ABSTRACT
The word "prescription", from "pre-" ("before") and "script" ("writing, written"), refers to the fact that the prescription is an order that must be written down before a drug can be dispensed. Prescription is a written order by the prescriber to the dispenser on how the drug should be dispensed. It serves as a means of communication among the prescriber, dispenser and drug consumer pertaining to treatment. That is why doctors are legally obliged to write prescription clearly. However, most of the time prescriptions are found to be unclear. Accordingly, the main objective of this survey study was to investigate the factors that affect proper prescription writing in Jimma University specialized hospital. In order to achieve the main objective, four specific objectives related to knowledge and perception on importance of good prescription and consequences of sloppy prescription writing, the practice of good prescription writing and other factors that affect the proper prescription writing were formulated. One hundred (25%) of the physicians and 50(100%) of the pharmacists were included in the survey. In order to select sample physicians, convenience sampling technique was employed. In order to collect data from the sample, two instruments namely questionnaire and document analysis were used. The collected data were analyzed using percentage and mean value. The result of the survey showed that most of the physicians have knowledge on the importance of clear prescription writing and they positively perceived that sloppy prescription writing has negative impact on both pharmacists and patients. Nevertheless, the magnitude of writing clear prescription was low because 54.8% of the sample prescriptions were proved to be illegible. Moreover, 70% of the pharmacists also reported that physicians write clear prescription only some times. The major factors that affect the proper prescription writing, according to the physicians, are shortage of time (69%), difficulty of some medicine names to spell (80%) and lack of feedback from pharmacists (52%) on their (physicians’) unclear prescription writing. Therefore, the university in collaboration with the hospital administrative bodies, ministry of health and other concerned bodies should work to make the physicians responsible and work cooperatively with pharmacists to alleviate the problem because illegible prescription may pose a medical threat to the treatment of a patient.
Key words: Prescription, writing, medical threat, illegible handwriting.
The word "prescription", from "pre-" ("before") and "script" ("writing, written"), refers to the fact that the prescription is an order that must be written down before a drug can be dispensed (DACA of Ethiopia, 2011). Prescription is a
written order by the prescriber to the dispenser on how the drug should be dispensed. It serves as a means of communication among the prescriber, dispenser and drug consumer pertaining to treatment or prophylaxis (DACA of Ethiopia, 2010).
It is often claimed that prescription is only meant for peers, who are specialized in deciphering the scrabbling because they most probably produce similar notes. Another joke says that while doctors are trained to write unreadable notes, pharmacists are trained to decipher them (Majorie, 2012).
Unlike the claim, DACA of Ethiopia (2010) argues that though there is no global standard for prescriptions and every country has its own regulations, the most important requirement is that the prescription be clear, legible and indicate precisely what should be given. Precise, according to Neville and Martin (2006), does not always mean short, but it means accurately expressed. They suggest that something that is precise will be clear and unambiguous, which is what is needed in scientific or medical writing.
Poor handwriting is a well-known and preventable cause of dispensing errors. All physicians share in the responsibility for preventing adverse drug events by writing prescriptions clearly and questioning intent whenever an order is ambiguous (Murray et al., 2009). It is assumed that the doctor is always focusing on the diagnosis and medication more than on writing the prescription (Majorie, 2012). However, trying to save time by writing quickly is a false economy (National Handwriting Day, 23). Doctors are legally obliged to write prescription clearly. They are under a legal duty of care to write clearly, that is with sufficient legibility to prevent medication error (BMJ, 1999).
Some abbreviations that are ambiguous, or that in their written form might be confused with something else, are not recommended and should be avoided during prescription writing (WHO, 2008). This is because abbreviation of the word units to IU resulted in the administration of 10-fold overdoses of insulin when prescriptions for 6IU were misread as 61 units (Pharm, 2001; 267:193). Many serious dispensing errors can be traced to the use of abbreviations (Cohen, 2007). The abbreviation "U" or "I" must NOT be used when writing prescription, as it leads to errors such as misinterpretation of "U" as 0 or 4, or "IU" as 10 or 14. The word "unit" should be written as such. The use of a slash mark (/) to separate names and doses can result in the incorrect drug or dose being dispensed; the slash mark may be interpreted as a letter or number (Teichman and Caffee, 2002). Moreover, unnecessary use of decimal points in prescription writing results in ineffective communication that can cause medication error (WHO, 2008).
