ABSTRACT
Midwives provide most of the maternity services, including nutritional counseling and education services. In Ghana, there is scarce evidence regarding the competency of midwives in providing sound nutritional advice to pregnant women. Therefore, the aim of this research was to assess the nutritional knowledge levels of final year midwifery students. A descriptive cross-sectional study was conducted, in which 562 final year midwifery students from six Midwifery Training Institutions answered 20 multiple-choice questions on nutritional-related issues during pregnancy. An average score of 9.8 (approximately 49%) was obtained by the respondents. Most (>70%) of the respondents were knowledgeable of the ideal time to start taking folic acid when planning to be pregnant and the effects of high alcohol intake during pregnancy. Key areas that require attention included recommended weight gain during pregnancy, sources and functions of micronutrients, such as folic acid, iron, vitamin C, calcium and iodine during pregnancy, and nutritional management of pregnancy-related conditions like pregnancy-induced hypertension, nausea and heartburn. The findings of this study support other reports that midwives need more training in human nutrition; and it has important implications for professional planning of curricula for midwifery education.
Key words: Midwifery students, nutrition education, diet during pregnancy.
Healthy eating is very critical before, during and after pregnancy. The nutritional status of a woman during the child-bearing stages of life has significant long-term consequences on the health and well-being of the mother, the growing foetus and newborn child (Marangoni et al., 2016; Darnton-Hill and Mkparu, 2015). It is therefore important that reliable nutrition information is given to pregnant women, and that midwives, the major health service providers of maternity care, have the requisite knowledge to execute their roles as nutrition counselors and educators (Elias and Green, 2007). Indeed, studies have established that nutrition education during pregnancy is associated with positive pregnancy outcomes (Streuling et al., 2010). Specifically in Ghana, previous studies have also highlighted the importance of nutritional counseling by health workers (Yawson et al., 2017; SPING/Ghana, 2013).
A systematic review to assess whether health professionals had the capacity to provide nutritional advice during pregnancy and if pregnant women were receiving such nutritional counselling services revealed that, generally, women in their reproductive age were not receiving adequate nutrition education during pregnancy. Although healthcare practitioners perceived nutrition education to be important, barriers to providing education to clients included lack of time, lack of resources and lack of relevant training (Lucas et al., 2014).
However, a literature review to explore the extent to which the role of midwives in nutrition education during pregnancy has been reported led to a conclusion that there is limited research available on the role of midwives in nutrition education during pregnancy. The authors therefore recommended that more research is required to explore the educational needs of midwives to enhance nutritional care of pregnant women (Arrish et al., 2014).
It has been asserted that midwives often lack the essential knowledge and skills to provide adequate and reliable nutrition advice to pregnant and lactating women on how to meet increased nutrient requirements during these critical and nutrient-demanding stages of their lives (Morton et al., 2014). Improving the quality of nutrition training of midwifery trainees is vital for building the necessary human resource capacity to provide effective nutrition education and counselling services in order to tackle the public health issue of malnutrition among vulnerable groups in Ghana (Yawson et al, 2017; Sodjinou et al., 2014).
In a review paper, Arrish et al. (2014) asserted that few studies have explored the nutrition knowledge of midwives. This study was therefore undertaken to assess the current status of nutritional knowledge of final year midwifery students who were in their last semester of training in six diploma awarding midwifery training tertiary institutions in Ghana.
This was a descriptive cross-sectional study designed to assess the nutritional knowledge of midwifery students at six diploma awarding midwifery training institutions in Ghana. The study was carried out to identify ‘gaps’ in the nutritional knowledge of these midwifery trainees who were in the last semester of their 3-year training programme.
Study participants
The inclusion criterion for participation was for a study participant to be in the final year of the three- year training programme. Hence only third (3rd) year midwifery students qualified to participate in the study since they had completed more than 75% of their course load required for their training and were more likely to have completed nutrition-related courses in the curriculum. Students in the first (1st) and second (2nd) years were excluded because they had not completed at least 75% of their course work.
