ABSTRACT
Antenatal depressive disorders are serious health problems and pose multiple dangers to both the mother and her fetus, however, not given due attention. They are found with significantly higher prevalence rates in low income countries and associated with socio-economic and socio-cultural factors predominantly. The main objective of this study was to assess the prevalence of antenatal depressive disorders and associated factors among Adama Hospital Antenatal clinic attendants. A hospital based cross sectional study was conducted from March 1st to April 21st, 2011 at Adama Hospital, Adama, Ethiopia. About 231 pregnant women were interviewed using systematic sampling method. Pretested Beck Depression Inventory (BDI) structured questionnaire was used to collect data. The presence of depressive disorders was explained by the sum of BDI items scored 21 and above. And, data entry was done by SPSS version 15 and analyzed using logistic regression. The mean age was 26.32±0.24. About 56.7% were in third trimester and 45% were nulliparous. Regarding pattern of current pregnancy, unwanted pregnancy accounted 42%. Prevalence rate of antenatal depressive disorders was found to be 31.2%. Previous abortion [AOR=2.86, CI (1.13, 7.24)], fear of pregnancy complications [AOR=3.49, CI (2.21, 22.17)], economic problem [AOR=9.52, CI (2.68, 33.78)] and unwanted pregnancy [AOR=6.99, CI (2.21, 22.17) and marital conflict [AOR=22.68, CI(3.61, 142.33] were found to have strong association with depressive disorders. The prevalence of antenatal depressive disorders was high at the study area. Psychosocial factors, economic problems and obstetric features were significantly associated with maternal depressive disorder. Adama Hospital should integrate mental health service with existing antenatal clinic service. In addition, screening of antenatal care (ANC) attendants for potential risk factors of antenatal depressive disorders could be crucial to hamper the impending dangers through early detection.
Key word: Antenatal depressive disorders, pregnant women, Adama hospital, beck depression inventory.
Antenatal depressive disorders are significant health problems; especially in low and middle income countries (Das, 1994). Though reports on prevalence rates lack consistency, substantial higher rates are from developing countries (Felice et al., 2008).
A systemic review of 15 counties reported 32.2% prevalence rate of antenatal depressive disorders. This may even be higher among high risk groups; within the range of 38 to 50 % (Bennettt et al., 2004; Nasreen et al., 2010). Standard survey was carried out on ten Michigan Obstetric units and the report viewed 20% prevalence rate (Marcus et al., 2003). Another study conducted among rural and urban pregnant women at Ankara antenatal settings found prevalence of 33.1% (Senturk et al., 2011). And also; a hospital based study in Hong Kong took the samples at the antenatal clinic and revealed 37% prevalence of depressive symptoms (Lee et al., 2007).
Unlike the commonly reported findings from developing countries, a recent community based study in Nigeria showed prevalence rate of 8%. However; there is paucity of information on antenatal depressive disorders from Africa. And, no available studies were carried out at health institutions (Adewuya et al., 2007).
Antenatal depressive disorders were found in association with some factors; marital conflict, economic problems, poor support from husband, unwanted pregnancy, previous abortion and past obstetric complications (Adewuya et al., 2007; Kaaya et al., 2010; Dayan et al., 2010). History of past psychiatric disorders, chronic medical illness and poor antenatal care were also reported (Rubertsson et al., 2005; Pereira et al., 2009); however, controversies in the data exist (Hartley et al., 2011; Nasreen et al., 2011; Sawyer et al., 2010).
Pregnant women with antenatal depressive disorders are at risk for recurrent spontaneous abortions, obstetric complications, postnatal depressive disorders and poor child rearing capacity. Babies are also at increased danger for intrauterine growth retardation, preterm delivery, impaired postnatal growth and frequent infant diarrheal diseases (Stewart et al., 2010; Deyessa et al., 2010). Moreover; such women are in danger of troubled social functioning and immune related disease states (Hart and Mahon, 2006; Stein et al., 1991).
Assessment of psychosocial problems and mental health is an integral part of antenatal services to ensure safe pregnancy and delivery. But developing countries lack such antenatal care (ANC) services; and even if available, lack coverage, quality or support from stake holders. In accordance with this fact, a study at Nottingham University notified that WHO has formulated a focused ANC guideline including women’s mental health package to be used during ANC assessment (Menon et al., 2010).
