Full Length Research Paper
ABSTRACT
The frequency and antibiotic resistance of N. gonorrhoeae are increasing worldwide. This study aimed to determine the prevalence of N. gonorrhoeae in genital swabs. A collaborative cross-sectional study was conducted by a team of Microbiologist, Dermato-Venerologist and Occupational Physician in Bangui, from January 2015 to December 2018. Genital samples were stained by the Gram method, grown on blood agar and the colonies identified according to the biochemical characteristics. Antibiotic sensitivity was determined by the agar diffusion method from disks. The prevalence of N. gonorrhoeae was 3.2%, more in males (90.5%), unschooled patients (61.1%), those with a history of STIs (56.8%), and female sex workers (p = 0.006) The strains of N. gonorrhoeae isolated were highly resistant to all antibiotics commonly prescribed in proportions from 60.9 to 95.8%. No resistance was observed to Ceftriaxone and Spectinomycin. This study highlights the interest of intensifying the prevention of N. gonorrhoeae infection in female sex workers, of the revision of the protocols of management of the N. gonorrhoeae infection and of a policy to ensure a better availability of new antibiotics selected. Understanding the mechanisms of resistance will be the subject of a characterization study in molecular biology.
Key words: N. gonorrhoeae, STI, prevalence, antibiotic resistance, female sex workers, Central African Republic, Africa.
INTRODUCTION
According to the World Health Organization (WHO), 30.6 million people were infected with N. gonorrhoeae in 2016. This number corresponds to a global prevalence of 0.9 and 0.7% respectively in women and men (Kirkcaldy et al., 2019; Rowley et al., 2019). Women in the WHO Africa region were the most affected (1.6%) while the combined prevalence among men and women aged 15-24 was 4.6% in South Africa and 8.2% in East Africa (Kirkcaldy et al., 2019; Torrone et al., 2018). The global incidence in 2016 was 20 per 1,000 women and 26 per 1,000 men, corresponding to 86.9 million new cases. The WHO African Region had the highest incidence (Kirkcaldy et al., 2019; Rowley et al., 2019). The trend is generally increasing in isolation of N. gonorrhoeae, which varies from one region to another depending on the diagnostic facilities (Kirby Institute, 2018; Choudhri, 2018). Gonococcal infection is usually asymptomatic in women (> 50%) unlike in men (10%). Complications of gonorrhea in women can be the cause of ectopic pregnancies and in both sexes of infertility (Unemo and Shafer, 2014). In addition, this high prevalence is associated by an increase in antibiotic resistance, with strains producing β-lactamases inactivating 3rd generation cephalosporins (C3G), the last resort for treatment of gonorrhea (WHO, 2016a). Thus, WHO has drawn worldwide attention to the risk of a therapeutic deadlock and the need to develop new drugs (Wi et al., 2017; Weston et al., 2017), especially in countries with limited resources, in sub-Saharan Africa. The Central African Republic (CAR) should not escape this reality because it is part of the Africa WHO region, the most affected. The probabilistic antibiotic therapy for N. gonorrhoeae infection in CAR is based on the use of ceftriaxone or/and Ciprofloxacin. However, the latest work on N. gonorrhoeae dates back to 1980. They already reported an increase in resistance to penicillins and the production of a β-lactamase (Georges et al., 1982). Thirty years later, these data require updating. In this context, this study aims to determine the prevalence and the antibiotic resistance of N. gonorrhoeae strains isolated from genital swab samples as well as the prevalence of sex workers among them at the National Reference Center of IST and Antiretroviral Therapy in Bangui.
METHODS
Study site
This is a cross-sectional study that took place at the National Reference Center of IST and Antiretroviral Therapy in Bangui, Central African Republic, from January 1, 2015 to December 31, 2018, that is a period of 4 years. The National Reference Center of IST and Antiretroviral Therapy is a public health establishment. It includes an Anonymous Screening Unit, Outpatient Treatment Service for HIV and tuberculosis, an STI care service and a medical analysis laboratory. The mission of the National Reference Center of IST and Antiretroviral Therapy in Bangui is to prevent STIs / HIV and provide comprehensive care for people living with STIs / HIV; as well as operational research. In order to promote access to care against STIs for female sex workers, an occupational doctor met in parallel with the female sex workers to make them aware of the systematic use of services and in particular to have access to prophylaxis of Accident of blood exposure of sexual origin (Corevih, 2019).