Prescribing is one aspect of patient care where it is possible to do considerable harm if not done judiciously (www.xenomed.com/forums/jnma). More problems are caused by medications than illness and implausibly, there is evidence that medication errors and adverse events are the primary cause of death in the United States today (National Handwriting Day, 23). According to report from the Institute of Medicine (IOM) (2006), doctors' sloppy handwriting kills more than 7,000 people annually in America. As indicated by Majorie (2012), many such errors result from unclear abbreviations and dosage indications and illegible writing on some of the 3.2 billion prescriptions written in the U.S. every year.
Moreover, illegible handwriting can delay treatment and lead to unnecessary tests and inappropriate doses which, in turn, can result in discomfort and death (National Handwriting Day, January 23). Administrators and health systems analysts should be aware of sloppy prescription writing which can lead to prolonged hospital stay and significant clinical deterioration (ibid).
Many pharmacists also complain about sloppy handwriting saying that it is more than an annoyance; it causes some very serious and costly problems in the real world (National handwriting day, January 23).
Abdella and Wabe (2012) conducted research on prescribers’ adherence to the basic principles of prescription order writing in Jimma health center. Their findings showed that prescribers had good adherence with some variables such as number of drugs per prescription, sex, age and generic name and poor adherence with some variables such as card number, prescribers’ name and signature and strength. However, this study is different in that it dealt with the factors that contribute to sloppy prescription writing.
The researcher, most of the time, tried to read the prescriptions written for him and for others in hospitals in different times and he found them unclear. Moreover, he, one day, heard the pharmacists complaining about sloppy prescription writing on one of the FM radio programs in his country. Thus, it is with this intention that he wanted to investigate the factors that impede proper prescription writing in Jimma University specialized hospital.
Institutional based cross- sectional study was carried out on factors that impede proper prescription writing in Jimma University specialized hospital in November 2014. The term proper in this survey refers to the word clear or legible. Thus, proper prescription writing refers to clear and understandable writing which also incorporates the physician’s name and phone number. The combination of qualitative and quantitative methods was employed for the survey.
Population and sample
Physicians and pharmacists of the hospital were the subjects of the study. As the information obtained from the hospital’s human resource shows, the total number of physicians and pharmacists in the hospital were 403 and 50 respectively. In order to get sample physicians, convenience sampling technique was used. Since the pharmacists were few (50) in number, they were all included in the study. Accordingly, 100 (25%) of the physicians and 50 (100%) of the pharmacists were included in the study.
Instruments and procedures
Both questionnaire and document analysis were used to collect data for the study. The researcher used more of closed-ended questions for both physicians and pharmacists. This is because, according to Kumar, 1996: 119, closed ended questions provide ‘ready made’ categories within which respondents reply to the questions asked by the researcher. All the questionnaires were pre tested and finally administered after they were passed through evaluation and criticism and proved to be valuable. All of the respondents answered the questions and returned the question papers.
In order to substantiate the data obtained through questionnaire, the researcher also used document analysis. As the information obtained from Jimma University model pharmacy shows, number one model pharmacy receives 500 prescriptions in average per day. The researcher randomly selected 500 prescriptions and analyzed them in terms of the check list he already prepared. The check list contains five (5) items. The five items were chosen because they are more related to the issue of proper prescription writing. Before using the check list for analysis, the researcher got it checked and proven by his colleagues.
Methods of data analysis
The data obtained through the instruments were analyzed using both qualitative and quantitative methods. Simple statistics such as percentage and mean values were used to report the results in numerical values whereas the qualitative data were described using descriptive method.