In addition to lack of available reports both at national and local study area of this study, higher prevalence rate of antenatal depressive disorders occur at health care settings; therefore, the purpose of this study was to assess the magnitude of antenatal depressive disorders and identify predictors of Antenatal Depressive symptoms among Adama Hospital antenatal clinic attendants.
Study design
Institutional based cross-sectional study design was used.
Study area and period
Adama Hospital is found in Adama town; East Shoa, about 99 km away from Addis Ababa. The Hospital is used for practical teaching of accelerated health officers, clinical nurses, and midwifery, laboratory and pharmacy students at BSc and diploma level besides serving the community. Antenatal care is one of the hospital services organized under health promotion case team. All pregnant mothers who visited the clinic were given appointment for re-visit accordingly. Pregnant mothers were allowed to come back to the clinic at any time on working days and hours for perceived emergency signs and symptoms of pregnancy complications. There was only one midwifery nurse carrying out the ANC services.
The ANC service is organized since establishment of the hospital. There was one psychiatry outpatient department. The system for mental health has no link with antenatal clinic; hence no access of integrated activities for pregnant ladies suffering from mental problems. The study was conducted from March 1st to April 21, 2011.
Study population
Pregnant women attending antenatal clinic within the study period, whose pregnancy was at least 16 weeks (4 months) and below 37 weeks.
Exclusion criteria
1. Those previously diagnosed for depressive disorders
2. Critically ill ones
3. Who were on treatment for mental disorders
Sample size determination and sampling procedures
Single population formula was used with the assumption of 95% confidence interval, precision (d) of 0.03, proportion 8% from the study done in Nigeria and adding 10% non-response rate, 243 women were participated in the study. Systematic sampling procedure was used to interview the study subjects. Every third pregnant woman was approached for the interview during follow up period until the required sample size fulfilled.
Study variables
1. Dependent variable: Antenatal depressive disorders
2. Independent variable: Age, educational level, occupation, marital status, level of monthly income, marital conflict, history of abortion, unplanned pregnancy, fear of pregnancy complications, poor husband support, number of live children, perceived poor antenatal care.
Operational definition
Depressive disorders
The presence of depressive disorders was explained by the sum of BDI items scored 21 and above.
Data collection method and quality assurance
Data was collected by interview technique using standardized and validated Beck Depression Inventory (BDI) and structured questionnaire after translated in to Amharic.
BDI was developed and revised to reflect the revision in the current DSM-IV-TR and had been extensively tested for content validity. BDI was composed of 21 questions, each with four possible responses. Each response was assigned a score ranging from zero to three, indicating severity of a symptom. Two BSc nurses supervisor and three diploma clinical nurses data collectors were recruited. Training was given for data collectors and supervisors before data collection and then pretest was done to avoid errors during the actual data collection period. The data was checked daily by supervisors.
Data analysis
All returned questionnaires were checked for completeness and consistency. Data was coded and then entered, cleaned, stored and analyzed using SPSS 15. Descriptive analysis was used to depict frequency and percentages of variables. Logistic regression was used to find out association between depressive disorders and suggested related factors and strength of association was evaluated using odds ratio at 95% confidence interval and P-values 0.05 was considered to declare significant associations.
Ethical consideration
Ethical approval was obtained from Adama Hospital ethical committee after having authorized letter from University of Gondar and Amanuel Specialized Mental Hospital. All antenatal clinic attending mothers were approached and subjects who gave written consent were interviewed. The interview was conducted in a single separate room around the antenatal clinic. Confidentiality was maintained through no registration of personal identification. Subjects identified with depressive disorders were advised to visit the psychiatric clinic and given referral.
A total of 231 pregnant women were interviewed and has 95% response rate. The mean age was 26.32 + 0.24. Regarding their level of education; unable to read and write was 7.8%, read and write to primary school were 30.8%, secondary school was 44.2% while higher education constituted 17.7%. Majority (82.3%) was married and house wife (58%). Prevalence rate of antenatal depressive disorders was found to be 31.2%. About 56.7% were in third trimester and 45% were nulipara. A total of 37.8% had history of abortion. Unwanted pregnancy accounted 42% (Table 1).
Overall, 55% stated pregnancy is not joyful for them and 16.9% respondents explored they have poor husband support. About 16% reported their husbands are not happy on the occurrence of current pregnancy (Table 2).
