ABSTRACT
Vasectomy is a method of family planning which is quite acceptable in many developed countries of the world. However, in most African countries, there are still existing barriers to its adoption by married men. This study was therefore designed to explore the antecedent factors related to the adoption of vasectomy among married men in eight (8) peri-urban communities of Ibadan, Nigeria. Four hundred and thirty one men selected using multi-stage sampling technique were interviewed in a household survey using the cross sectional study design. Mean age of the respondents was 44 ± 13.2 years, 13.5% of the respondents had reportedly heard about vasectomy, 30.8% considered it an unacceptable method of contraception while 16.2% see it as a sin against God. Barriers to the adoption of vasectomy included fear of the surgery and its side effects (26%), indifference to family planning (23%), its irreversibility (19%), personal beliefs (10%), lack of evidence that it works (8%), lack of awareness (7%), financial constraints (3%) and inadequate health system (2%). Only 29.7% had intention to adopt vasectomy as a means of birth control. Intention to adopt vasectomy was significantly associated with age (p<0.05). Awareness of vasectomy as a birth control method and intention to adopt it were low. Public enlightenment to provide correct and adequate information, education, and communication (IEC) using appropriate health promotion strategies aimed at increasing awareness and benefits of vasectomy are advocated.
Key words: Antecedent factors, vasectomy, married men, peri - urban communities.
Nigeria is one of the most populated countries in Africa, with an estimated 165 million people as at 2014, and a total fertility rate of 5.5 (NPC and ICF international, 2014). With the current population growth rate, Nigeria is expected to double its population in the next two decades (United Nations, 2015). This comes with its attendant socio-economic challenges. Unfortunately, use of family planning methods remain low in the entire population as only 15% of currently married women aged 15 to 49 use any form of contraception and only 10% reported using a modern method (NPC, 2006 and ICF International, 2014). This is in spite of the existence of the national policy on population and sustainable development which encourages voluntary limitation of births to four children per woman as well as utilization of various family planning methods.
The use of the two male-oriented contraceptive methods, the condom and vasectomy is low compared to the use of other methods, but it is slowly increasing in some countries (Ezegwui and Enwereji, 2009). In most countries, traditional methods that require male cooperation, the withdrawal and abstinence methods are also less utilised. Worldwide, condoms and vasectomy are among the least used of all the contraceptive methods (NPC and ICF International, 2014; Tolassa, 2004).
Vasectomy is the only currently available method other than condoms that allows the man to take responsibility for preventing pregnancy (Kogan and Moshe, 2014). It is more common than female sterilization in only five countries of the world, namely: Bhutan, Canada, the Netherlands, New Zealand and Great Britain. New Zealand has the highest vasectomy prevalence among married couples of reproductive age at 20% (Population Reference Bureau (PRB), 2008). World vasectomy use significantly varies by region and country; despite its many advantages, vasectomy is used in only a few countries, this includes China, India, Thailand, Korea, the United Kingdom, Canada and the United States. About three-fourth of the 37 million couples who use vasectomy live in Asia; China and India alone account for more than two-third of this number. In the other developing countries, only 4.5million men use vasectomy (UN, 2005). Inspite of the introduction of vasectomy in some African countries such as Ghana, Kenya, Malawi and Tanzania, vasectomy rates in all of Africa are still less than 0.1% (Tsai, 2011; Jacobstein and Pile, 2007).
In many developing countries, men hold several misconceptions about vasectomy and the procedure is not widely available. Even if it is available and men have heard of it, many incorrectly believe that the procedure affects a man’s sexual functioning and weakens his strength. Vasectomy is a safe, cost effective and permanent method of contraception, but there are many factors that play a role in its relative lack of acceptance, such as socio-demographic factors, economic factors, low social support and inaccurate knowledge and belief about the procedure (Mahat et al., 2010). Incorrect information and unfounded fears often limit its use, even in countries where the procedure is readily available.
In Nigeria, few studies have explored the perceptions of men towards vasectomy. Given the critical role that men play in family decisions; their support, involvement and understanding their reproductive intentions are essential for family planning to become more widespread. In addition, a growing number of family planning and other reproductive health care programmes and providers now understand that men deserve more attention for their own sakes, for women’s sake and for the health of their families and communities. There is currently no record of the number of male initiated contraceptive methods in Nigeria (NPC and ICF International, 2014). A strategy to promote men’s involvement in effective birth control is needed to reduce the population growth and to ameliorate the resultant health, social and economic challenges. Men’s participation in issues related to reproductive health especially family planning, is a promising strategy for addressing some of these pressing reproductive health problems (Akpamu et al., 2010). Furthermore, there is a dearth of information on the awareness and intention to adopt vasectomy. This research therefore sought to find out what the awareness of married men about vasectomy is, barriers to its uptake and intention to adopt it by married men, in typical indigenous Nigerian communities.
