ABSTRACT
Coronary atherosclerosis still represents one of the main causes of death. Efficacious prevention should focus on early control of cardiovascular risk factors, including lipid profiles, which unable detect on sub-clinical cases. High-sensitive C-reactive protein (hs-CRP) can prove to be an early cardiac risk predictor. Aims of this study were to compare hs-CRP levels between healthy volunteer with normal blood pressure and those with prehypertension, and to use hs-CRP levels along with other risks to be a cardiac risk predictor. Cross sectional study was done for 6 months duration from January to June 2013 at Kudjab Hospital located in Udonthani province, Thailand. Forty (40) healthy volunteers with pre-hypertension and other 40 volunteers with normal blood pressure were joined in this study. Both groups were similar in the age range and sex. Twelve-hour fasting blood samples were collected from all the participants. Serum was assayed for hs-CRP and lipid profile. All the parameters were statistically significant difference (P<0.001). hs-CRP levels (6.27±7.8 mg/l) was elevated among prehypertension. Odd ratio of hs-CRP for pre-hypertension was 15.45, whereas odd ratio of lipid profiles for prehypertension prediction was only 1.69. However, hs-CRP and lipid profiles were significance related to prehypertension (P<0.001). hs-CRP is early cardiac risk predictor even with normal lipid profile and can help measure additional risk especially subclinical people such as prehypertension.
Key words: Cardiovascular diseases, high-sensitive C-reactive protein (hs-CRP), prehypertension, lipid profile.
The study in Thailand showed that the death rate from heart disease and coronary artery disease is in the top three of fatal diseases. There are about 20 million people who have heart disease and coronary artery subclinical people that need permanent treatment with high cost (Nakapong and Meerit, 2006). In general, pathological lesion of coronary artery disease is that cholesterol accumulates in the artery walls causing atherosclerosis. High-sensitive C-reactive protein (hs-CRP), an acute phase reactant protein is a proinflammatory atherogenic circulating marker which can prove to be an early cardiac risk predictor (Corrado and Novo, 2005). According to epidemiology data, hs-CRP can predict coronary artery diseases. The Adult Treatment Panel III Guidelines, the National Cholesterol Education Program suggests and that the use of level of hs-CRP and fibrinogen together with general biochemical substance check can be used as a risk indicator (Pearson et al., 2003).
Hs-CRP is more accurate value because its normal range gives better interpretation especially for prediction of atherosclerosis and artery disease. As hs-CRP can measure CRP value as low as 0.3 mg/L so, it is useful to evaluate and indicate the risk of atherosclerosis. CDC/AHA statement suggested that when CRP < 1 mg/L low cardiovascular risk; 1 to 3 mg/L intermediate (average) cardiovascular risk; > 3 mg/L high cardiovascular risk and if > 10 mg/L, the infected part or the acute coronary syndrome should be detected (Pearson et al., 2003). In the high cardiovascular risk group, the risk becomes twice compared to the low cardiovascular risk group. Individual with high hs-CRP at the highest point of a normal range will have a higher risk to 1.5-4 times of getting heart attack compared with those with lower hs-CRP at the lowest point of a normal range (Ridker, 2003; Ridker, 1998).
The researchers were interested to: 1) compare hs-CRP levels between healthy volunteer with normal blood pressure and those with prehypertension, and 2) use hs-CRP levels along with other risk including body mass index (BMI) and lipid profiles to be a cardiac risk predictor.
Subject
Cross sectional study for 6 months duration from January to June 2013 at Kudjab Hospital located in Udonthani province, Thailand. 80 samples in this study included 40 healthy volunteers with pre-hypertension and other 40 volunteers with normal blood pressure, which were similar in the age range (20-40 years) and sex (male = 20, female = 20). The research program had to pass the approval of the hospital directors and the Board of Human Research Ethics Committees of the hospital and all subjects gave written consent. The healthy volunteers were normal vital signs and normal physical examination as inclusion criteria. The exclusion criteria included drug use, recent surgery, pregnancy, smoking, drinking, exercise before blood penetration, and blood borne infection such as hepatitis B or C, AIDS and syphilis (Horowitz, 2008). Prehypertension group was the same criteria as the healthy volunteers, except, there had blood pressure values between 120> to <139 mmHg of systolic blood pressure (SBP) and between >80 to <89 mmHg of diastolic blood pressure (DBP) were defined as prehypertension according to the Prehypertension; Joint National Commission 7 criteria (Chobanian et al., 2003). Each blood pressure measurement was done at resting blood pressure (after 5 min resting 2 times). This research project had been approved by Ethical Human Research Committee of Kudjab Hospital, Thailand. The specimens must be clearly labeled with name, surname, age, sex, height, weight, and collection date on the blood collecting tubes.