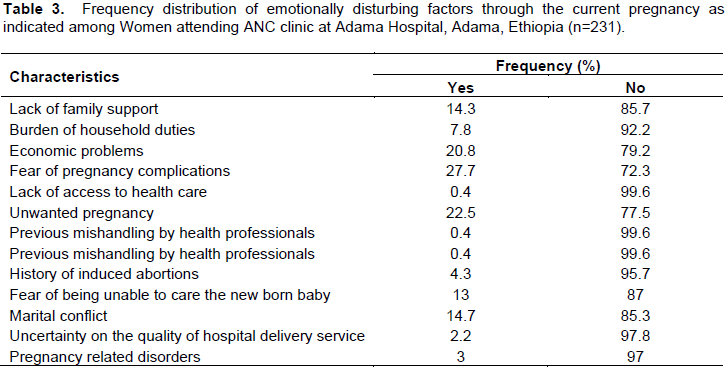
Participants were made to indicate or choose factors at which they mostly worry about through the current pregnancy. Accordingly; fear of pregnancy complications 27.7%, unwanted pregnancy 22.5% and economic problem 20% were more frequent (Table 3).
About 98.3% reported their happiness on services of the antenatal clinic; however 66.7% stated lack of enough information regarding possible outcomes of pregnancy and expected labor. Moreover, 97% complained their ANC visit did not help for psychosocial problems.
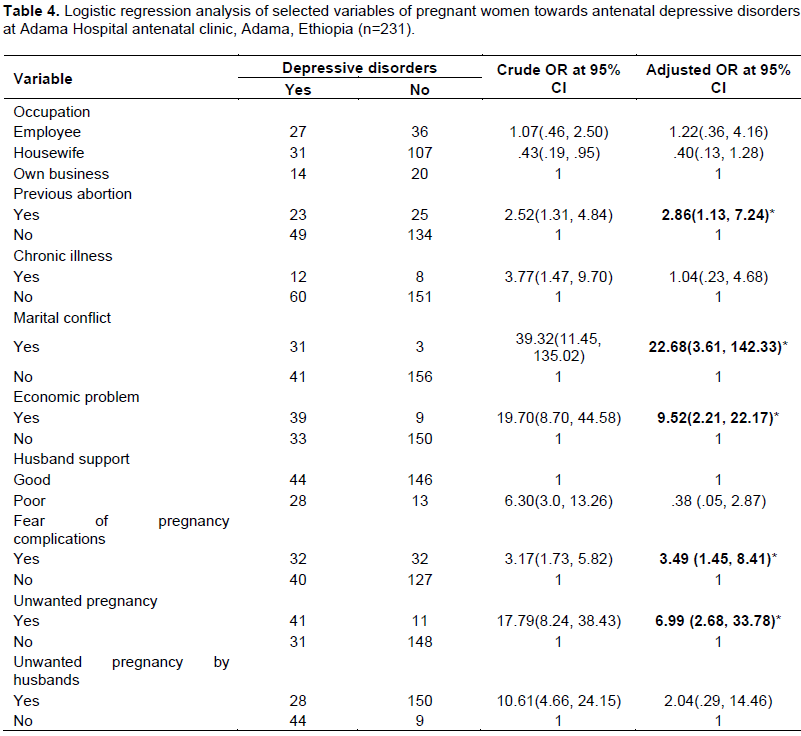
Association of covariates with antenatal depressive disorders
From logistic regression, there was statistically significant association between antenatal depressive disorder and previous abortion history [AOR=2.86, 95%CI=(1.13, 7.24)], unwanted pregnancy [AOR=6.99, 95%CI=(2.68, 33.78)], marital conflict (AOR=22.68 CI (3.61, 142.33)], economic problem [AOR=9.52, 95%CI=(2.21, 22.17)] and fear of pregnancy complications [AOR=3.49,95%CI=(1.45, 8.41)]. However, there was no statistically significant association between socio demographic variables and antenatal depressive disorder (Table 4).
This hospital based study attempted to assess the magnitude of antenatal depressive disorders and associated factors among Adama hospital antenatal clinic attendants. The screening material for prevalence rate was the standard BDI. Beck depression inventory was considered because it is revised recently in considering the DSM IV TR which is currently in use for psychiatric evaluation. Moreover, psychosocial factors, obstetric information, health and ANC related factors were recognized to assess associated factors.
Prevalence rate of antenatal depressive disorders in this study was 31.2%; within the range of previous reports at clinical settings. A report at Michigan Obstetric Clinics showed 20% and there was 33.1% prevalence rate at Ankara antenatal clinic (Mohammed and Gamble, 2011). Generally, considerable higher prevalence rates have been seen with screenings at health care facilities than community based studies. This could be due to effects of study designs, sample size, types of instrument and different cut-off points (Hart and Mahon, 2006; Stein et al., 1991).
