ABSTRACT
Extended spectrum β-lactamase (ESBL) producing Escherichia coli and Klebsiella pneumoniae causing urinary tract infection (UTI) constitutes a significant therapeutic challenge. The aim of this study was to investigate the frequency of ESBL producing Escherichia coli and Klebsiella pneumoniae isolated from urine samples. Clinical isolates of multidrug resistant Gram negative rods (n=102) were taken from urine specimens from tertiary care hospital Lahore. Micro-organisms were identified on the basis of their morphology, cultural characteristics, and confirmed using API 20E. Identified E. coli and K. pneumoniae were subjected to susceptibility testing using Kirby-Bauer disc diffusion method as per CLSI guidelines. Furthermore, phenotypic confirmation of ESBL production was done according to CLSI guidelines. Out of 102 multidrug resistant Gram negative rods 97 (95%) were ESBL producers isolated from different urine specimens from different wards of hospitals (emergency, ICU, urology ward); among these 64 (66%) were E. coli and 33 (34%) were K. pneumoniae. Antimicrobial susceptibility pattern of ESBL producing pathogens showed that 75% of these pathogens were resistant to ciprofloxacin whereas most effective drug was meropenem and pipracillin+tazobactam. Meropenem could be used as an alternative treatment option for UTI related to ESBL producing E. coli and K. pneumoniae. High prevalence of these ESBL producing pathogens are alarming and need special consideration.
Key words: Extended spectrum β-lactamases, urinary tract infection, Escherichia coli, Klebsiella pneumoniae.
Urinary tract infection (UTI) has been reported to affect around more than 150 million people globally every year (Picozzi et al., 2014). High burden of UTI are mainly due to Gram negative rods (GNR) (80 to 85%) among these the leading pathogens are Escherichia coli (75 to 95%) and Klebsiella pneumoniae (Tanvir et al., 2012; Jamil et al., 2014). It is also the second main cause of nosocomial infections at our setup (Qamar et al., 2014). This is associated with a high risk of morbidity, mortality, extra financial budget and even, fatal consequences (Hasan et al., 2013). World Health Organization and the European Commission has recognized the importance of studying the emergence of different antimicrobial resistant determinants and it is the need to develop appropriate strategies for their control particularly the spread of extended spectrum β-lactamase (ESBL) producing E. coli and K. pneumoniae (Picozzi et al., 2013). Production of ESBL is a significant resistance-mechanism that impedes the antimicrobial treatment of infections caused by Enterobacteriaceae and is a serious threat to the currently available antibiotic armory (Shaikh et al., 2015). ESBLs are a group of plasmid-mediated, diverse, complex and rapidly evolving enzymes that are posing a major therapeutic challenge today in the treatment of hospitalized and community-based patients (Rawat and Nair, 2010). Reflects the same as previous sentence. They force the physician to use expensive carbapenems to which these are sensitive. The ESBL producers can also develop co-resistance to other classes of antimicrobial agents, such as fluoroquinolones, co-trimoxazole, and aminoglycosides, which are also frequently used for UTI (Potron et al., 2015, Liu et al., 2011). Seriously ill patients with prolonged hospital stays and in whom invasive medical devices are present (urinary catheters, endotracheal tubes) for long duration are at high risk for colonization and infection with ESBL (Peirano and Pitout, 2010). Therefore the aim of this study is to investigate the frequency of ESBL producing E. coli and K. pneumoniae isolated from urine specimens in a tertiary care hospital Lahore, Pakistan.
A total of 102 multidrug resistant (MDR) clinical isolates of Gram negative rods were taken from hospitalized UTI patients from different sources (emergency, ICU, urology ward) during December 2013 to December 2014 from tertiary care hospital Lahore.
Identification/purification of isolates
The isolates were culture on blood and MacConkey agar and plates were incubated at 37°C aerobically overnight. The isolates were preliminarily identified on the basis of their morphology and culture characteristics and biochemical profile. Gram-negative isolates particularly E. coli and K. pneumoniae were further confirmed by API 20E (BioMerieux, France) (Figure 1).