Regarding sampling of the respondents after obtaining permission from the principals in the school, all final year students were approached and those who gave their consent to participate in the study signed an informed consent form and were given the questionnaire to complete. Therefore, participation was voluntary. Out of a total number of 571 questionnaires that were administered to students who consented to participate in the study in the six selected Midwifery training schools, 562 completed the questionnaire representing approximately 98.4% of the population. Participants were individually approached to seek for their consent to voluntarily participate in the study. The consenting process entailed thoroughly explaining the purpose of the study, confidentiality and the freedom to opt out of the study without any penalty. After the study had been thoroughly explained to the participants, they were only recruited to participate in the study after they gave their consent by signing an informed consent form. Confidentiality was maintained and anonymity of responses was ensured by avoiding the use of any form of identity of participants.
Data collection
The data was collected between November and December, 2016. A self-administered questionnaire was distributed to students who voluntarily gave their consent to participate in the study after the purpose for the study had been explained to them. The questionnaire used in this study is a modified version of nutritional knowledge questionnaires employed in similar studies among midwives in Australia (Arrish et al., 2016), New Zealand (Elias and Green, 2007) and Sudan (Elkhalifa and Kuppuswamy, 2014).
Information sought from the study participants included demographic data, educational background, knowledge about nutrition during pregnancy and respondents’ views regarding the relevance of nutrition as part of their school’s curriculum and their ability to thus apply nutritional knowledge in their career as professional midwives.
Quality assurance
Standard procedures were used to ensure accurate and consistent collection of data in each of the six schools. The data was collected by final year health science education university students who were undergoing their teaching practice in these six schools. They were trained on how to explain the purpose of the study to the students and issues on voluntary participation, informed consent, ensuring anonymity and confidentiality of responses given by the study participants.
The questionnaire was also pre-tested among 30 final year students to assess for reliability, clarity and simplicity of the test items at one midwifery training institution not selected for the final study. To ensure that responses given by the students were a true reflection of their knowledge levels, the students were not allowed to send the questionnaire out of their lecture rooms, but had to sit and answer the questions on their own without consulting any textbook or fellow student. Therefore it was ensured that students completed the questionnaire independently in a quiet lecture room setting.
Data analysis
The data was analysed using the Statistical Package for the Social Sciences (SPSS) programme, (version 21.0). Each correct multiple choice question was assigned a score of 1 mark (with a maximum possible score of 20 marks). In addition, the proportion of students who provided correct answers to each question was assessed and presented in tables. Descriptive statistics were run to summarize the data collected; and the results were displayed in frequencies, percentages and means.
All the study participants were females as the profession of midwifery is dominated by females with so few men in this profession. Most of the respondents, 514 (91.5%), were between the ages of 18 and 24 years.
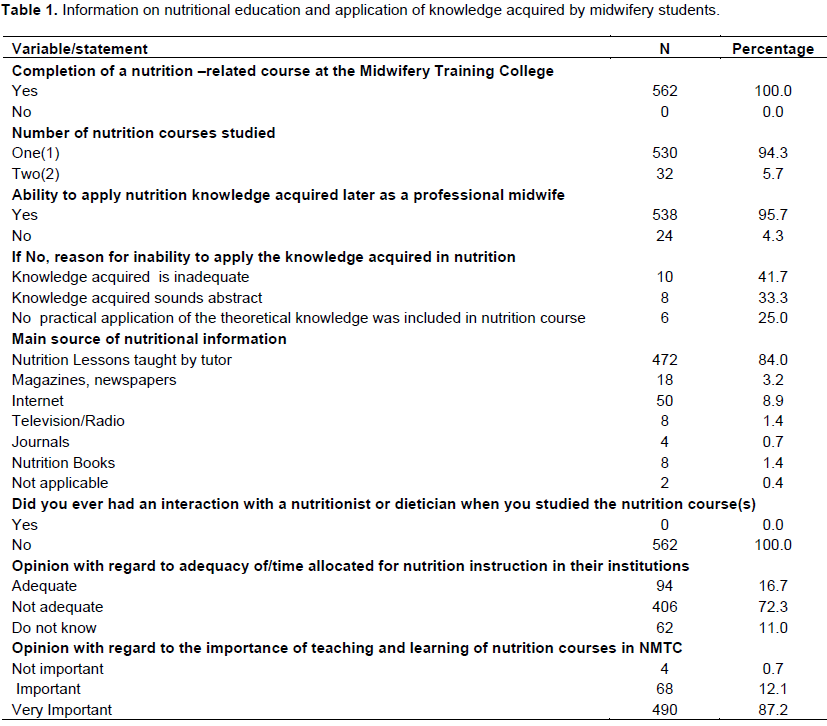
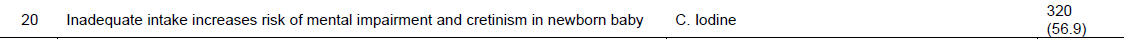
Nutrition education and application of knowledge acquired by study participants
Information on nutrition education and application of knowledge acquired by the surveyed midwifery students
are presented in Table 1.