Hundred (100) sample physicians and all (50) pharmacists were included in the study. Totally 150 respondents were selected as a sample for the study. Sixty percent (60%) of the physicians are graduating physicians (internship) whereas 35% of them are qualified in first degree (MD) and the rest 5% are specialists. Eighty nine percent (89%) of the physicians are between the ages of 20-30 whereas the rest 11% are between the ages of 31-40. All of the graduating physicians (internship) (60%) have served as a physician for not more than one year and they write 10 to 25 prescriptions per day in average whereas the rest 40% of the physicians have served as a physician for more than two years (ranges from 2-6 years) and they write 30 to 55 prescriptions per day on average.
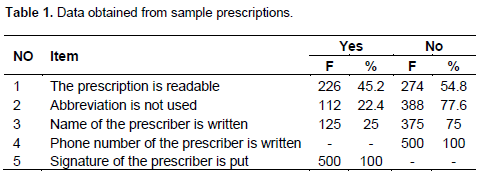
The table 1 above shows that 54.8% of the sample prescriptions are not readable. At the same time, 77.6% of the prescriptions are full of abbreviations. Although 100% of the physicians put their signature on the prescription they write, 75% of them do not write their name on the prescription and 100% of the physicians do not write phone number on the prescriptions they write.
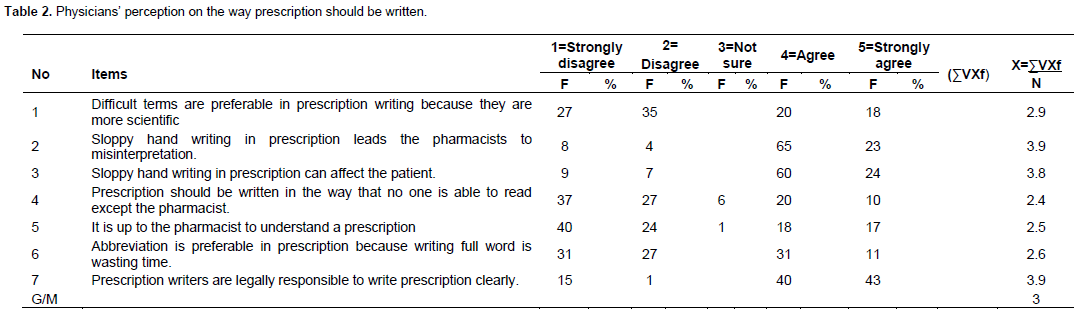
Majority of the physicians did not support the use of difficult terms in prescription writing by indicating their strongly disagreement (27%) and disagreement (35%) to the item that says difficult terms are preferable in prescription writing because they are more scientific. Moreover, all of the respondents (100%) showed that sloppy hand writing in prescription leads the pharmacists to misinterpretation and the result can affect the patient (Table 2).
More than half (64%) of the respondents supported that prescription should be legible to any literate person. The same number (64%) of the respondents (physicians) perceived that they cooperate with pharmacists when unclear prescription is received. Significant number of them (83%) also indicated that they are legally res-ponsible to write a prescription clearly.
Moreover, majority of the respondents did not support the use of abbreviation in prescription writing by indicating that they strongly disagree (31%) and disagree (27%) with the assumption that says abbreviation is preferable in prescription because writing full word is wasting time.