Socio-demographic characteristics of participants were explained by age, educational status, income level, marital status and occupation. None of socio demographic features show association. This is analogous with a previous systemic review in Africa (Mohammed and Gamble, 2011).
There was discrepancy observed between influence of monthly income and economic problems on presence of antenatal depressive disorders. About 20.8% of subjects reported that economic problems were something that caused frequent stress. Similarly, pregnant women having economic problems were found to be 9.52 times prone to antenatal depressive disorders than financially stable ones. Conversely, monthly income was not found as an association. This may attributed women having less economic power and an unbalanced share on the financial management of family income. Furthermore, more than half of the participants were housewives who reported monthly income of their husbands.
Presence of bad obstetric history (complications of pregnancy and/or labour), number of live children, parity and age of pregnancy were not found in association with presence of antenatal depressive disorders. This was supported by a systemic review done in Africa (Mohammed and Gamble, 2011). But, opposite to previous report from rural Malawi (Rubertsson et al., 2005). Unwanted pregnancy indicated 6.99 times increased risk [AOR= 6.99 CI (2.21, 22.17)]; similar to a study in Brazil (Pereira et al., 2005). However; it was in contrast to findings at Cape Town (Kaaya et al., 2010). This could be due to the difference in sample size, inclusion exclusion criteria and used instruments. Fear of pregnancy complications [AOR=3.49, CI (1.45, 8.41)] and previous abortion [AOR=2.86, CI (1.13, 7.24)] showed strong association; analogous with a prior report in Africa (Lee et al., 2007).
A positive relationship between presence of chronic illness and antenatal depressive disorders was seen prior to controlling confounders but no longer existed; opposite to previous findings (Senturk et al., 2011). This might be explained by the variation in sample size and instruments. About 98.7% participants were happy on ANC service. Contrary to this, 68.8% of the study subjects and 97.2% of those having depressive disorders witnessed no enough information was provided at ANC about possible outcomes and expected delivery of the current pregnancy. This was found in line with the positive relationship between fear of pregnancy complications and antenatal depressive disorders [AOR=3.17, CI (1.45, 8.41)]. Moreover; 97% affirmed no benefit of ANC visits for their psychosocial problems. These all showed discrepancy to service satisfaction obtained from participants suggesting that perhaps participants did not feel comfortable reporting dissatisfaction because the survey took place at the hospital.
Marital conflict was associated to antenatal depressive disorders [AOR=22.68, CI (3.61, 142.33)] and this was similar to other studies (Pereira et al., 2009; Hartley et al., 2011). Opposite to societal values about pregnancy as joyful period for women, about 45% of study subjects declared pregnancy did not brought extra joy. This was also in line with other studies (Bennettt et al., 2004).
As limitation of this, it prone to demerits of the study design nature being cross sectional. The other limitation could be information bias may be introduced while using the measurement of BDI.
The prevalence of antenatal depressive disorder was high among Adama Hospital antenatal clinic attendants. It could be because this study is inclusive to all types of depressive disorders likely to occur at antenatal period. The effects of previous abortion, fear of pregnancy complications, economic problems, unwanted pregnancy and marital conflict have significant association with the development of antenatal depressive disorders. There should be consideration of integration of mental health service to antenatal clinic services by the hospital. Moreover; refreshment of the Hospital health professionals on antenatal depressive disorders, including common mental disorders within the contents of health education and early screening of pregnant women may help more.
The authors have not declared any conflict of interests.
REFERENCES
|
Adewuya AO, Ola BA, Aloba OO, Dada AO, Fasoto OO (2007). Prevalence and correlates of depression in late pregnancy among Nigerian women. Depress. Anxiety 24(1):15-21.
Crossref
|
|
|
|
Bennett HA, Einorson A, Taddio A (2004). Prevalence of depression during pregnancy: systemic review. Obstet. Gynecol. 103(4):698-709.
Crossref
|
|
|
|
|
Das V (1994). Moral orientations to suffering: Legitimation, power and healing. In: health and social change in international perspective; Chen L, Kleinman A and Ware N (eds,). pp. 139-170.
|
|
|
|
|
Dayan J, Creveuil C, Dreyfus M, Herlicoviez M, Baleyte JM, O'Keane V (2010). Developmental Model of Depression Applied to Prenatal Depression: Role of Present and Past Life Events, Past Emotional Disorders and Pregnancy Stress. PLoS One 5(9):e12942.