The study revealed that all the study participants, 562 (100.0%) had completed and passed a nutrition course as required in their training. Majority 530 (94.3%) indicated that they had studied one nutrition course. A higher proportion of the respondents, 538 (95.7%), indicated that they had the ability to apply the nutrition knowledge acquired during their training later when they start working as professional midwives. Out of the 24, who indicated that they did not have the ability to apply the knowledge acquired later as professional midwives, most of them 10 (41.7%) pointed out that the knowledge acquired was not adequate, 8 (33.3%) indicated that the knowledge acquired sounds abstract, whereas for 6 (25%), they were not in a better position to apply the knowledge acquired in nutrition because no practical application of the theoretical knowledge was included in nutrition course. Most of the respondents (84.0%) indicated that their main source of nutritional information was from their nutrition course tutor rather than nutrition books or the internet. With regard to their opinion on the relevance of studying nutrition as part of their midwifery curriculum, majority 486 (86.5%) indicated that it is very important to study nutrition as midwifery students.
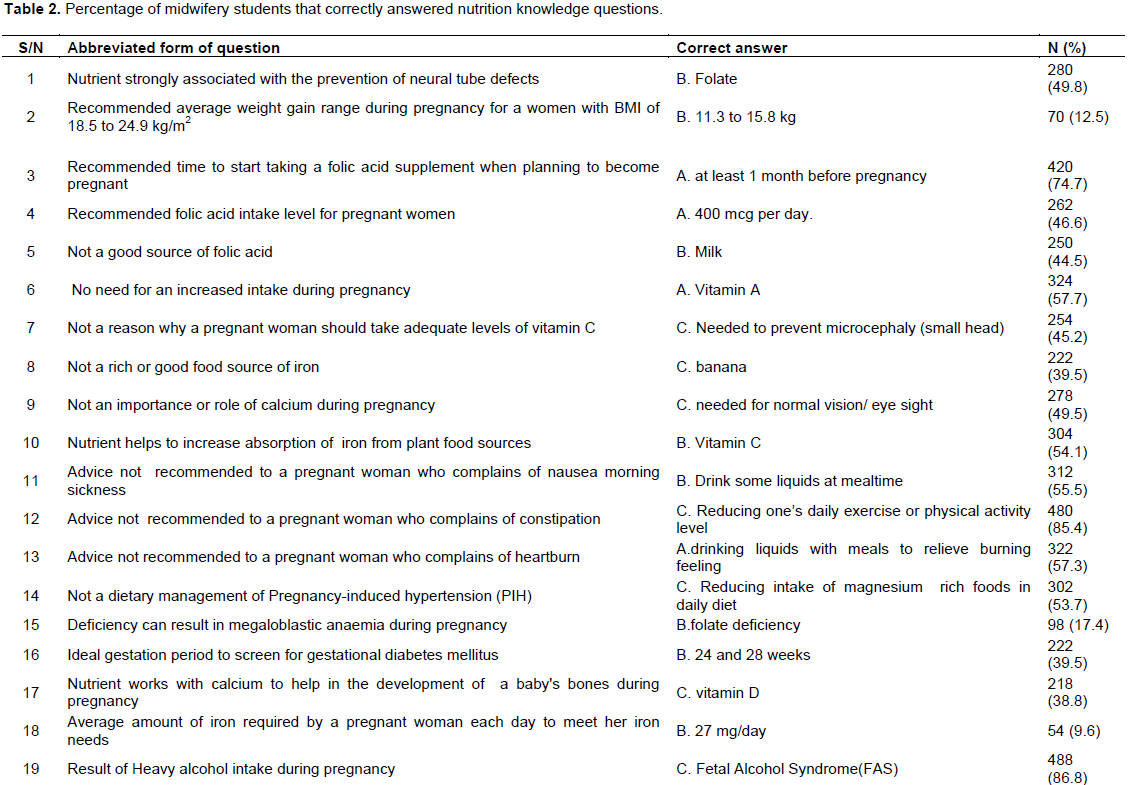
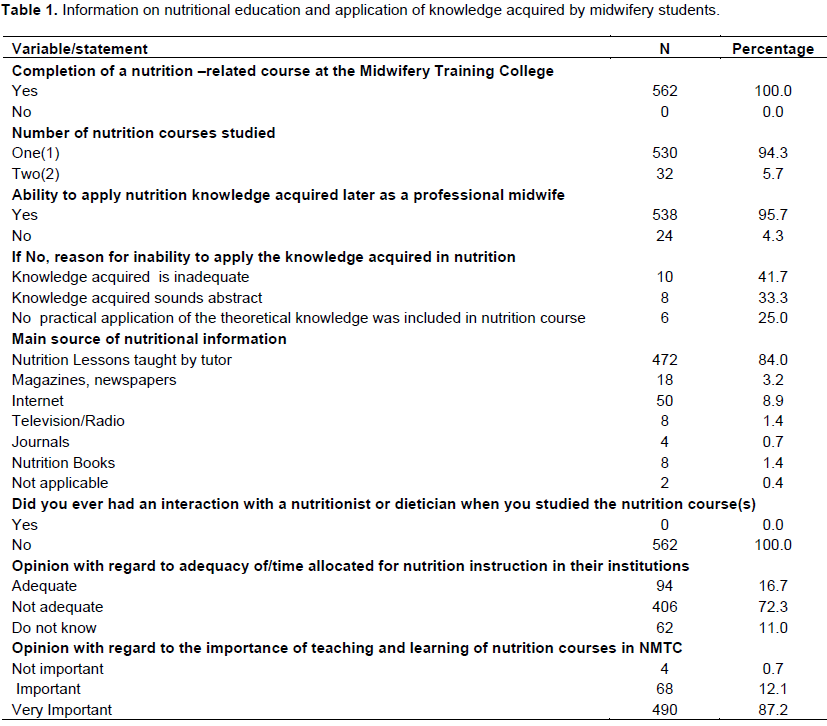
The percentage distribution of students who gave correct answers to the nutrition knowledge questions is presented in Table 2. The mean score for correctly answered questions for all the study participants was 9.8 (49%) out of the total 20 questions (approximately 49%). Some of these questions assessed respondents’ knowledge of the importance of taking folic acid supplements during pregnancy, recommendations on weight gain during pregnancy, importance of micronutrients such as vitamin C, B, calcium, iron, iodine, dietary management of pregnancy-related minor disorders and complications such as heartburn, constipation, pregnancy induced hypertension and effect of alcohol intake during pregnancy.