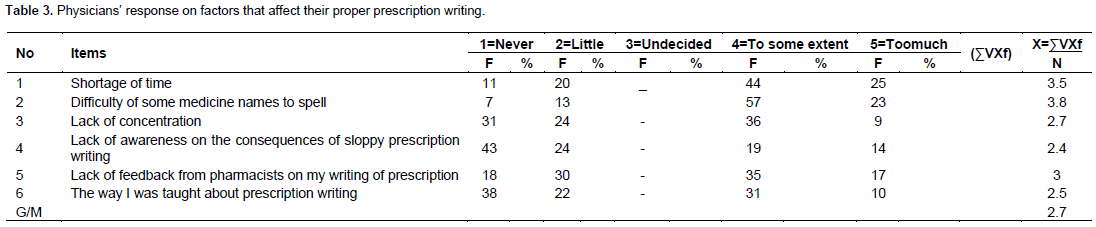
Writing clear and unambiguous prescription is very important and it is one aspect of patient care (www.xenomed.com/forums/jnma). Nevertheless, there are many constraints which may hinder the physicians to do so. Regarding this, 6 main common factors are selected and included for the physicians (Table 3). The responses of the physicians on these factors are analyzed and presented below.
Majority of the physicians (69%) responded that shortage of time affects their proper prescription writing. The mean value (3.5) also shows that shortage of time affects the physicians’ proper prescription writing. The other factor that affects the physicians’ proper prescription writing as indicated by many of th
em (80%) is difficulty of some medicine names to spell. Besides, more than half (52%) of the physicians indicated that they do not get feedback from pharmacists on the illegibility of the prescriptions they (physicians) write.
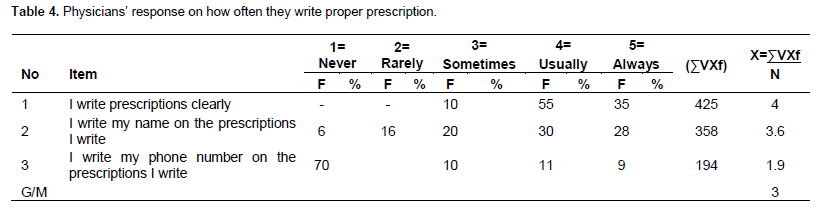
More than half of the physicians (55%) said that they usually write clear prescription whereas 35% of them said that they always write clear prescription. Regarding whether the physicians write their name on the prescription they write or not, the mean value (3.6) tends to show that they usually write their name. Nevertheless, more than half of the respondents (70%) indicated that they do not write their phone number on the prescription they write (table 4).
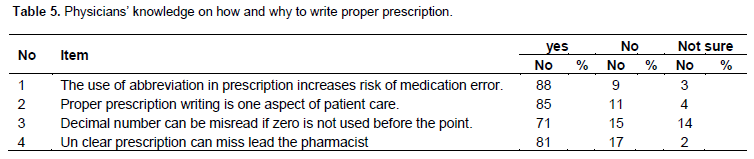
Significant number of the physicians (88%) responded that they know that the use of abbreviation in prescription increases risk of medication error. At the same time, 85% of them also said that they know that proper prescription writing is one aspect of patient care. Moreover, 81% of the physicians showed that they know the consequences of unclear prescription (Table 5).
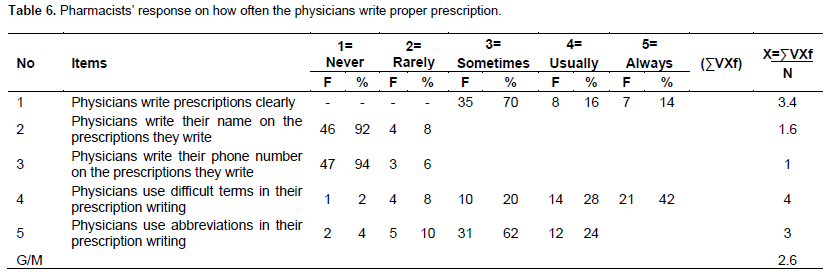
In order to substantiate the responses of the physicians on how often they write proper prescription, five (5) items are included in the pharmacists’ questionnaire (Table 6). Their responses are analyzed and presented below.