Study population
The population of our study consisted of patients referred to the National Reference Center of IST and Antiretroviral Therapy laboratory for sampling. Were included in this study, male or female patients, aged 15 years and over, with or without genital discharge, referred to the center's laboratory for a bacteriological study with culture of the urethral or vaginal sample. Any patient taking an antibiotic treatment or even having stopped the treatment less than 72 h before the sample was not included. The inclusion of patients was systematic in order to obtain a sufficient number of strains for the study of their resistance to antibiotics.
Data collection and bacterial analysis of genital samples
A standard data collection sheet containing socio-demographic and biological information (results of the culture and the antibiogram) made it possible to collect the data. N. gonorrhoeae has been the subject of a classical bacteriological diagnosis (Unemo and Shafer, 2014). Briefly, the vaginal and urethral samples were stained by the Gram method (Cypress Diagnostics, Hulshout, Belgium), inoculated on cooked and multivitamin blood agar made selective by the addition of vancomycin, colistin and nystatin (Cypress Diagnostics, Hulshout, Belgium). Bacterial identification using biochemical characters by API NH (BioMérieux, Marcy-l'Etoile, France) was completed by the study of antibiotic sensitivity using the agar diffusion method from antibiotic discs (Cypress Diagnostics, Hulshout, Belgium) according to the recommendations of the European Committee on Antimicrobial Susceptibility testing (EUCAST) for each study year (EUCAST, 2022).
Statistical analysis and ethical considerations
The data were entered and analyzed with Epi-Info version 7 software (WHO, Geneva & CDC, Atlanta). The general prevalence of N. gonorrhoeae was determined by relating the number of patients carrying N. gonorrhoeae to the number of total patients tested. Likewise, the prevalence of N. gonorrhoeae in the different groups was determined by relating the number of N. gonorrhoeae isolated in the group to the total number of N. gonorrhoeae isolated (95).

The prevalence of resistance to each antibiotic was determined by relating the number of strains resistant to this antibiotic to the total number of strains tested (95). Fisher's exact test, a parametric test obeying 2 conditions (random distribution of the sample and number in each group <5), was calculated, with online software BiostaTGV online statistic tests (https://biostatgv.sentiweb.fr/?module=tests/fisher), to compare the proportions of categories of qualitative variables with a significance level of 5%. The study received authorization from the Ethics and Scientific Committee of the Faculty of Health Sciences and the Pasteur Institute in Bangui.
RESULTS
During the study period, 3004 patients were received at the laboratory of the National Reference Center of IST and Antiretroviral Therapy for a bacteriological examination of the genital sample. The mean age of the patients was 29.7 years with extremes of 19 and 44 years. Women were more represented with 58.9% (1769); the sex ratio was 0.82. Among women, the female sex workers number was 197 (11.1%). Ninety-five (95) strains of N. gonorrhoeae were isolated by bacteriological examinations of genital samples; the prevalence was 3.2%. Among the 95 patients from whom N. gonorrhoeae was isolated, 86 or 90.5% were men and 9 women or 9.5%; the sex ratio (M / F) was 10.1. A history of STIs was noted in more than half of the cases, 56.8%. Unschooled patients predominated with 61.1%. N. gonorrhoeae was isolated from urethral and vaginal swabs in 90.5 and 9.5% respectively (Table 1). The evolution of the number of patients received at the laboratory for the analysis of genital samples is presented in Table 2 with an average of 751 patients and 3.2% isolation of N. gonorrhoeae per year. The patients were classified into different groups: men, women and female sex workers among women. These groups were compared according to Table 3. Among the 9 women, carriers of N. gonorrhoeae, 4 were female sex workers (4.2%) of the 3004 identified patients or 44.4% of the infected women. Comparison of female sex workers with other women showed that female sex workers were significantly more carriers of N. gonorrhoeae than other women (p = 0.006). On the other hand, there is no difference between the female sex workers and the rest of the participants of all sexes (Table 3). The antibiotics tested are those indicated for the antibiogram of N. gonorrhoeae according to the recommendations of the European Committee on Antimicrobial Susceptibility testing (EUCAST) for each study years (EUCAST, 2022). Regarding antibiotic resistance, the isolated N. gonorrhoeae strains showed a very high rate of resistance to commonly used antibiotics, 95.8% to nalidixic acid, 83.3% to chloramphenicol, 82.6% to penicillin G and 60.9% to ciprofloxacin. The rate of resistance to tetracycline is moderate (34.8%) and low for gentamycin (13.0%) and azythromycin (10.3%). No resistance was observed with ceftriaxone and spectinomycin (Figure 1).