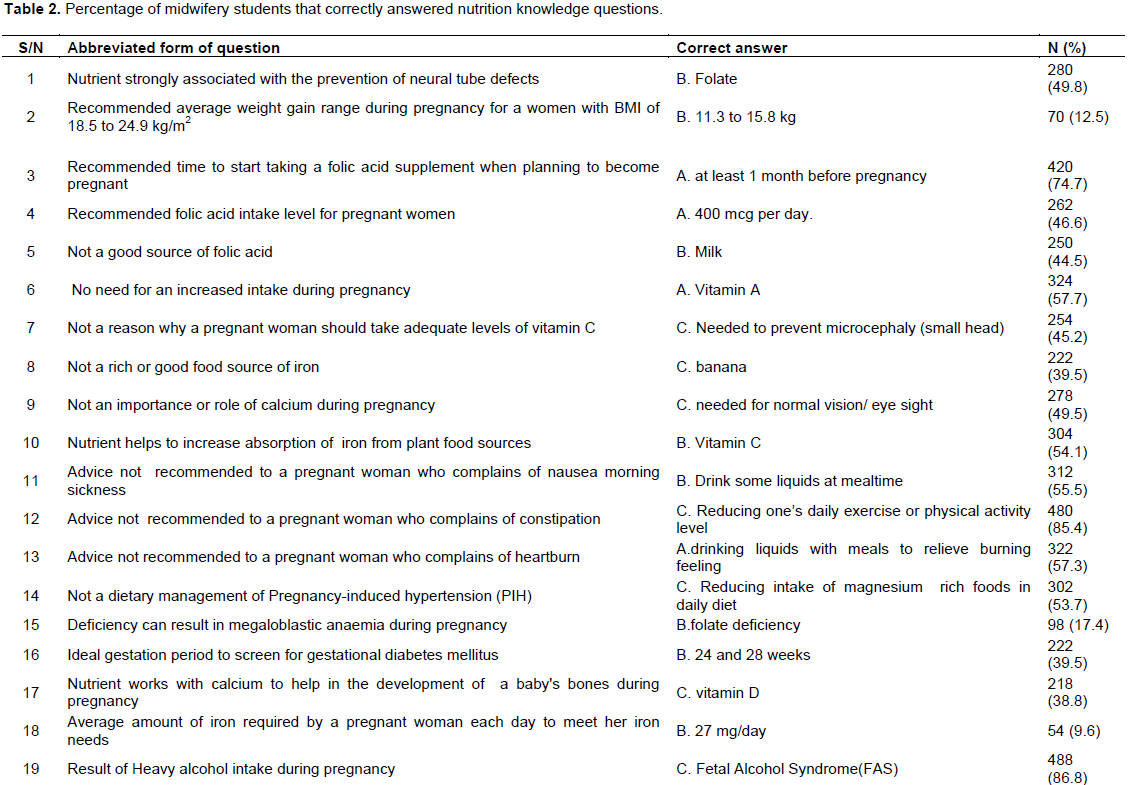
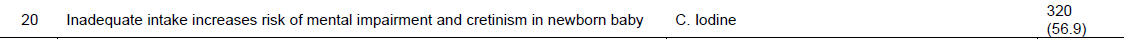
Three questions were answered correctly by less than 20% of the respondents. One of questions assessed respondents’ knowledge of the recommended average weight gain during pregnancy for women with normal/healthy BMI of 18.5 to 24.9 kg/m2 of which only 70 (12.5%) had it correct. The other question tested respondents’ knowledge of the nutrient whose deficiency can result in megaloblastic anaemia during pregnancy, of which only 98 (17.4%) were able to provide the right answer. Again, the third question which evaluated respondents’ knowledge on the approximate average iron intake per day during pregnancy was answered correctly by 9.6% of the respondents. Three questions were answered correctly by more than 30% but less than 40% of the respondents. One of the questions required that respondents should identify one out of five food sources given which was not a rich or good food source of iron, of which 222 (39.5%) provided the right answer. The other question assessed respondents’ knowledge on the gestation period in weeks which is ideal to screen pregnant women for gestational diabetes, of which 222 (39.5%) provided the correct answer. The third questionnaire assessed respondents’ knowledge on the nutrient that works with calcium to help in the development of a baby's bones during pregnancy, of which 38.8% had it correct.
Five questions were answered correctly by more than 40%, but less than 50% of the respondents. These five (5) questions assessed respondents’ knowledge on the nutrient associated with the prevention of neural tube defects, the recommended folic acid intake level for pregnant women, food sources of folic acid, reasons why a pregnant woman should take adequate levels of vitamin C and the importance of calcium during pregnancy. Six (6) questions were answered correctly by more than 50% but less than 60% of the respondents. Some of these six (6) questions assessed respondents’ knowledge on the nutrient that helps to increase absorption of iron from plant sources, nutritional advices that must be given to manage pregnancy induced hypertension (PIH), nausea, morning sickness and heartburns. Two (2) questions were answered correctly by more than 80% of the respondents. One of these questions sought to evaluate the knowledge levels of respondents on the dietary advice that must be given to pregnant women who complains of constipation. The other question sought to assess respondents’ knowledge on the result of heavy alcohol intake during pregnancy, of which 488 (86.8%) of the respondents provided the correct answer.