Significant number of the pharmacists (70%) responded that physicians write clear prescription only sometimes. The mean value (3.4) also indicates that they do it only sometimes. Moreover, 46% of the pharmacists responded that the physicians never write their name on the prescription they write whereas the rest 54% of them indicated that the physicians rarely write their name on the prescription. Almost all of the respondents (94%) answered that physicians do not also write phone number on the prescription they write. Regarding the use of difficult terms which can affect the readability of prescription, the mean value (4) indicates that the physicians usually use them in the prescriptions they write. More than half (62%) of the pharmacists also said that physicians sometimes use abbreviations when writing prescriptions whereas 24% of them indicated that physicians usually prefer abbreviation to writing full words when writing prescription.
In order to assess pharmacists’ perception on the impact of improper prescription, 3 items are included in their questionnaire (Table 7). Their responses are analyzed and presented below.
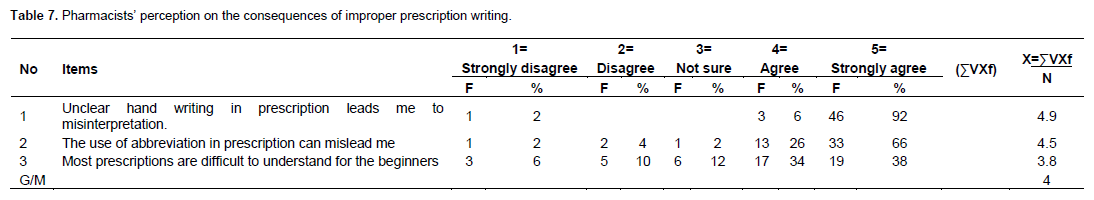
Majority of the pharmacists (92%) said that unclear hand writing in prescription can lead them to commit medication error by misinterpreting. The same number (92%) of them also indicated that the use of abbreviation in prescription can mislead them. Moreover, 72% of the respondents supported that most of the prescriptions they receive are difficult to understand for the beginners.
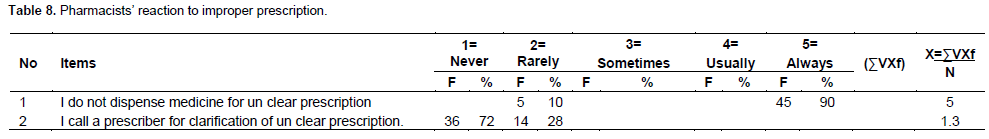
In order to know the pharmacists’ reaction against improper prescription, two (2) items are included in pharmacists’ questionnaires (Table 8). Thus, their responses on the items are analyzed and presented below.
Majority of the pharmacists (90%) said that they do not dispense medicine for unclear prescription. Besides, 72% of them also indicated that they never call a prescriber for clarification of unclear prescription whereas the rest 28% of them said that they rarely call the prescriber for clarification.
DISCUSSION OF THE RESULTS
This part deals with the discussions of the results of the study in response to the research objectives. Below are the research questions to be discussed:
1. Do physicians have necessary knowledge on the impact of sloppy prescription writing?
2. Do physicians positively perceive the fact that prescriptions should be written clearly?
3. To what extent do physicians practice their legal responsibility when writing a prescription?
4. What are the other factors that affect proper prescription writing?
Do physicians have necessary knowledge on the impact of sloppy prescription writing?
Being alert to common problems that can occur with medication orders can assist in reducing medication errors (Murray et al., 2009). Thus, in order to assess whether physicians have necessary knowledge on how to write proper prescription, 4 questions were included in physicians’ questionnaires. Accordingly, all of the physicians responded that they have necessary knowledge on how to write proper (clear) prescription. They also revealed that clear prescription writing is one aspect of patient care. Nevertheless, their knowledge on the importance of clear prescription writing did not help them to be pragmatic about it because more than half (54.8%) of the sample prescriptions were proved to be unclear. Moreover, 70% of the pharmacists witnessed that physicians write clear prescription only sometimes. This implies that they are not putting their knowledge in to practice.
Do physicians positively perceive the fact that prescriptions should be written clearly?