Antimicrobial susceptibility testing
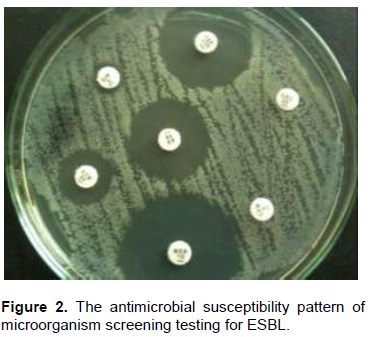
Antimicrobial susceptibility of isolates was performed by Kirby-Bauer disk diffusion method using Mueller-Hinton agar (Oxoid UK), according to Clinical Laboratory Standards Institute (CLSI) 2012 guidelines (Wikler et al., 2012). The plates were do you mean streaked and inoculated at 35°C for 24 h. Implanted antibiotics were ampicillin (10 μg), cefuroxime (30 μg), ceftriaxone (30 μg), ciprofloxacin (5 μg), amikacin (30 μg), piperacillin+tazobactam (110 μg), co-amoxeclav (20/10 μg), aztronam (30 μg) and meropenem (10 μg). The interpretation of susceptibility results were done according to CLSI guidelines (Figure 2). Statistical analysis was done using SPSS 22.0.
Screening test was performed using Kirby-Bauer disk diffusion method as per CLSI guidelines (2012). The antibiotic disks of ceftazidime (30 µg), aztreonam (30 µg), cefotaxime (30 µg), ceftriaxone (30 µg) were placed on the Mueller Hinton agar (Oxoid) plates per CLSI guidelines. Isolates showing inhibition zone size of ≤ 22 mm with ceftazidime (30 µg), ≤ 27 mm with aztreonam (30 µg), ≤ 27 mm with cefotaxime (30 µg), ≤ 25 mm with ceftriaxone (30 µg) were identified as ESBL positive.
Double disc synergy test ESBL
The double disk synergy test was performed by placing a disk of co-amoxiclav in the center of the plate while ceftazidime (30 µg), cefotaxime (30 µg), ceftriaxone (30 µg) and cefepime (30 µg) were placed at 20 mm distance center to center from co-amoxiclav disk.
The plates were incubated at 37°C for 18 to 24 h. Isolates which showed zone of inhibition greater than 5 mm on the co-amoxiclav side of the disk compared to the results seen on the side without co-amoxiclav were confirmed as ESBL producers (Figure 3) (Hannan et al., 2013).
Out of 102 clinical isolates; 66 (64.7%) were E. coli and 36 (35.3%) were K. pneumonie. Among these 97 (95%) were ESBL producers; 64 (66%) were Escherichia coli and 33 (34%) were K. pneumoniae. Male to female ratio was 1: 2.4 patients (P-value <0.05).
Overall susceptibility pattern of ESBL producing pathogens showed high drug resistance against ESBLs are intrinsically resistant to these drugs, no need to mention here, moderate resistance was observed against ciprofloxacin (75%) whereas most effective drugs was meropenem and pipracillin+tazobactam (Figure 4).
Extensive and misuse of β-lactam antibiotics in hospital and community produce a high bacterial resistance which can lead to increased morbidity, mortality and health care costs. During the past decades, ESBL producing E. coli and K. pneumoniae have emerged as dangerous pathogens both in hospital and community acquired infections due to extensive use of antibiotics particularly third generation cephalosporins. Recent studies revealed that patients with ESBL producing organisms had significantly higher fatality rate than those with non-ESBL isolates (Mehrgan and Rahbar, 2008). The prevalence of ESBL among the clinical isolates varies greatly worldwide and rapidly changing over time. In present study frequency of ESBL producing pathogens was greater in male as compare to female and E. coli was the predominant organism. These results are in accordance with the previous studies conducted in Pakistan that reported the high frequency of ESBL producing E. coli among females current study shows higher incidence in males, so it is not in accordance with the cited studies (Ejaz et al., 2011, Kausar et al., 2014). This could be due to the limited health care facilities, broad spectrum and misuse of antibiotics and other unhygienic conditions as compared to developed countries and the most sensitive drug was pipracillin+tazobactam and meropenem. This study correlates with the studies done at national level (Ejaz et al., 2011, Hannan et al., 2013). Spread of ESBL in our setting is mainly due to inappropriate infections control practices, contaminated intravenous catheters, feeding tube and various environmental surfaces (door handles, sucker machine, incubators, mattresses, wash basins, floor, sink, emergency trolley, ventilator, ambo bag, laryngeal scopes) and colonized hands of staff. Next major factor is the irrational use of antibiotics, use of broad spectrum antibiotics and substandard practices are very common (Hannan et al., 2013).