Study design
This household survey which utilised the cross-sectional study design was carried out among married men aged 25 years and above living in the three socio-economic and developmental (inner core, transitional and peripheral) strata of Ibadan South East Local Government Area, Oyo state, Nigeria.
Study population
The study participants were recruited from selected households in the communities who provided informed consent to participate in the study. According to the 2006 population census, the population of the Local Government Area (LGA) was 266,457; 131,150 (49.2%) were males while 135,307(50.8%) were females.
Study setting
The population density of the local government is calculated to be 2832 persons per kilometer. The LGA has 12 political wards, each of which has a political head (councilor). Though the population census on ward basis was not available at the time of study, observations indicate that the core areas of the local government are more densely populated than other areas. Low and medium income people largely reside in the community and Yoruba is the predominant ethnicity.
Sampling
The sample size was determined using an assumed prevalence of 50% for awareness of vasectomy and 95% confidence interval and 80% power. The minimum calculated sample size for the survey was approximately 385 which was increased by 10% to cover for attrition or loss of questionnaire. A multistage sampling approach using a combination of stratified, systematic and simple random sampling techniques was used for recruitment of respondents for the study. According to the settlement pattern, the LGA was divided into inner-core, transitional and peripheral areas. There were eight wards in the inner-core, three in the transitional and only one in the peripheral areas of the LGA. Seven wards were chosen by simple random sampling; four out of eight in the innercore, two out of the three in the transitional and the only one in the peripheral areas of the LGA. Based on the proportional population ratio of 3:2:1 and a systematic sampling of houses was performed sequentially using every second interval; 210 houses were selected from the inner-core, 145 from the transitional and 76 from the peripheral areas. One head of household was randomly selected from the households in each house to make up a total of 431 household heads.
Data collection procedure
A pretested semi-structured, interviewer-administered questionnaire was used to collect quantitative data on the awareness of, barrier towards and intention to practice vasectomy as a family planning method. The instrument which was designed in English was translated to Yoruba, the main language of communication within the LGA, and translated back to ensure consistency of information. Data collection was carried out by four trained male research assistants using face - to - face interview among married men in the selected wards. Verbal consent was obtained from each of the respondents before commencement of the interview. Data collection was done in the late afternoon and evenings, between 15 and 20 h time, when most of the heads of households would have returned from their different places of work. The instrument was designed in conformity to the ethical law of confidentiality and anonymity. Each questionnaire was checked for inconsistency by the principal investigator at the end of each day. All questionnaires were collated and numbered after each day on the field. Questionnaires were given to research assistants on a daily basis before administration, to ensure it had not been pre-filled.
Data analysis
A coding guide was developed for all open-ended questions and was entered into the computer using the Epi-info version 6 software. Frequencies of all variables were generated to check for any error or missing data, where after data cleaning was carried out. Data presentation was in varying descriptive representation such as tables and charts and inferential statistics. Descriptive statistics were presented using frequencies, means and standard deviations (SD). Test of association between the dependent and independent variables were conducted using chi-square, and p-value of <0.05 representing significance levels.
Socio demographic characteristics
The details of socio-demographic characteristics of the respondents are outlined in Table 1. Mean age of the respondents was 44 ± 13.2 years. Almost all, 95.8% were married and living with their spouses, 63.1% of those who are married were in monogamous marriages with 23.7% of those in polygynous marriages having two wives. Majority of the respondents (97.4%) were Yoruba in ethnicity.
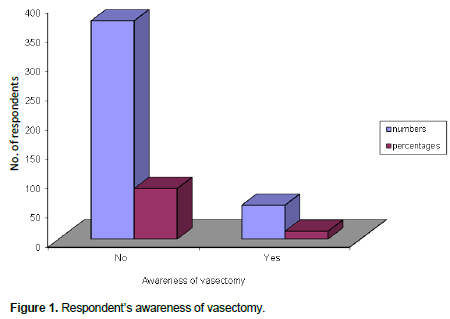
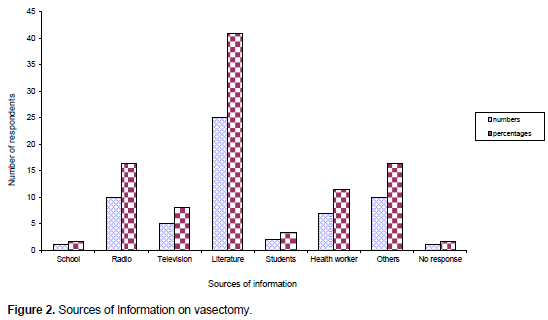
Awareness of Vasectomy
As shown in Figures 1 and 2, only 58(13.5%) of the respondents reported having heard about vasectomy, the majority (86.5%) had not. The main sources of information about vasectomy were literature (book, pamphlets) 25 (41%) and radio (16.4%).
