ABSTRACT
Extended spectrum beta-lactamases (ESBLs) are enzymes that are now becoming major sources of resistance to β-lactamase antibiotics more especially in enteric bacteria such as Klebsiella pneumoniae, P. aeruginosa and Escherichia coli. Increase in the frequency of the β-lactam resistance in bacteria has become a serious threat for treating bacterial infections caused by enterobacteriaceae. This study aims to determine the prevalence of ESBLs producers among enteric Gram negative bacteria isolated from patients in OAUTHC, Ile-Ife, Osun State. The subject used in this study involved patients presenting with evidence of hospital infections. The collected sputum specimens were processed for the isolation and identification of Gram negative bacilli. Resistance of the isolates to different antibiotics tested was determined using the standard disc diffusion method of Kirby-Bauer. Phenotypic and confirmatory test of the isolates were done for ESBL production using double disc synergy test (DDST) on Mueller Hinton agar according to CLSI 2013 guidelines. Results reveal that the highest occurrence of bacteria was recovered in Klebsiella species (35%), followed by Enterobacter sp. (13%), P. aeruginosa (10%), Escherichia coli and Salmonella sp. (7%) while the least occurs in Proteus sp. All the isolates were 100% resistance to class piperacillin, 76.6% to beta-lactamase inhibitor and 52% resistance to cephalosporins while they were susceptible to carbapenems, nitrofurans, and fluoroquinolones. The prevalence of ESBLs producing isolates was 51.1% while non-ESBL producing strains were 48.8%. Therefore, it can be concluded that extended spectrum beta lactamases are gradually increasing in Nigeria with co-resistance to some other classes of antibiotics which is very alarming. There is a limited number of drugs sensitivity for these bacteria and the drug of choice is imipenem, ciprofloxacin and ofloxacin.
Key words: Multidrug resistance, extended spectrum beta-lactamases (ESBLs), Gram negative bacteria
Extended spectrum β-lactamases (ESBLs) are beta-lactamases enzymes that are capable of conferring bacteria resistance to the penicillins, first, second and third generation cephalosporins, and aztreonam and those that do not confer resistance to the cephamycins or carbapenems groups of antibiotics. They confer resistance by hydrolysis of these antibiotics which are inhibited by β-lactamase inhibitors such as clavulanic acid, tazobactam or sulbactam, and they are encoded by genes that can be exchanged between bacteria (Paterson and Bonomo, 2005; Shaikh et al., 2015). The first ESBL was identified by Knothe et al. (1983) in a nosocomial Klebsiella pneumoniae strain isolated in Germany in 1983 since then over 500 variants of the clavulanic acid-inhibited form (TEM, CTX-M, SHV, OXA) have been described worldwide (Kiratisin et al., 2008). They are most prevalent in Klebsiella sp and their epidemiology reflects a mixture of mutations, plasmid transfer and or clonal spread (Livermore and Woodford, 2006). The most common ESBL phenotypes arise from point mutations in the blaTEM ,blaSHV, or blaCTX genes resulting in alteration of the primary amino acid sequence of the enzyme (Bradford, 2001; Gniadkowski, 2001; Paterson and Bonomo, 2005; Paterson, 2006). In the past years there has been an increase in the incident of extended spectrum beta lactamase infections and those related to ESBL infections. This study has been carried out to examine the occurrence of ESBLs among Gram negative isolates from patients with respiratory tract infections.
The study was conducted on in-patients and out-patients attending Obafemi Awolowo University Teaching Hospital Complex (OAUTHC). Ethical approval was obtained from the Hospital Ethical and Research Committee of the institution. Sputum samples were collected aseptically from subjects between the period of January, 2015 and February, 2016. Sample size was determined using Cochran’s formula of N= Z2 pq/d2 (Bartlett et al., 2001). In all, a total of 471 enteric bacteria isolates (Gram-negative) were collected altogether from both inpatients and outpatients. The morphological and conventional methods of the bacteria strains were done and confirmation of the bacteria was determined by biochemical test and with the use of API 20E kit. (API Bio Merieux, Germany). The resistance of isolates to different antibiotics was done using the method of Kirby-Bauer standard disc diffusion method.