DISCUSSION
This study aimed to determine the prevalence and resistance to antibiotics of N. gonorrhoeae strains isolated from samples of genital swabs as well as the prevalence of female sex workers among them at the National Reference Center for STIs and of Antiretroviral Therapy in Bangui. During the study period, 3,004 patients were received at the CNRISTTAR laboratory for a bacteriological analysis of the genital samples. Among them, there were 1769 women (58.9%) including 197 female sex workers (11.1%). The prevalence of N. gonorrhoeae was 3.2%. Men were in the majority (90.5%), like unschooled patients (Table 1). Female sex workers were significantly more carriers of N. gonorrhoeae than the other women and the rest of the participants, regardless of gender (Table 3).
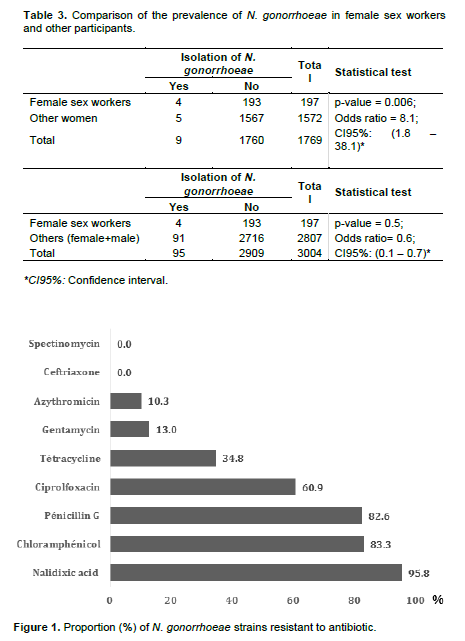
The vast majority of N. gonorrhoeae strains were resistant to nalidixic acid (95.8%), chloramphenicol (83.3%), Penicillin G (82.6%) and ciprofloxacin (60.9%). The rate of resistance was moderate to low, 34.8, 13.0 and 10.3%, respectively, to tetracycline, gentamycin and azythromycin.
In contrast, no strain was found to be resistant to ceftriaxone or spectinomycin (Figure 1). This study updates the data on N. gonorrhoeae in the CAR, the latest data were published on 1982, ie around thirty years. The prevalence of N. gonorrhoeae was 3.2%. This prevalence is higher than the global prevalence of 0.9 and 0.7% respectively among women and men (Kirkcaldy et al., 2019; Rowley et al., 2019) and that observed among women in Ndjamena in Chad (1.2%) (Compain, 2019). The prevalence of our series was lower than that of South Africa (4.6%) and East Africa (8.2%). These data from the CAR and other countries and regions show that the prevalence of N. gonorrhoeae varies from one country or even from one geographic region to another. In this study, the detection of N. gonorrhoeae was carried out by classical bacteriological examination with culture. The prevalence would therefore be underestimated because the trend is now to use nucleic acid amplification tests (Poncin and Bercot, 2019) as is the case in the studies by Compain, Kirkcaldy and Torrone (Compain et al., 2019; Kirkcaldy et al., 2019; Torrone et al., 2018), more sensitive than culture.