Barriers to adopt vasectomy
Many of the respondents (30.8%) considered vasectomy a ‘bad’ method of contraception while (16.2%) saw it as a sin against God (Table 2). Barriers to the adoption of vasectomy included fear of the surgery and its side effects (26%), indifference to family planning (23%), its irreversibility (19%), personal beliefs (10%), lack of evidences (8%), lack of awareness (7%), financial constraints (3%) and inadequate health system (2%).
Factors influencing respondent’s awareness of vasectomy
As stated in Table 3, there is a significant relationship between respondents’ awareness of vasectomy and their places of residence; more people in the peripheral areas were aware of vasectomy compared to those in other areas (p= 0.014). There is a significant relationship between the educational status of respondents and their awareness of vasectomy; respondents with higher (tertiary and secondary) education had heard of vasectomy than those with lower education (p=0.000).
There is also a significant relationship between respondents’ occupation and their religion regarding their awareness of vasectomy; more of the professionals were aware of the procedure compared to those in the other occupational groups do (p=0.000).
Intention to adopt vasectomy
Table 4 indicates the intention of respondents to adopt vasectomy for family planning. A third, 128 (29.7%) of the respondents had intention to adopt vasectomy for family planning. Table 5 showed that intention to adopt vasectomy was significantly related to respondent’s age (p=0.03). There was no significant relationship between respondents’ place of residence (p=0.98), marital status (p=0.48), occupation (p=0.54) ethnic group (p=0.87) and their intention to adopt vasectomy. Out of all the respondents only 2(0.5%) reported they have had vasectomy.
Vasectomy awareness among men was low (13.5%), the main sources of information were literature and health workers. Fewer respondents in this study, knew about vasectomy, periodic abstinence and vaginal methods; this finding is consistent with a qualitative study among married men and women in California, United States of America, carried out by Shih et al. (2013) in which most men reported a lack of counseling about both female and male sterilization and contraception in general. In consonance with the study carried out in Ghana, respondents who have heard about vasectomy mostly reported literature and health workers as their major source of information (Owusu-Asubonteng et al., 2012). Residents who lived in urban (peripheral areas) were more likely to be aware of vasectomy. This cannot be isolated from the fact that most people living in the urban peripheral areas were those with higher educational attainment and would most likely be engaged in professional occupations. This is very much in agreement with the study carried out in Iran (Keramat et al., 2011) where most of the subjects who had heard of vasectomy shared characteristics with respondents in the current study.
In agreement with the current study carried out among resident gynaecologists in a Nigerian University (Ebeigbe et al., 2011), quite a number of myths and misconceptions constitute barriers to the use of vasectomy by married men in a typical Nigerian community. These included intolerance of the method due to religious and moral norms including fears associated with surgery, impotence, diseases and perceived inadequacy of the health system in these communities. In the RESPOND project carried out among married men and women in Uttar Pradesh, fears about weakness resulting from the procedure were common among both men and women and served as one of the main barriers to acceptance of non-scapel vasectomy (Scott et al., 2011). Oyediran et al. (2002) in a study conducted among married men in Nigeria stated incorrect and incomplete information including misconceptions that: Men do not care about avoiding pregnancy, they prize their fertility, they think wrongly that vasectomy will end their manhood, they unreasonably fear minor procedure, and that they put all responsibility of family planning on women as barriers to vasectomy among them. This may be the major reason why only one third of the respondents indicated their intention to adopt the method in the near future. Many of the respondents, 176 (40.8%) suggested that use of mass-media for public enlightenment would likely increase awareness of vasectomy among men.
The study assessed the antecedent factors related to the intention to adopt vasectomy for family planning among married men in Ibadan. The majority of the men surveyed had limited awareness of vasectomy as a method of family planning and few had intention to adopt it due to misconceptions about the procedure. The main reason for low levels of use may not lie in men’s attitude alone but also in policy-makers’ and providers’ lack of attention to vasectomy and cultural acceptability of the procedure, especially among African men and Nigerian in particular.