Extended spectrum beta-lactamase production from the isolates were screened by using disc diffusion of cefotaxime (CTX) and ceftazidime (CAZ) placed on Muller Hinton agar plate seeded with the isolates according to the CLSI recommendations. Phenotypic confirmatory test for ESBL positive strains were determined by double disc synergy test (DDST) for all the ESBL producing isolates using CLSI (2015) guidelines. Bacterial colony was re-suspended in nutrient broth to 0.5 McFarland standards and was inoculated directly on a Mueller-Hinton agar plates. Single discs containing ceftazidime with and cefotaxime was placed center to center, 25 mm apart to the amoxycillin/clavulanic acid (20/10 μg) disc on a lawn culture of the isolate on Mueller-Hinton agar plate. The plates were then incubated at 37°C for 18 - 24 h. An enhanced cleared zone of inhibition towards the amoxycillin/clavulanic acid (20/10 μg) disc showed positive ESBL production (Iroha et al., 2009).
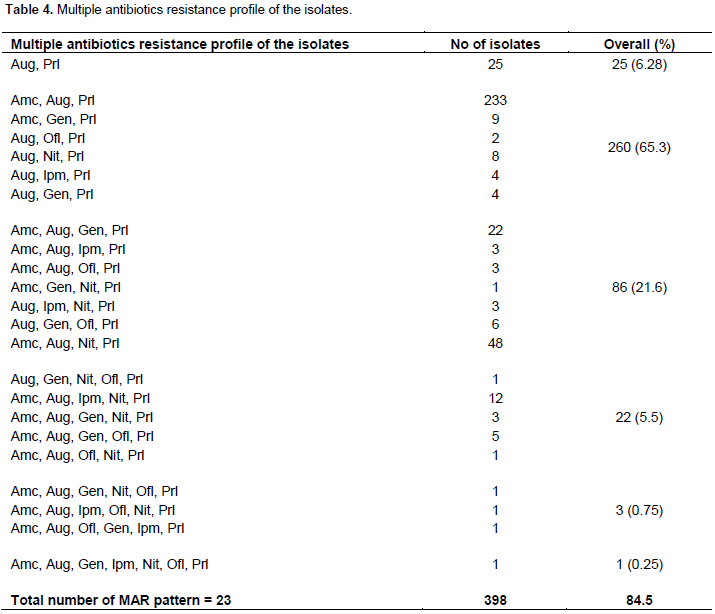
Four hundred and seventy-one enteric Gram-negative bacteria which consist of thirty-two different species were recovered from patients with respiratory tract infection. They are K. pneumoniae, Citrobacter freundii, Escherichia coli, Proteus mirabilis, Aeromonas salmonicida, Serratia liquefaciens and Salmonella arizonae. Out of four hundred and seventy-one (471) isolates, 241 (51%) isolates produced extended spectrum beta-lactamase, while 230 (49%) were not extended spectrum beta-lactamase producers (Table 1). The ESBL producers are 51% while non-ESBL producing strain are 48.8% (Table 2). Most of the ESBL-producers were multiple drug resistant to piperacillin, augmentin, ceftazidime, cefoxtazime, cefuroxime, cefixime and beta lactam inhibitor, 95.6 and 96.4% of isolates were found sensitive to imipenem and ofloxacin respectively while other isolates showed resistance to piperacillin (100%) (Table 3). The multiple antibiotic resistance (MAR) phenotypes of bacterial isolates recovered from patients diagnosed with LRTI in Ile-Ife showed diversities of MAR patterns which occurred among the isolates (Table 4).