In order to find out physicians’ perception on the way how prescription should be written, 7 questions were prepared and included for the physicians. Accordingly, the analyses of physicians’ responses revealed that majority of the physicians seem to have positively perceived that prescription should be written clearly to avoid the negative consequences of illegible prescription. Nevertheless, their positive perception on the importance of clear prescription and the consequences of unclear prescription did not help most of them to write it clearly. This was witnessed by the result obtained from document analysis which revealed that 54.8% of the sample prescriptions were found to be unclear.
To what extent do physicians practice their legal responsibility when writing a prescription?
Even though there is no global standard for prescriptions and every country has its own regulations, the most important requirement is that the prescription be clear, legible and indicate precisely what should be given (DACA of Ethiopia, 2010). Precise, according to Neville and Martin (2006), does not always mean short, but it means accurately expressed. They suggest that something that is precise will be clear and unambiguous, which is what is needed in scientific or medical writing. Neville and Martin (2006) also emphasize that readers should be able to understand a sentence on first reading, each idea following logically from the previous one. Moreover, if physicians include their name, phone number, signature, date and etc. in the prescriptions they write, not much can go wrong because if the pharmacist has any questions about the prescription (s), he can easily contact the prescriber (WHO,1992). In line to this, 3 important questions were chosen and included in the physicians’ questionnaire to assess how often they write clear prescription and their name and phone number on it. The analysis of their responses is discussed below:
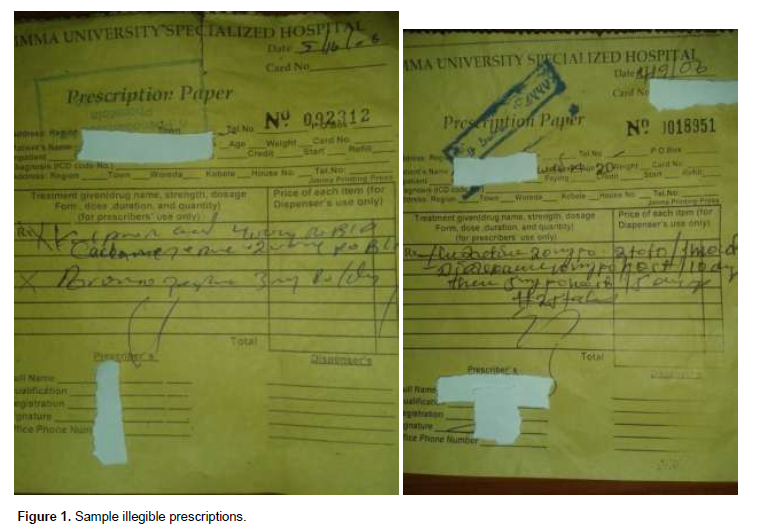
Majority of the physicians indicated that they usually write clear and legible prescriptions. The mean value (4) of their responses on this regard also showed that the physicians usually write clear prescription. Nevertheless, the result of document analysis (sample prescriptions) showed that 54.8% of the prescriptions were unreadable while some from the rest are only semi readable. Moreover, 70% of the pharmacists supported that physicians write clear prescription only sometimes. As a result, many of the pharmacists, when asked what they do when they receive unclear prescription, said that they do not dispense medicine for unclear prescription which results to delay of treatment as a result of which the patient can be victimized. The idea on National handwriting day (January 23) supports this result that illegible handwriting can delay treatment and lead to unnecessary tests and inappropriate doses which, in turn, can result in discomfort and death. This implies that what physicians said about the clarity of their prescriptions and what they did are not the same. The following sample prescriptions support the result (Figure 1).
Doctors are legally obliged to write prescription clearly. They are under a legal duty of care to write clearly, that is with sufficient legibility to prevent medication error (BMJ, 1999). Sloppy handwriting in prescription can be inter-preted by the jury as sloppy care (National Handwriting Day, January 23).
For the question that asks how often the physicians write their name on the prescription they write, majority of them said that they usually write their name on the prescriptions they write. The mean value (3.6) tends to show that they usually write their name on the prescription they write. However, the analysis of sample prescription result shows that few of the physicians (less than 25%) write their name when writing prescription. This shows that there is contradiction between what they say and what they practically do.