Specimen preparation and biochemical assays
Twelve-hour fasting 6 ml blood samples were collected from each of the participants. Serum was assayed for hs-CRP and lipid profile by COBAS INTEGRA® 400 plus (Roche-diagnostics, Switzerland). 3 ml blood sample was separated for serum preparation to analyze for hs-CRP, total cholesterol, triglyceride, LDL- cholesterol and HDL-cholesterol. The experiment serum centrifugation (3,000 rpm/5 min) was done by analyzing the separated sample with automatic COBAS INTEGRA® 400 plus (Roche-diagnostics, Switzerland). The measurement of hs-CRP was based on immunonephelometry or turbidimetry by using monoclonal antibody specified to CRP binding with the CRP in serum creating agglutination and the sediment of the solution. The sediment of the solution was directly related with the CRP amount compared with standard samples in mg/L. The test of total cholesterol, triglyceride, LDL- cholesterol and HDL-cholesterol by using the principle of absorbance photometry shown in COBAS INTEGRA® 400 plus can be analyzed together with controlled materials according to low or high level by the manufacturer’s method.
Data analysis
Age, BMI, hs-CRP and lipid profiles were reported in mean and standard deviation. The comparison between the healthy group and the prehypertension group was done by hs-CRP level together with the lipid profile with unpaired t-test at the statistic significant level, P < 0.05. The relationship of between hs-CRP and prehypertension, and lipid profiles and prehypertension were analyzed by using Pearson Chi-square. All statistic analyses were analyzed through SPSS computer program version 11.0 (SPSS, Chicago, IL). The calculation of odds ratio of hs-CRP and lipid profiles for prehypertension was calculated by the following formula:
Odd Ratio = [a/(a+b)]/[b/(a+b)]/[c/(c+d)]/[d/(c+d)].
a = number of normal parameter and normal blood pressure.
b = number of normal parameter with prehypertension.
c = number of abnormal parameter and normal blood pressure.
d = number of abnormal parameter with prehypertension.
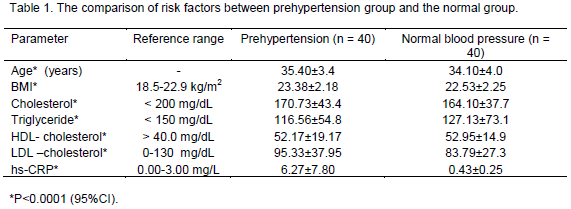
The study of risk factors of prehypertension group to compare with the normal blood pressure group of the same number (N = 40), was showed that there was a significant difference (P<0.0001) as shown in Table 1. The mean of hs-CRP in prehypertension had higher than the normal range (CRP>3 mg/L), while the mean of hs-CRP in normal blood pressure group or control was within normal range (0.00 to 3.00 mg/L).
When separating the prehypertension group from the normal group, hs-CRP value in the normal range (hs-CRP³3 mg/L) and the abnormal (hs-CRP >3 mg/L), it was found that hs-CRP can be used to indicate the risk of heart disease and coronary artery disease by calculating odds ratio at 15.45 (Table 2). However, when separating the prehypertension group from the normal group by cut-off with reference range (cholesterol <200 mg/dl, Triglyceride <150 mg/dl, HDL- cholesterol >40.0 mg/dl, LDL –cholesterol 0.0 -130.0 mg/dl) and dyslipidemia (out of reference range), it was found that some healthy people had abnormal lipid profile due to lower HDL cholesterol. When using lipid profile value to indicate the risk of heart disease and coronary artery disease of prehypertension group, the result was lower odds ratio = 1.69 (Table 3). However, relation of hs-CRP and lipid profiles to prehypertension was still statically significance at P<0.001.