The results of the present study indicated that the mean score for correctly answered questions for all the study participants was approximately 49%, suggesting that the nutritional knowledge of midwifery students was poor as has been reported in similar studies previously conducted among midwives in Sudan (Elkhalifa and Kuppuswamy, 2014); Australia (Schmied et al., 2011) and the United Kingdom (Lee et al., 2010). The poor performance of the final year students in general in the present study can perhaps be attributed to the little emphasis or priority given to nutrition education during the training of midwives (Arish et al., 2016; Sodjinou et al., 2014). Other factors include the level of nutritional competences exhibited by tutors (Sethuraman et al., 2015) and issues related to the lack of essential aspects of human nutrition in courses taught (Shrimpton et al., 2016). In this study, majority (94.3%) of the final year students indicated that they studied only one nutrition course throughout the entire three year duration of the training programme.
Out of the 20 questions that were asked on maternal nutritional issues during pregnancy, 11 questions were answered correctly by less than 50% of the respondents. With regard to folic acid intake during pregnancy, only 46.6% knew the recommended folic acid intake level for pregnant women. It has been reported based on studies conducted in developing countries that majority of health professionals have insufficient knowledge on benefits, correct dose, particular time when folic acid should be administered to prevent Neural Tube Defects (NTDs) (Abedi et al., 2011) and food sources of folic acid (Demilew and Nigussie, 2017).
With respect to the importance of vitamin C during pregnancy, only 45.2% of the respondents knew the benefits of meeting the recommended intakes of vitamin C during pregnancy. The study also shows that 54.1% knew that vitamin C helps to increase absorption of iron from plant food sources. The fact that only 45.2% of the respondents knew the importance of vitamin C during pregnancy in a country like Ghana where about 42% of Ghanaian women aged between 15 and 49 are anaemic and 66% of children aged between 6 and 59 months are anaemic (Ghana Statistical Service (GSS), Ghana Health Service (GHS), 2015) warrants much attention. This is because of the important role that vitamin C plays in facilitating the absorption of non-heam iron.
With regard to calcium intake during pregnancy, only 49.5% knew about its role during pregnancy. In addition only 38.8% of the respondents knew the nutrient (vitamin D) which works with calcium to help in the development of a baby's bones during pregnancy. Regarding, the importance of iodine during pregnancy, a little over half (56.9%) of the participants knew that inadequate intake of iodine increases risk of mental impairment and cretinism in a newborn baby. Pregnant women have much higher iodine requirements as compared to all other population groups. The fact that midwives lack adequate knowledge about the importance of iodine during pregnancy has implications on the awareness of pregnant women and even their dietary intakes of good iodine food sources.
On the issue of gestational weight gain (GWG), only 12.5% knew the recommended average weight gain during pregnancy for women with healthy BMI of 18.5 to 24.9 kg/m2. Generally, it has been reported in some studies that generally, midwives give low priority to GWG, lack adequate knowledge in GWG and its management and in most cases fail to educate clients on weight gain management issues (Fieldwick et al., 2014; Willcox et al., 2012).
With respect to knowledge on gestational diabetes mellitus (GDM), only 39.5% knew that pregnant women should be screened for the condition between 24 and 28 weeks of pregnancy. The findings of this study suggest that midwifery trainees might not have been introduced to the need for screening pregnant women to early detect cases of women affected with gestational diabetes. Similarly, it has been reported that midwives knowledge about screening, management practices especially with diet and sensitization of women about gestational diabetes is low (Utz et al., 2016; Antos et al., 2013).
With regard to Pregnancy Induced Hypertension (PIH), only 53.7% could indicate out of five options given that reducing intake of magnesium rich foods is not a recommended dietary management of PIH. Generally, it has been indicated based on the findings of studies that the knowledge of midwives is deficient regarding management of PIH (Stellenberg and Ngwekazi, 2016; Munirathnamma and Lakshmamma, 2013). Munirathnamma and Lakshmamma (2013) reported that generally midwives are more knowledgeable in the area of nursing management than in the area of dietary management of PIH.