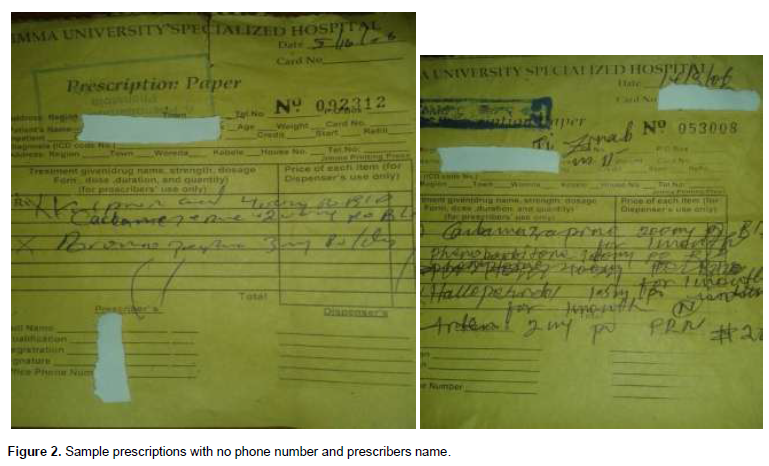
Prescriptions have legal implications, as they may indicate that the prescriber takes responsibility for the clinical care of the patient and in particular for monitoring efficacy and
safety (Wikipedia, the free encyclopedia). Writing phone number is one of the implications. More than half of the respondents (70%) indicated that they do not write their phone number on the prescriptions they write. The analysis of sample prescription result (100%) showed that none of the physicians write phone numbers on the prescription they write. This was also supported by significant number of the pharmacists (94%). This implies that they are disobeying the legal requirement about prescription writing to work collaboratively with pharma-cists to minimize medication error. The following sample prescriptions support the result (Figure 2).
This might be the reason for which majority of the pharmacists said that they do not call physicians for clarification of unclear prescription. So the only options that the pharmacists have are either to dispense medicine based on their experience or refrain from dispensing which either of them is not good.
What are the other factors that affect proper prescription writing?
Writing clear and unambiguous prescription is very important because it is one aspect of patient care (DACA of Ethiopia, 2010). Nevertheless, there are many constraints which may hinder the physicians to do so. Regarding this, 6 main common factors are selected and included for the physicians. Below are their discussions:
Majority (69%) of the physicians revealed that shortage of time affects their proper prescription writing. National handwriting day (January 23) argues that trying to save time by writing quickly in medical is thus a false economy. Moreover, 80% of the physicians indicated that they have spelling problem when writing some medicines name. The mean value (3.8) also showed they have spelling problem to some extent. On the free space given to late the respondents write on if they think that there are other factors to affect their clear prescription writing, few of them emphasized the difficulty of some medicine names to spell. This implies that difficulty of some medicine names to spell is one of the factors that affect physicians to write legible prescription.
The other factor which was identified was absence of feedback to physicians from pharmacists on the writing problem of prescription. This implies that there is no communication between the physicians and pharmacists during work time (through tell phone) and meeting time.
This survey, as mentioned in the introduction, was intended to investigate the factors that affect proper prescription writing in Jimma University specialized hospital. In order to achieve the main objective, the following four research questions were formulated:
1. Do physicians have necessary knowledge on the impact of sloppy prescription writing?
2. Do physicians positively perceive the fact that prescriptions should be written clearly?
3. To what extent do physicians practice their legal responsibility when writing a prescription?
4. What are the other factors that affect proper prescription writing?
Data were collected from both physicians and pharmacists. In order to collect data from the sample, two instruments namely questionnaire and document analysis were used. To substantiate the data obtained through questionnaire, sample prescriptions were analyzed. The collected data were analyzed using both qualitative and quantitative methods of data analysis. The quantitative values were reported using percentage and mean value. Accordingly, the following are the findings of the survey:
