaver J, Verma A, Leite R, Morris JS, Rader DJ, Elovitz MA, Wherry EJ, Puopolo KM, Hensley SE (2020). SARS-CoV-2 seroprevalence among parturient women in Philadelphia. Science Immunology 5(49):eabd5709. |
|
|
Hantz S (2020). Diagnostic biologique de l'infection à Sars-CoV-2: stratégies et interprétation des résultats. Revue Francophone des Laboratoires 526:48-56. |
|
|
Jering KS, Claggett BL, Cunningham JW, Rosenthal N, Greene MF, Solomon SD (2021). Clinical Characteristics and Outcomes of Hospitalized Women Giving Birth With and Without COVID-19. Journal of the American Medical Association Internal Medicine e209241. |
|
|
Juan J, Gil MM, Rong Z, Zhang Y, Yang H, Poon LC (2020). Effect of coronavirus disease 2019 (COVID-19) on maternal, perinatal and neonatal outcome: systematic review. Ultrasound Obstetrics Gynecology 56:15-27. |
|
|
Kouas S, Zoukar O, Ikridih K, Mahdhi S, Belghaieb I, Haddad A (2020). Infection COVID-19 chez la femme enceinte: à propos d'un cas. Pan African Medical Journal 37(156):1-6. |
|
|
Lambelet V, Vouga M, Pomar L, Favre G, Gerbier E, Panchaud A, Baud D (2020). SARSCoV-2 in the context of past coronaviruses epidemics: Consideration for prenatal care. Prenatal Diagnosis 40(13):1641-1654. |
|
|
Moore KM, Suthar MS (2021). Comprehensive analysis of COVID-19 during pregnancy. Biochemical and Biophysical Research Communications 538:180-6. |
|
|
Moustapha B, Ngalame AN, Tchente CN, Okala F, Ombaku K, Neng H, Kamdem D, Julie N, Sandrine N, Mwadjie D, Mboudou E (2022). Covid-19 in Pregnancy: Cases of Women Managed in the City of Douala-Cameroon Open Journal of Obstetrics and Gynecology 12:1019-1030. |
|
|
Ngaba GP, Kalla GCM, Assob JCN, Njouendou AJ, Jembe CN, Mboudou ET, Mbopi-Keou FX (2021). Evaluation de deux tests de diagnostic antigénique du COVID-19: BIOSYNEX® COVID19 Ag BSS et BIOSYNEX® COVID-19 Ag+ BSS comparés à la PCR Ampli Quick® SARS-CoV-2. Pan African Medical Journal 39:228. |
|
|
Pandémie COVID-19 (2022). Pandémie COVID-19/Sénégal: Communiqué 994. |
|
|
Peyronnet V, Sibiude J, Huissoud C, Lescure FX, Lucet JC, Mandelbrot L, Nisand I, Belaish-Allart J, Vayssière C, Yazpandanah Y, Luton D, Picone O (2020). Infection par le SARS-CoV-2 chez les femmes enceintes. Etat des connaissances et proposition de prise en charge. CNGOF. Gynécologie Obstétrique Fertilité & Sénologie 3288:1-8. |
|
|
Schwartz DA, Graham AL (2020). Potential Maternal and Infant Outcomes from (Wuhan) Coronavirus 2019-nCoV Infecting Pregnant Women: Lessons from SARS, MERS, and Other Human Coronavirus Infections. Viruses 12(2):19. |
|
|
Sh. Nur MA, Dahie HA, Hassan NA, Garba B, Adam MHA, Mohamoud JH, Dirie NI (2022). Seroprevalence of SARS-CoV-2 virus antibodies and sociodemographic features of pregnant women in Mogadishu, Somalia: a cross-sectional survey study. British Medical Journal Open 12:e059617. |
|
|
Statistics of Coronavirus in the world (2022). |
|
|
Tsatsaris V, Mariaggi AA, Launay O, Couffignal C, Rousseau J, Ancel PY, Marcault E, Ville Y, Cordier AG, Vivanti A, Carrara J, Luton D, Dommergues M, Borie C, Kayem G, Alessandrini V, Lecomte L, Meritet JF, Leruez-Ville M, Goffinet F, Dubois C, Picone O, Vauloup Fellous C (2021). SARS-CoV-2 IgG antibody response in pregnant women at delivery. Journal of Gynecology Obstetrics and Human Reproduction. 50(7):102041. |
|
|
Van Elslande J, Vermeersch P, Kris Vandervoort K, Wawina-Bokalanga T, Vanmechelen B, Wollants E, Laenen L, André E, Van Ranst M, Lagrou K, Maes P (2021). Symptomatic Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Reinfection by a Phylogenetically Distinct Strain. Clinical Infectious Diseases 73(2):354-356. |
|
|
Zambrano H, Anchundia K, Aviles D, Andaluz R, Calderon N, Torres E, Gonzalez-Granda N, Maxwell A, Chen K, Gonik B, Mor G (2021). Seroprevalence of SARS-CoV-2 immunoglobulins in pregnant women and neonatal cord blood from a highly impacted region. Placenta 115:146-150. |
|
|
Zeng L, Xia S, Yuan W, Yan K, Xiao F, Shao J, Zhou W (2020). Neonatal Early-Onset Infection With SARS-CoV-2 in 33 Neonates Born to Mothers With COVID-19 in Wuhan, China. Journal of the American Medical Association Pediatrics 174(7):722-725. |
|
Copyright © 2024 Author(s) retain the copyright of this article.
This article is published under the terms of the Creative Commons Attribution License 4.0