Providing correct and adequate information, education, and communication (IEC) about reproductive health is key to gaining men’s interest and support for vasectomy. In view of these, several health promotion and education strategies such as training of family planning service providers and public enlightenment may be employed to bring about a positive behavioural change by men to adopt vasectomy as a method of contraception in an attempt to get men more involved and ensure their participation in family planning.
The authors have not declared any conflict of interests.
The authors of this research wishes to appreciate the contribution of data collectors to the success of the research. They are also very grateful to all the respondents for consenting to participate in the research.
REFERENCES
|
Akpamu U, Nwoke EO, Osifo UC, Igbinovia ENS, Adisa AW (2010). Knowledge and Acceptance of 'Vasectomy as a Method of Contraception' amongst Literate Married Men in Ekpoma, Nigeria. Afr. J. Biol. Res. 13:2.
|
|
|
|
Ebeigbe PN, Igberase GO, Eigbefoh J (2011). Vasectomy: A Survey of Attitudes, Counseling Patterns and Acceptance among Nigerian Resident Gynaecologists. Ghana Med. J. 45(3):101-4.
|
|
|
|
|
Ezegwui HU, Enwereji JO (2009). Attitude of men in Nigeria to vasectomy. Int. Health 1(2):169-72.
Crossref
|
|
|
|
|
Jacobstein R, Pile JM (2007). Vasectomy: The Unfinished Agenda ACQUIRE Project Working Paper Engender Health. USAID, New York. pp. 1-12.
|
|
|
|
|
Keramat A, Zarei A, Arabi M (2011). Barriers and facilitators affecting vasectomy acceptability (a multi stages study in a sample from north eastern of Iran), 2005-2007 Asia Pac. Fam. Med. 10:5.
Crossref
|
|
|
|
|
Kogan P, Moshe W (2014). Male Contraception: history and development. Urol. Clin. N. Am. 41(1):145-61.
Crossref
|
|
|
|
|
Mahat K, Pacheun O, Taechaboonsermsak P (2010). Intention to Accept Vasectomy among Married Men in Kathmandu, Nepal. Asia J. Public Health 1(1):8-13.
|
|
|
|
|
National Population Commission (NPC) (2006) Federal Republic of Nigeria, 2006 Population Distribution by Age, Sex and Marital Status. Census Priority Table 5:1-371.
|
|
|
|
|
National Population Commission (NPC) and ICF International (2014). Nigeria Demographic and Health Survey 2013. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF International.
|
|
|
|
|
Owusu-Asubonteng G, Dassah ET, Odoi AT, Frimpong P, Ankobea FK (2012). Trend, client profile and surgical features of vasectomy in Ghana. Eur. J. Contracept. Reprod. Health Care 17(3):229-36.
Crossref
|
|
|
|
|
Oyediran KA, Ishola GP, Feyisetan BJ (2002). Factors affecting ever-married men's contraceptive knowledge and use in Nigeria. J. Biosoc. Sci. 34(4):497-510.
Crossref
|
|
|
|
|
Population Reference Bureau (PRB) (2008). Family planning worldwide 2008 data sheet. In: Washington DC PRB, ed.
|
|
|
|
|
Scott B, Alam D, Raman S (2011). Factors affecting acceptance of vasectomy in Uttar Pradesh: Insights from community-based, participatory qualitative research. The Respond Project Study Series: Contributions to Global Knowledge-Report No, 3. Available at:
View
|
|
|
|
|
Shih G, Dubé K, Dehlendorf C (2013). We never thought of a vasectomy": a qualitative study of men and women's counseling around sterilization. Contraception 88(3):376-81.
Crossref
|
|
|
|
|
Tolassa Y (2004). The Role of Men in Family Planning in a Rural Community of Western Ethiopia. A Thesis Submitted to the School Of Graduate Studies, Addis Ababa University in the Partial Fulfillment of the Requirement for the Degree of Masters of Public Health.
|
|
|
|
|
Tsai T (2011). Vasectomy an option for African men in Family Planning. Population Reference Bureau (PRB) Report. Dec. 11. Available at:
View
|
|
|
|
|
United Nations (UN) (2005). World contraceptive use 2005, Wall chart. New York.
|
|
|
|
|
United Nations (UN) (2015). Department of Economic and Social Affairs - Population Division - World Population Prospects, the 2015 Revision.
|
|