Findings from this study also revealed that majority (91.4%) of the final year midwifery trainees did not know the approximate average iron intake per day during pregnancy. Again, only 39.5% could indicate out of five food sources given (Meat, Spinach, Fish, Banana and Eggs) that banana is not a good food source of iron. This finding supports reports made in a similar study where most of the midwives failed to recognize rich food sources of iron (Elkhalifa and Kuppuswamy, 2014). This finding is worrying and warrants great attention particularly considering WHO reports that more than 40% of pregnant women worldwide are anaemic and that at least half of this anaemia burden is assumed to be due to iron deficiency (WHO, 2017).
Findings from this study demonstrate and reiterate the need for continued education to improve midwifery trainees’ nutrition knowledge which will boost their confidence as they carry out their duties. Recommendations include the need to update and strengthen the content of the nutrition curriculum in collaboration with experts in nutrition such as dieticians and public health nutritionists. In addition, developing a maternal nutrition resource toolkit which can be approved and adopted for use by all midwifery training institutions and conducting regular refresher workshops for midwifery tutors who teach nutrition-related courses are also worth considering. It is also worthwhile considering giving midwifery students the opportunity to apply their theoretical knowledge on the field while being mentored by a dietician or a public health nutritionist as part of the curriculum for their training.
Generally, majority of midwifery students who are in their final semester of their three-year training lacked basic knowledge of nutrition requirements during pregnancy. Their poor nutritional knowledge was evident in the fact that less than 50% of them could provide the right answers to most of the questions asked (11 out of 20 questions). Lack of knowledge in areas in maternal nutrition which were evident among the final-year midwifery diploma students include weight gain during pregnancy, role and food sources of critical micronutrients in pregnancy such as iron, folic acid, calcium, vitamin D and vitamin C. Other areas which were deficient in the knowledge levels of the study participants include screening for gestational diabetes, and dietary management of problems such as nausea, heartburn and pregnancy-induced hypertension (PIH) during pregnancy.
The authors have not declared any conflict of interests.
REFERENCES
|
Abedi G, Abdollahi F, Etemadinejad S (2011). Health behaviors of health practitioners about folic acid in Mazandaran province, Sari, Iran. World Appl. Sci. J. 12:944-50.
|
|
|
|
Antos E, Nowak B, Olszewski J (2013). The analysis of midwives' knowledge on the education of women with gestational diabetes and preparation for it. J. Public Health, Nurs. Med. Rescue 19(4):29-36.
|
|
|
|
|
Arrish J, Yeatman H, Williamson M (2014). Midwives and nutrition education during pregnancy: A literature review. Women Birth 27(1):2-8.
Crossref
|
|
|
|
|
Arrish J, Yeatman H, Williamson M (2016). Australian midwives and provision of nutrition education during pregnancy: A cross sectional survey of nutrition knowledge, attitudes, and confidence. Women Birth 29(5):455-464.
Crossref
|
|
|
|
|
Darnton-Hill I, Mkparu UC (2015). Micronutrients in pregnancy in low-and middle-income countries. Nutrients 7(3):1744-1768.
Crossref
|
|
|
|
|
Demilew YM, Nigussie AA (2017). Knowledge of Health Professionals on Folic Acid Use and Their Prescribing Practice in Bahir Dar City Administration, Northwest Ethiopia: Cross-Sectional Study. PloS One 12(1):e0170116.
Crossref
|
|
|
|
|
Elias S, Green T (2007). Nutrition knowledge and attitudes of New Zealand registered midwives. Nutr. Diet. 64(4):290-294.
Crossref
|
|
|
|
|
Elkhalifa AEO, Kuppuswamy SB (2014). Evaluation of Midwifery Knowledge on Antenatal Care in Omdurman Maternity Hospital Sudan. Int. J. Health Sci. Educ. 2(2):127-142.
|
|
|
|
|
Fieldwick D, Paterson H, Stephen M, Cameron A, Egan R, McFadden S, Pienaar J, Sinclair C, Struthers T, Taplin K, Watson C (2014). Management of excess weight in pregnancy in Otago, New Zealand: a qualitative study with lead maternity carers. NZ Med. J. 127(1392):27-37.
|
|
|
|
|
Ghana Statistical Service (GSS) (2014). Ghana Health Service (GHS), ICF International (2015). Ghana Demographic and Health Survey 2014. Rockville, Maryland, USA: GSS, GHS, and ICF International.
|
|
|
|
|
Lee D, Haynes C, Garrod D (2010). Exploring health promotion practice within maternity services. National Health Service Foundation Trust. Stockport, UK: National Health Service.
|
|
|
|
|
Lucas C, Charlton KE, Yeatman H (2014). Nutrition advice during pregnancy: do women receive it and can health professionals provide it? Matern Child Health J. 18(10):2465-2478.