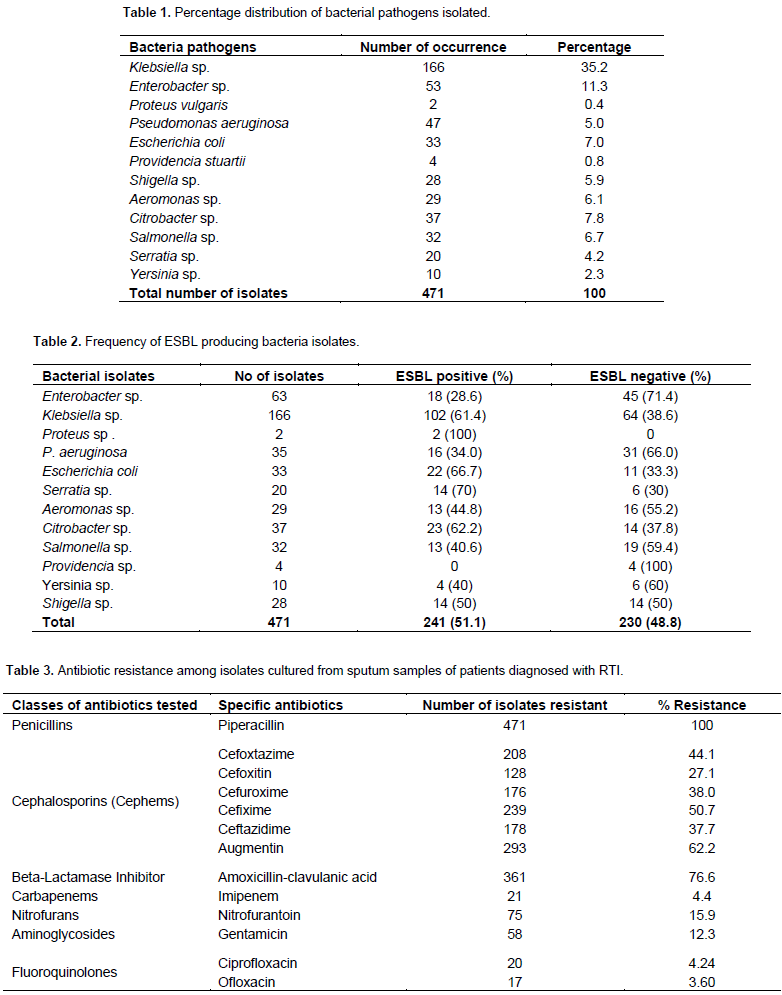
The antibiotic resistance among the respiratory pathogens is a major barrier that might interfere with an effective treatment. The emergence of multidrug resistant strains poses a major threat to the patients globally. Among the isolates, various mechanisms of antibiotic resistance have been attributed, among which production of beta-lactamases is a leading cause of resistance. Extensive use of broad spectrum antibiotics has further increased the multidrug resistance. Carbapenem-hydrolyzing beta-lactamases of Ambler class B (metalloenzymes), Ambler class D (oxacillinases) and extended-spectrum beta-lactamases (ESBLs) of Ambler class A are sources of multidrug resistance in Gram-negative isolates (Noyal et al., 2009). In this study, two hundred and forty-one (51.1%) bacterial isolates were extended spectrum beta-lactamases producers. Sherchan et al. (2012) reported 20% ESBL production among the Gram-negative isolates which is in contrast to this present study. Statistically, there were no significant differences (P>0.05) among the ESBL producers and non-ESBL producers.
The emergence of these ESBLs in Gram-negative bacilli is becoming a therapeutic challenge. Carbapenem group of antibiotics play a vital role in the management of Gram-negative infection, because of their broad spectrum activity and stability to hydrolysis by most of the beta-lactamase including ESBLs (Sherchan et al., 2012). Another finding in this study was that the isolates showed low level of susceptibility to third generation cephalosporins such as cefotaxime, ceftriazone, and ceftazidime, that is, they were highly resistant to third generation cephalosporins. This may be due to the fact that many of the organisms are ESBL producers which are evident from these findings as they showed ESBL production at a very high rate, especially in Klebsiella spp, E. coli and P. aeruginosa. Other reason may be that the third generation cephalosporins antibiotics have been misused for a long period by individuals, so that over this time pathogens have developed and become resistance.
The misuse of broad spectrum antibiotics, insufficient hygiene, immunosuppression, and a prolonged stay in the hospital are some other major aetiological factors that enhance the chances of multi drug resistant infections (Manjunath et al., 2011). Studies from Indian and Nigeria reported high level of resistance (87 - 89%) and (84.8 - 96%) respectively to cephalosporins (Egbebi and Famurewa, 2011; Gupta et al., 2012). The decreased susceptibility of third generation cephalosporins could also be due to production of ESBL and AmpC beta-lactamases. In the present study, 23.4% isolates were sensitive to amoxicillin-clavulanic acid. Such low level of sensitivity has also been reported in other Indian studies stating 49.3% to as low as 9% (Gupta et al., 2012; Namratha et al., 2015).
The prevalence and incidence of respiratory infections has been on the increase side, which are caused by beta lactam resistant organisms and due to the production of different enzymes has increased recently. Detection of strains producing ESBL is of paramount importance in both hospital acquired and community acquired isolates. The close monitoring of this pathogens in laboratories is required to minimize the spread of these bacteria and help to select appropriate antibiotics to combat them. The detection of extended spectrum beta lactamase producing isolates in the study area are multidrug resistance; thus, there is a need for constant and careful surveillance for multidrug-resistant bacteria in the study area.