Strains of N. gonorrhoeae were variously distributed by sex. In fact, the majority of men were more affected (90.5%) than women (9.5%). These results confirm the fact that genital N. gonorrhoeae infection is noisier in men, leading them to seek health services, unlike women who are often carriers or even asymptomatic. The same observation was noted in France (Poncin and Bercot, 2019). However, WHO data indicates a higher prevalence among women than among men (Kirkcaldy et al., 2019; Rowley et al., 2019). The results of our study were obtained in patients referred to the laboratory. There is a high probability of detection of N. gonorrhoeae among them, particularly in men who were most often symptomatic. First, the great majority of women were pregnant, sent from the antenatal consultation, referred to the laboratory for prenatal analyzes, most often asymptomatic with theoretically a low probability of isolation of N. gonorrhoeae. On the other hand, the use of molecular tests can reveal N. gonorrhoeae even if the culture is negative. However, nucleic acid amplification tests were not used with our series, hence the low proportion of women with a sex ratio of 10.1.
Some women, female sex workers, were more carriers of N. gonorrhoeae than other women (p = 0.006). If the investigation of the determination of the behavior and the serological profile among female sex workers in Bangui identified 1,051 PS (CNLS, 2019) with 11.7% of VIH seroprevalence while it was not exhaustive, and that in our series female sex workers identified on a duration of 4 years were 197 but more carriers of N. gonorrhoeae than the other women, it is that the female sex workers would not frequent enough the National Reference Center of IST and Antiretroviral Therapy. Female sex workers are one key population for HIV (WHO, 2016b). HIV and N. gonorrhoeae are transmitted sexually. Priority prevention actions must be implemented for female sex workers to reduce the HIV seroprevalence and the N. gonorrhoeae prevalence too. This is why the female sex workers must be well sensitized and organized around care centers such as the National Reference Center of IST and Antiretroviral Therapy. This organization must involve Dermato-Venerologists and Occupational Safety and Health Doctors since the female sex workers activity is for a several number of women an income-generating activity allowing them to meet their needs (CNLS, 2019).
The high prevalence of N. gonorrhoeae, particularly among female sex workers in CAR is not the only problem encountered in the control of this bacterium in CAR. Our series results showed that the N. gonorrhoeae antimicrobial resistance is the second one. N. gonorrhoeae strains were highly resistant to nalidixic acid (95.8%), chloramphenicol (83.3%), penicillin G (82.6%) and ciprofloxacin (60.9%). These are the cheapest antibiotics, the most commonly used in Bangui, and inexpensive to cost. However, ciprofloxacin is one of the antibiotics recommended in CAR for the treatment of N. gonorrhoeae infection (DGLSIST, 2007). The cost of managing an N. gonorrhoeae infection would therefore increase. Only a study of the cost of care could confirm this hypothesis. This strong resistance is linked to self-medication which is a widespread practice in the CAR and especially to the free sale of drugs in the street. Shops called "Minipharma" that sell counterfeit drugs are legion in the streets of Bangui. An increase in resistance to penicillins and a strain producing β-lactamase have already been described in 1982 (Georges et al., 1982). If this trend continues, CAR would in a few years be in a therapeutic stalemate against N. gonorrhoeae. This trend of rapid and significant increase in resistance of N. gonorrhoeae has been observed in several countries on several continents (Martin et al., 2019; Unemo et al., 2016, Gasser et al., 2018). This is why the antibiotic resistance of N. gonorrhoeae has become worrying and the alert is raised for the development of other treatments (Bodie, 2019; Alirol, 2017). The rate of resistance was moderate against tetracycline (34.8%) and low for gentamycin (13.0%) and azthromycin (10.3%). With nearly 35% resistance, tetracycline could not even be prescribed as probabilistic antibiotic therapy because the treatment would only be effective against 2 out of 3 strains. Tetracycline must not be given to pregnant women. Azythromycin and gentamycin, although presenting a low rate of resistance, would hardly be effective. Gentamycin is not applicable in the treatment of N. gonorrhoeae infection because of the injectable route for the first and the cost for the other. These 2 antibiotics are therefore not indicated in current practice. The fact that no resistance has been observed with ceftriaxone and spectinomycin shows that these 2 molecules would be the antibiotics of choice for treating N. gonorrhoeae infection, this is the protocol in some countries (Pogany et al., 2015).