Crossref
|
|
|
|
|
Deyessa N, Berhane Y, Emmelin M, Ellsberg MC, Kullgren G, Högberg U (2010). Joint effect of maternal depression and intimate partner violence on increased child death in rural Ethiopia. Arch. Dis. Child 95(10):771-775.
Crossref
|
|
|
|
|
Felice E, Saliba J, Grech V, Cox J (2008). Prevalence rates and psychosocial characteristics associated with depression in pregnancy and postpartum in Maltese women. J. Affect. Disord. 82(2):297-301.
Crossref
|
|
|
|
|
Hart R, McMahon CA (2006). Mood state and psychological adjustment to pregnancy. Arch. Womens Ment. Health 9(6):329-337.
Crossref
|
|
|
|
|
Hartley M, Tomlinson M, Greco E, Comulada WS, Stewart J, Le Roux I, Mbewu N, Rotheram-Borus MJ (2011). Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reprod. Health 8(1):9.
Crossref
|
|
|
|
|
Kaaya SF, Mbwambo JK, Kilonzo GP, Van Den Borne H, Leshabari MT, Fawzi MC, Schaalma H (2010). Socio-economic and partner relationship factors associated with antenatal depressive morbidity among pregnant women in Dares Salaam, Tanzania. Tanzan. J. Health Res. 12(1):23-35.
Crossref
|
|
|
|
|
Lee AM, Lam SK, Lau SM, Chong CS, Chui HW, Fong DY (2007). Prevalence, course, risk factors for antenatal anxiety and depression. J. Obstet. Gynaecol. 110:1102-1112.
Crossref
|
|
|
|
|
Marcus SM, Flynn HA, Blow FC, Barry KL (2003). Depressive symptoms among pregnant women screened in obstetrics settings. J. Women's Health 12(4):373-380.
Crossref
|
|
|
|
|
Menon JA, Musonda VCT, Glazebrook C (2010). Perception of care in Zambian women attending community antenatal clinics. Educ. Res. 1(9):356-362.
|
|
|
|
|
Mohammad KI, Gamble J, Creedy DK (2011). Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery 27(6):e238-45.
Crossref
|
|
|
|
|
Nasreen HE, Kabir ZN, Forsell Y, Edhborg M (2010). Low birth weight in offspring of women with depressive and anxiety symptoms during pregnancy: results from a population based study in Bangladesh. BMC Public Health 10(1):515.
Crossref
|
|
|
|
|
Nasreen HE, Kabir ZN, Forsell Y, Edhborg M (2011). Prevalence and associated factors of depressive and anxiety symptoms during pregnancy: A population based study in rural Bangladesh. BMC Womens Health 11:22.
Crossref
|
|
|
|
|
Pereira PK, Lovisi GM, Pilowsky DL, Lima LA, Legay LF (2005). Depression during pregnancy: prevalence and risk factors among women attending a public health clinic in Rio de Janeiro, Brazil. Cad Saude Pub. 25(12):2725-2736.
|
|
|
|
|
Rubertsson C, Wickberg B, Gustavsson P, Rådestad I (2005). Depressive symptoms in early pregnancy, two months and one year postpartum-prevalence and psychosocial risk factors in a national Swedish sample. Arch. Womens Ment. Health 8(2):97-104.
Crossref
|
|
|
|
|
Sawyer A, Ayers S, Smith H (2010). Pre and post natal psychological well-being in Africa: A systemic review. J. Affect. Disord. 123(1-3):17-29.
Crossref
|
|
|
|
|
Senturk V, Abas M, Berksun O, Stewart R (2011). Social support and antenatal depression in extended and nuclear family environments in Turkey: a cross-sectional survey. BMC Psychiatry 11(1):48.
Crossref
|
|
|
|
|
Stein M, Miller AH, Trestman RL (1991). Depression, the immune system, and health and illness: findings in search of meaning. Arch. Gen. Psychiatry 48(2):171-177.
Crossref
|
|
|
|
|
Stewart RC, Bunn J, Vokhiwa M, Umar E, Kauye F, Fitzgerald M, Tomenson B, Rahman A, Creed F (2010). Common mental disorders and associated factors among women with young infants in rural Malawi. Soc Psychiatry Psychiatr. Epidemiol. 45(5):551-559.
Crossref
|
|