It is concluded from the current study that the most effective drugs against ESBL producing pathogens are meropenem and pipracillin+tazobactam and the prevalence such pathogens is gradually increasing in Pakistan and need special consideration.
The authors have not declared any conflict of interests.
REFERENCES
|
Ejaz H, Haq K, Zafa A, Mahmood S, Javed MM (2011). Urinary tract infections caused by extended spectrum β-lactamase (ESBL) producing Escherichia coli and Klebsiella pneumoniae. Afr. J. Biotechnol. 10:16661-16666.
|
|
|
|
Hannan A, Qamar MU, Usman M, Waheed KAI, Rauf K (2013). Multidrug resistant microorganisms causing neonatal septicemia: In a tertiary care hospital Lahore, Pakistan. Afr. J. Microbiol. Res. 7:1896-1902.
Crossref
|
|
|
|
|
Jamil I, Zafar A, Qamar MU, Ejaz H, Akhtar J, Waheed A (2014). Multi-drug resistant Klebsiella pneumoniae causing urinary tract infection in children in Pakistan. Afr. J. Microbiol Res. 8:316-319.
Crossref
|
|
|
|
|
Kausar A, Akram M, Shoaib M, Mehmood RT, Abbasi MN, Adnan M, Aziz DH, Asad MJ (2014). Isolation and Identification of UTI Causing Agents and Frequency of ESBL (Extended Spectrum Beta Lactamase) in Pakistan. Am. J. Phytomed. Clin. Ther. 2:963-975.
|
|
|
|
|
Liu HY, Lin HC, Lin YC, Yu SH, Wu WH, Lee YJ (2011). Antimicrobial susceptibilities of urinary extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae to fosfomycin and nitrofurantoin in a teaching hospital in Taiwan. J. Microbiol. Immunol. Infect. 44: 364-368.
Crossref
|
|
|
|
|
Mehrgan H, Rahbar M (2008). Prevalence of extended-spectrum beta-lactamase-producing Escherichia coli in a tertiary care hospital in Tehran, Iran. Int. J. Antimicrob. Agents 31:147-151.
Crossref
|
|
|
|
|
Peirano G, Pitout JD (2010). Molecular epidemiology of Escherichia coli producing CTX-M beta-lactamases: the worldwide emergence of clone ST131 O25:H4. Int. J. Antimicrob. Agents 35:316-321.
Crossref
|
|
|
|
|
Picozzi S, Ricci C, Gaeta M, Macchi A, Dinang E, Paola G, Tejada M, Costa E, Bozzini G, Casellato S, Carmignani I (2013). Do we really know the prevalence of multi-drug resistant Escherichia coli in the territorial and nosocomial population. Urol. Ann. 5:25-29.
Crossref
|
|
|
|
|
Picozzi SC, Casellato S, Rossini M, Paola G, Tejada M, Costa E, Carmignani L (2014). Extended-spectrum beta-lactamase-positive Escherichia coli causing complicated upper urinary tract infection: Urologist should act in time. Urol. Ann. 6:107-112.
Crossref
|
|
|
|
|
Potron A, Poirel L, Nordmann P (2015). Emerging broad-spectrum resistance in Pseudomonas aeruginosa and Acinetobacter baumannii: Mechanisms and epidemiology. Int. J. Antimicrob. Agents 45:568-585.
Crossref
|
|
|
|
|
Qamar MU, Hannan A, Arshad MU, Arshad M (2014). Metallo-β-lactamase producing Enterobacter cloacae: An emerging threat in neonates. Afr. J. Microbiol. Res. 8:525-528.
Crossref
|
|
|
|
|
Rawat D, Nair D (2010). Extended-spectrum beta-lactamases in Gram Negative Bacteria. J. Glob. Infect. Dis. 2:263-274.
Crossref
|
|
|
|
|
Shaikh S, Fatima J, Shakil S, Rizvi SM, Kamal MA (2015). Antibiotic resistance and extended spectrum beta-lactamases: Types, epidemiology and treatment. Saudi J. Biol. Sci. 22:90-101.
Crossref
|
|
|
|
|
Tanvir R, Hafeez R, Husnain S (2012). Prevalence and Multidrug resistant Escherichia coli in patients of Urinary Tract Infection Registering at Diagnostic Laboratory Lahore. Pak. J. Zool. 44:707-712.
|
|
|
|
|
Wikler MA, Cockerill FR, Bush K, Dudley MN, Eliopoulos GM (2012). Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Second International Supplement. P 32.
|
|