Crossref
|
|
|
|
|
Marangoni F, Cetin I, Verduci E, Canzone G, Giovannini M, Scollo P, Corsello G, Poli A (2016). Maternal Diet and Nutrient Requirements in Pregnancy and Breastfeeding. An Italian Consensus Document. Nutrients 8(10):629.
Crossref
|
|
|
|
|
Morton SM, Grant CC, Wall CR, Carr PEA, Bandara DK, Schmidt JM, Ivory V, Inskip HM, Camargo CA (2014). Adherence to nutritional guidelines in pregnancy: evidence from the Growing Up in New Zealand birth cohort study. Public Health Nutr. 17(9):1919-1929.
Crossref
|
|
|
|
|
Munirathnamma M, Lakshmamma T (2013) Knowledge of Staff Nurses Regarding Management of Pregnancy Induced Hypertension (PIH). Int. J. Soc. Sci. Humanit. Invent. 2(11):8-12.
|
|
|
|
|
Schmied VA, Duff M, Dahlen HG, Mills AE, Kolt GS (2011). 'Not waving but drowning': a study of the experiences and concerns of midwives and other health professionals caring for obese childbearing women. Midwifery 27(4):424-430.
Crossref
|
|
|
|
|
Sethuraman K (2015). Development of a public health nutrition workforce: Nurses and midwives in Ghana. In 2015 APHA Annual Meeting and Expo (Oct. 31-Nov. 4, 2015). APHA.
|
|
|
|
|
Shrimpton R, du Plessis LM, Delisle H, Blaney S, Atwood SJ, Sanders D, Margetts B, Hughes R (2016). Public health nutrition capacity: assuring the quality of workforce preparation for scaling up nutrition programmes. Public Health Nutr. 19(11):2090-2100.
Crossref
|
|
|
|
|
Sodjinou R, Bosu WK, Fanou N, Déart L, Kupka R, Tchibindat F, Baker S (2014). Nutrition training in medical and other health professional schools in West Africa: the need to improve current approaches and enhance training effectiveness. Glob. Health Action 2014:7.
Crossref
|
|
|
|
|
Stellenberg EL, Ngwekazi NL (2016). Knowledge of midwives about hypertensive disorders during pregnancy in primary healthcare. Afr. J. Prim. Health Care Fam. Med. 8(1):1- 6.
Crossref
|
|
|
|
|
SPING/Ghana (Strengthening Partnerships, Results and Innovations in Nutrition Globally) (2013). Breastfeeding Basics Mean Better Nutrition: The Important Role of Nutrition Counseling in Ghana. United States Agency for International Development (USAID) and JSI Research and Training Institute, Inc.
|
|
|
|
|
Streuling I, Beyerlein A, von Kries R (2010). Can gestational weight gain be modified by increasing physical activity and diet counseling? A meta-analysis of interventional trials. Am. J. Clin. Nutr. 2010:29363.
hCrossref
|
|
|
|
|
Utz B, Assarag B, Essolbi A, Barkat A, Benkaddour YA, De Brouwere V (2016). Diagnosis a posteriori? Assessing gestational diabetes screening and management in Morocco. Glob. Health Action 2016:9.
Crossref
|
|
|
|
|
Willcox JC, Campbell KJ, van der Pligt P, Hoban E, Pidd D, Wilkinson S (2012). Excess gestational weight gain: an exploration of midwives' views and practice. BMC Pregnancy Childbirth 12(1):102.
Crossref
|
|
|
|
|
Yawson AE, Amoaful EO, Senaya LK, Yawson AO, Aboagye PK, Mahama AB, Selenje L, Ngongalah V (2017). The lancet series nutritional interventions in Ghana: a determinants analysis approach to inform nutrition strategic planning. BMC Nutr. 3(1):27.
Crossref
|
|