1. The physicians have necessary knowledge on the negative impact of sloppy prescription writing.
2. They also seemed that they have positively perceived that prescription should be written clearly to avoid the
negative consequences of illegible prescription. However, the magnitude of practicing their legal requirements about prescription writing is low because:
a. Majority of the sample prescriptions (54.8%) were unclear
b. All physicians do not write their phone number on the prescription
c. Abbreviations dominating in their prescription
3. The main factors that impede their proper prescription writing, as identified in the discussion, are listed below.
a. Shortage of time (69%)
b. Difficulty of some medicine names to spell (80%)
c. Lack of feedback from pharmacists on the writing problem of prescription (52%)
The problem of practice
1. Physicians should improve the magnitude of proper prescription writing by doing the following things:
a. Write legible prescriptions to avoid misinterpretation which leads to medication error.
b. write full words than using abbreviation in prescription writing
c. use zero before decimal point to avoid misreading of a dose
d. write their names and phone number to help the pharmacists to call back for clarification
The problem of time
The university and the hospital administrative bodies in collaboration with ministry of health should find a way to increase the number of their human resource on this line to minimize burden of prescription writing per day because it is a serious issue.
Moreover, the physicians themselves can minimize the problem of time by considering the following points:
- Avoiding lost time
- Avoiding late starts and early finishes
- Handling routine procedures smoothly and quickly
Difficulty of some medicines’ name to spell
1. The concerned bodies ought to prepare some manual which contains some medicines names which are considered to be difficult to spell so that those who have spelling problem can study them.
2. Physicians should exert their efforts to know how each medicine name is spelt in advance.
Lack of feedback from pharmacists
First, the physicians themselves should be cooperative by writing their names and phone number on the prescriptions they write to help the pharmacists to call for clarification of unclear prescription which is on the other hand used as feedback for them.
Second, the university and the hospital administrative bodies should arrange a kind of forum on which both physicians and pharmacists meet to talk how they can make effective collaboration to benefit patients.
Finally, Ministry of health should give awareness creation on job trainings for the physicians on how and why to write proper prescription because it is one aspect of patient care.
The author has not declared any conflict of interests.
REFERENCES
|
Abdella SH, Wabe NT (2012). Prescriber's adherence to the basic principles of prescription orders. South West Ethiopia. Natl. J. Physiol. Pharm. Pharmacol. 2(1):66-70. Retrieved from
View
|
|
|
|
Cohen MR (2007). The Institute of Medicine report, preventing medication errors: Another good day. Am. J. Health Syst. Pharm, 64:S1-S2.
Crossref
|
|
|
|
|
Drug Administration and Control Authority of Ethiopia Contents January, 2010. Retrieved from
View
|
|
|
|
|
Good Prescribing Manual for Ethiopia (2011). Drug Administration and Control Authority of Ethiopia. Retrieved from apps.who.int › All › Medicine Access and Rational Use › Rational Use.
|
|
|
|
|
Kumar R (1996). Research Methodology. MewDeihi: SAGE Publications.
|
|
|
|
|
Majorie van Leijen Published Sunday, November 04, 2012.
|
|
|
|
|
Murray MD, Ritchey ME, Wu J, Tu W (2009). Effect of a pharmacist on adverse drug events and medication errors in outpatients with cardiovascular disease. Arch. Int. Med. 169:757-763.
Crossref
|
|
|
|
|
National handwriting day January 23. Prescription errors caused by sloppy handwriting. Retrieved from
View
|
|
|
|
|
Neville WG, Martin BE (2006). Medical Writing: Prescription for clarity. Cambridge:Cambridge University press).
|
|
|
|
|
Report from the National Academies of Science's Institute of Medicine (IOM), July 2006.
|
|
|
|
|
Teichman PG, Caffee AE (2002). Prescription writing to maximize patient safety. Fam Pract. Manag. 9:27-30.
|
|
|
|
|
Wikipedia, the free encyclopedia
|
|