However, spectinomycin is hardly available in Bangui. The remedy therefore remains ceftriaxone, an antibiotic recommended in the treatment of N. gonorrhoeae infection in combination with ciprofloxacin in CAR. The most ceftriaxone advantage is the single dose in treatment of N. gonorrhoeae infection. The CAR should therefore revise its management protocol for N. gonorrhoeae infections by replacing ciprofloxacin with azythromycin or spectinomycin. A policy must be put in place to ensure good availability of these 2 antibiotics in all Central African Republic territory.
CONCLUSION
The prevalence of N gonorrhoeae was 3.2%; female sex workers were more carriers than the other women. The prevalence of resistance to common antibiotics was very high. These results suggest urgent reinforcement of prevention actions against the transmission of N gonorrhoeae to female sex workers, the revision of the protocols for the management of N gonorrhoeae infections and a policy to ensure the best availability of the antibiotics indicated in the new therapeutic protocols.
CONFLICT OF INTERESTS
The authors have not declared any conflict of interest.
REFERENCES
|
Alirol E, Wi TE, Bala M, Bazzo ML, Chen XS, Deal C, Dillon JAR, Kularatne R, Huijsduijnen J, Hook EW, Lahra MM, Lewis DA, Ndowa F, Shafer WM, Tayler L, Workowski K, Unemo M, Balasegaram M (2017). Multidrug-resistant gonorrhea: A research and development roadmap to discover new medicines. PLoS Medicine 14(7):e1002366. |
|
|
Bodie M, Gale-Rowe M, Alexandre S, Auguste U, Tomas K, I Martin (2019). Considérations portant sur les taux croissants de gonorrhée et de gonorrhée résistante aux médicaments: il n'y a pas de temps à perdre. Relevé des Maladies Transmissibles au Canada. 45(2/3):58-67. |
|
|
Choudhri Y, Miller J, Sandu J, Leon A, Aho J (2018). Gonorrhea in Canada, 2010-2015. Canadian Communicable Diseases Report 44(2):37-42. |
|
|
Compain F, Nodjikouambaye ZA, Sadjoli D, Moussa MA, Adawaye C, Mboumba Bouassa RS, Koyalta D, Tonen Wolyec S, Péré H, Podglajen I and Bélec L (2019). Low prevalence of common sexually transmitted infections contrasting with high prevalence of mycoplasma asymptomatic genital carriage: a community-based cross-sectional survey in adult women living in N'djamena, chad. The Open Microbiology Journal 13:222-229. |
|
|
Coordination Nationale du Comité National de Lutte contre le Sida de la République Centrafricaine (CN/CNLS) (2019). Rapport de l'enquête de la détermination du comportement et du profil sérologique chez des professionnelles du sexe à Bangui, Boali, Bouar, Carnot et Berbérati en République Centrafricaine. CN/CNLS, Bangui, République Centrafricaine. pp 81. |
|
|
Corevih (2019). Guide de prise en charge des accidents d'exposition sexuelle et au sang: Document destiné aux établissements de santé de la région Bourgogne-Franche-Comté. Bourgogne, France, 34p. |
|
|
Direction Générale de la Lutte contre le Sida et les Infections Sexuellement Transmissible de la RCA (DGLSIST) (2007). Rapport sur les Infections Sexuellement Transmissibles. Ministère de la Santé Publique de la Population et de la Lutte contre le Sida, Bangui, République Centrafricaine P 54. |
|
|
European Committee on Antimicrobial Suscpetibility Testing (EUCAST) (2022). Antimicrobial susceptibility testing. |
|
|