We investigated hs-CRP level of the prehypertension and control groups to compare the level of hs-CRP, lipid profile, and other risk factors such as age and BMI. All parameters of both groups were a statistically significant difference (P<0.0001), however, almost all were still in reference ranges except the BMI and hs-CRP level, which was out of reference range in prehypertensions. It can be concluded that lipid profile and other risk factors cannot detect sub-clinic occurrence, such as, prehypertension. However, hs-CRP level can be determined prehypertension rather than lipid profiles (odds ratio = 15.45 and1.69, respectively).
The previous study (Rogowski et al., 2007) was reported that hs-CRP of healthy people (n = 6,588) was averagely low (0.16 mg/L) also other risk factors such as lipid profile, systemic inflammation (by using erythrocyte sedimentation rate, ESR), white blood cell count, and fibrinogen level decrease, impaired aortic elasticity of the prehypertension with the same age group (33 to 35) and revealed that hs-CRP of prehypertension with impaired arterial stiffness were higher (Celik et al., 2011) which was similar to this study.
It can be concluded that people with prehypertension tend to have less aortic elasticity but with higher hs-CRP value. The children and teenage group (6 to 18 years old) with obesity status defined from decreasing of HDL-cholesterol, increasing of triglyceride, hypertension, and impaired glucose metabolism (prediabetes) or at least 2 aspects showed that the average hs-CRP was higher than normal (average normal = 3.8 mg/l, 95% CI: 2.8 to 4.8) as well (Soriano-Guillén et al., 2008). Moreover, hs-CRP can be used to follow up the treatment and self-caring of diabetes type 2 (insulin independent diabetic mellitus, IIDM) who tend to suffer from complications of heart disease and coronary artery disease with normal lipid profile (Asegaonkar et al., 2011).
In this study, the increase of BMI was also found in prehypertension (BMI = 23 to 24.9 kg/m2 for Thai people). In the overweight people, there is an increase of adipose tissue and abnormal protein with hormone characteristics causing infection of systemic inflammation type affecting metabolic pathway in several processes such as dysglycemia or clinically called prediabetic; impaired fasting glucose, IFG; impaired glucose tolerance, IGT and abnormal blood pressure control, that is, prehypertension (Moreno-Aliaga et al., 2005; Fantuzzi, 2005; Vettor et al., 2005; Xu et al., 2003). Moreover, the increase of systemic inflammation can cause abnormal circadian blood pressure and resulting in endothelial dysfunction. If the disorder retains for a long time, it will result in heart disease and coronary artery disease (Kougias et al., 2005). hs-CRP, a golden inflammatory marker has been proposed to be a more sensitive predictor of CHD events than LDL itself (Pu et al., 2006).
It is a surrogate marker of subclinical inflammation which represents a state of chronic low-grade inflammation of arterial wall. hs-CRP is not only an inflammatory but also a proatherogenic pentameric protein as it directly and actively participates in atherogenesis (Armani and Becker, 2005). During recent years, the importance of hs-CRP and its estimation in the laboratory have been dramatically changed. Individuals with LDL <100 mg% and hs-CRP level >3 mg% represent a high-risk group often missed in clinical practice. The addition of hs-CRP to standard lipid profile evaluation may provide a simple and inexpensive method for improving global risk prediction (Ridker, 2003). It can be said that hs-CRP (normal value = 0.0-0.3 mg/L) in blood can indicate systemic inflammation and the risk of heart disease and coronary artery disease. In this study, it may include hs-CRP with other biochemical tests such as glucose, HbA1C, lipid profile for more sensitivity diagnose for subclinical group such as prehypertension and may also prediabetes. Further study need to be conducted to detect hs-CRP along with other blood parameter such as, fasting blood sugar and HbA1C to see the relation between hs-CRP and prediabetes and as a marker to prevent diabetic mellitus in subclinical group. Also, hs-CRP detection should be done with biochemical parameters in large population to make sure that hs-CRP can be used for evaluating the risk of subclinical group and can be use in massive control.
The hs-CRP was more preferable to evaluate the risk of subclinical appearance such as, prehypertension. The use of hs-CRP along with lipid profile detection can enable early detection of the risk of heart and coronary artery diseases with more effective data to medical consultant for changing of dietary intake and increased physical activities especially in subclinical group. hs-CRP detection can be done in large population for massive control to give the public policy on self-caring such as weight control, diet control and exercise.
The authors have not declared any conflict of interests.