The authors have not declared any conflict of interests.
REFERENCES
|
Bartlett JE, Kortrijk JW, Higgins C (2001). Organizational research: Determining appropriate sample size for survey research. Inform. Technol. Learn. Perform. J. 19:43-50.
|
|
|
|
Bradford PA (2001). Extended-spectrum beta-lactamases in the 21st century: Characterization, epidemiology, and detection of this important resistance threat. Clin. Microbiol. Rev. 14(4):933-951.
Crossref
|
|
|
|
|
Egbebi O, Famurewa O (2011). Antibiotic resistance of Klebsiella isolated from some hospitals in southwest Nigeria to third generation cephalosporins. Adv. Trop. Med. Public Health Int. 1(3):95-100.
|
|
|
|
|
Gniadkowski M. (2001). Evolution and epidemiology of extended-spectrum β- lactamases (ESBLs) and ESBL-producing microorganisms. Clin. Microbiol. Infect. 7:597-608.
Crossref
|
|
|
|
|
Gupta V, Kumarasamy K, Gulati N, Garg R, Krishnan P, Chander J (2012). AmpC β-lactamases in nosocomial isolates of Klebsiella pneumoniae from India. Indian J. Med. Res. 136(2):237-241.
|
|
|
|
|
Iroha IR., Egwu OA, Ngozi AT, Chidiebube NA, Chika EP (2009). "extended spectrum beta–lactamase (ESBL) mediated resistance to antibiotics among Klebsiella pneumonia in Enugu metropolis" Macedonia J. Med. Sci. 2:196-199.
|
|
|
|
|
Kiratisin P, Apisarnthanarak A, Laesripa C, Saifon P (2008). Molecular Characterization Epidemiology of Extended-Spectrum-b -Lactamase-Producing Escherichia coli and Klebsiella pneumoniae Isolates Causing Health Care-Associated Infection in Thailand, Where the CTX-M Family is Endemic. Antimicrob. Agents Chemother. 52:2818-2824.
Crossref
|
|
|
|
|
Knothe H, Shah P, Krcmery V., Antal M, Mitsuhashi S. (1983). Transferable resistance to cefotaxime, cefoxitin, cefamandole and cefuroxime in clinical isolates of K. pneumoniae and Serratia marcescens. Infection 11:315-317.
Crossref
|
|
|
|
|
Livermore DM, Woodford N. (2006). The β-lactamase threat in Enterobacteriaceae, Pseudomonas and Acinetobacter. Trends Microbiol. 14:413-420.
Crossref
|
|
|
|
|
Manjunath GN Prakash R Vamseedhar A, Kiran S (2011). The Changing Trends In The spectrum of the antimicrobial drug resistance pattern of uropathogens which were isolated from hospitals and community patients with urinary tract infections in Tumkur and Bangalore. Int. J. Biol. Med. Res 2(2):504-550.
|
|
|
|
|
Namratha K G, Padiyath S, Subbannayya K, Dinesh PV, Hemachandra C (2015) Characterization and Antibiogram of Klebsiella spp. Isolated from Clinical Specimen in a Rural Teaching Hospital. Scholar J. Appl. Med. Sci. 3(2E):878-883.
|
|
|
|
|
Noyal MJC, Menezes GA, Harish BN, Sujatha S, Parija SC (2009). Simple screening tests for detection of carbapenemases in clinical isolates of nonfermentative Gram-negative bacteria. Indian J. Med. Res. 129:707-712.
|
|
|
|
|
Paterson DL (2006). Resistance in Gram-negative bacteria: Enterobacteriaceae. Am. J. Infect. Contr. 34:S20-28.
Crossref
|
|
|
|
|
Paterson DL, Bonomo RA (2005). Extended-spectrum β-lactamases: a clinical update. Clin. Microbiol. Rev. 18:657-686.
Crossref
|
|
|
|
|
Shaikh S., Jamale FJ, Shakil S, Syed MS, Danish RD, Mohammad A, Kamal MA (2015). Antibiotic resistance and Extended Spectrum Beta-lactamases: Types, epidemiology and treatment. Saudi J. Biol. Sci. 22:90-101.
Crossref
|
|
|
|
|
Sherchan JB, Gurung P, Bam DS, Sherchand JB (2012) Multi-Drug Resistant Bacterial Strains in Lower Respiratory Tract Infections, Antibiotic Sensitivity Patterns and Risk Factors. Nepal J. Sci. Technol 13:1:157-163.
|
|