Gasser M, Schrenzel J, Kronenberg A, pour le Centre suisse pour le contrôle de l'Antibiorésistance. (2018). Evolution actuelle des résistances aux antibiotiques en Suisse. Swiss Medical Forum 18(46):943-949. |
|
|
Georges AJ, Georges MC, Saluzzo JF, Gonzales JP, Martin, PMV, Guibourdenche M, Riou JY (1982). Auxotypes et sensibilité à 5 antibiotiques des souches de N. gonorrhoeae isolées en RCA en 1980 et 1981. Bulletin de la Société de Pathologie Exotique 75:352-359. |
|
|
Kirby Institute (2018). HIV, viral hepatitis and sexually transmissible infections in Australia: annual surveillance report 2018. Kirby Institute, UNSW Sydney, Sydney, Australia P 208. |
|
|
Kirkcaldy RD, Weston E, Segurado AC, Hughes G (2019). Epidemiology of Gonorrhea: A Global Perspective. Sexual Health. 16(5):401-411. |
|
|
Martin I, Sawatzky P, Allen V, Lefebvre B, Hoang LM , Naidu P, Minion J, Van Caeseele P, Haldane D, Gad RR, Zahariadis G, Corriveau A, German G, Tomas K, Mulvey MR (2019). Neisseria gonorrhoeae, bactérie multirésistante et ultrarésistante, Canada, de 2012 à 2016. Relevé des Maladies Transmissibles au Canada 45(2/3):48-57. |
|
|
Pogany L, Romanowski B, Robinson J, Gale-Rowe M, Latham-Carmanico C, Weir C, Wong T (2015). Prise en charge de l'infection gonococcique chez les adultes et les jeunes Nouvelles recommandations. Canadian Family Physician 61:e451-e456. |
|
|
Poncin T, Bercot B (2019). Le gonocoque: le point en 2018. Revue de Biologie Médicale 347:1-13. |
|
|
Rowley J, Vander Hoom S, Korenromp S, Low N, Unemo M, Abu-Raddad LJ, Chico RM, Smolak A, Newman L, Gottlieb S, Thwin SS, Broutet N, Taylor MM (2019). Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bulletin of the World Health Organization 97(8):548-562. |
|
|
Torrone EA, Morrison CS, Chen PL, Kwok C, Francis SC, Hayes RJ, Looker KJ, McCormack S, McGrath N, van de Wijgert JHHM, Watson-Jones D, Low N, Gottlieb SL, STIMA Working Group (2018). Prevalence of sexually transmitted infections and bacterial vaginosis among women in sub-Saharan Africa: An individual participant data meta-analysis of 18 HIV prevention studies. PLoS Medicine 15(2):e1002511. |
|
|
Unemo M, del Rio C, Shafer WM (2016). Antimicrobial resistance expressed by Neisseria gonorrhoeae: a major global public health problem in the 21st century. Microbiology spectrum 4(3):4-3. |
|
|
Unemo M, Shafer WM (2014). Antimicrobial Resistance in Neisseria gonorrhoeae in the 21st Century: Past, Evolution, and Future. Clinical Microbiology Reviews 27(3):587-613. |
|
|
Weston EJ, Wi T, Papp J (2017). Surveillance for antimicrobial drug-resistant neisseria gonorrhoeae through the enhanced gonococcal antimicrobial surveillance program. Emerging Infectious Diseases 23(Suppl):S47-S52. |
|
|
Wi T, M Lahra MM, Ndowa F, Bala M, Dillon JAR, Ramon-Pardo PR, Eremin SR, Bolan G, Unemo M (2017). Antimicrobial resistance in Neisseria gonorrhoeae: Global surveillance and a call for international collaborative action. PLoS Medicine 14(7):e1002344. |
|
|
World Health Organization (WHO) (2016a). Guidelines for the treatment of Neisseria gonorrhoeae. WHO, Geneva, Switzerland. P 55. |
|
|
World Health Organization (WHO) (2016b). Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. WHO, Geneva, Switzerland, P 155. |
|
Copyright © 2024 Author(s) retain the copyright of this article.
This article is published under the terms of the Creative Commons Attribution License 4.0