The author is grateful to Suan Sunandha Rajabhat University, Bangkok, Thailand for grant support. We would like to sincerely thank all staff of Clinical Chemistry Laboratory Section, Division of Pathology, Kudjab Hospital located in Udonthani province, Thailand for a research laboratory facility and all volunteers for providing useful data on this research.
REFERENCES
Armani A, Becker RC (2005). The biology, utilization, and attenuation of C-reactive protein in cardiovascular disease: Part II. Am. Heart J. 149(6):977-983.
Crossref |
|
|
Asegaonkar SB, Marathe A, Tekade ML, Cherekar L, Bavikar J, Bardapurkar J, Ajay R (2011). High-sensitivity C-reactive protein: a novel cardiovascular risk predictor in type 2 diabetics with normal lipid profile. J. Diab. Complication 25(6):368-370.
Crossref |
|
|
Celik T, Yuksel UC, Demirkol S, Bugan B, Iyisoy A, Kabul HK, Kilic S, Fici F, Yaman H (2011). Relationship between increased systemic inflammation and impaired aortic elasticity in young patients with prehypertension. Blood Press. Monit. 16(2):55-61.
Crossref |
|
|
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ (2003). National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National High Blood Pressure Education Program Coordinating Committee: The Seventh Report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA 289(19):2560-2572.
Crossref |
|
|
|
Corrado E, Novo S (2005). Role of inflammation and infection in vascular disease. Acta Chir. Belg. 105(6):567-579. |
|
|
Fantuzzi G (2005). Adipose tissue, adipokines, and inflammation. J. Allergy Clin. Immunol. 115(5):911-919.
Crossref |
|
|
|
Horowitz LG (2008). Reference intervals: practical aspects. Electronic J. Int. Fed. Clin. Chem. Lab. Med. 19(2):1-11. |
|
|
Kougias P, Chai H, Lin PH, Yao Q, Lumsden AB, Chen C (2005). Effects of adipocyte-derived cytokines on endothelial functions: implication of vascular disease. J. Surg. Res. 126(1):121-129.
Crossref |
|
|
|
Moreno-Aliaga MJ, Campion J, Milagro FI, Berjon A, Martinez JA (2005). Adiposity and proinflammatory state: The chicken or the egg. Adipocytes 1:1-16. |
|
|
|
Nakapong R, Meerit S (2006). Cardiovascular diseases report in 2006. Department of Disease Control, Ministry of Public Health, Thailand. |
|
|
Pearson TA, Mensah GA, Alexander, RW Anderson JL, Cannon RO 3rd, Criqui M, Fadl YY, Fortmann SP, Hong Y, Myers GL, Rifai N, Smith SC Jr, Taubert K, Tracy RP, Vinicor F (2003). Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 107(3):499-511.
Crossref |
|
|
Pu LJ, Lu L, Xu XW, Zhang RY, Zhang Q, Zhang JS, Hu J, Yang ZK, Ding FH, Chen QJ, Lou S, Shen J, Fang DH, Shen WF (2006). Value of serum glycated albumin & high-sensitivity C-reactive protein levels in the prediction of presence of coronary artery disease in patients with type 2 diabetes. Cardiovasc. Diabetol. 5:27.
Crossref |
|
|
Ridker PM (1998). Inflammation, infection, and cardiovascular risk: How good is the clinical evidence? Circulation 97(17):1671-1674.
Crossref |
|
|
Ridker PM (2003). Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 107(3):363-369.
Crossref |
|
|
Rogowski O, Shapira I, Toker S, Melamed S, Shirom A, Zeltser D, Berliner S (2007). Very low C-reactive protein in apparently healthy individuals: Physiological status or just a reflection of an improved health profile. Biomarkers 12(6):645-656.
Crossref |
|
|
Soriano-Guillén L, Hernández-García B, Pita J, Domínguez-Garrido N, Del Río-Camacho G, Rovira A (2008). High-sensitivity C-reactive protein is a good marker of cardiovascular risk in obese children and adolescents. Eur. J. Endocrinol. 159(1):R1-4.
Crossref |
|
|
Vettor R, Milan G, Rossato M, Federspil G (2005). Adipocytokines and insulin resistance. Aliment. Pharmacol. Ther. 22(Suppl 2):3-10.
Crossref |
|
|
Xu H, Barnes GT, Yang Q, Tang G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H (2003). Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J. Clin. Invest. 112(12):1821-1830.
Crossref |